Indexing & Abstracting
Full Text
Original ArticleDOI Number : 10.36811/rjnnd.2021.110004Article Views : 88Article Downloads : 47
Normal pressure hydrocephalus. Results of shunting correlated with diagnostic tests in 55 patients
Fares Laouar*, Manel Bensama, Ridha Rabia and Lotfi Boublata
Department of Neurosurgery, Benbadis University Hospital Centre, Benseghir Abdelouahab Street, 25000 Constantine. Algeria
*Corresponding Author: Fares Laouar, Department of Neurosurgery, Benbadis University Hospital Centre, Benseghir Abdelouahab Street, 25000 Constantine. Algeria, Phone number: +213662385306, +213794194974; Email: laouarfares@hotmail.com; fares.laouar@univ-constantine3.dz
Article Information
Aritcle Type: Original Article
Citation: Fares Laouar, Manel Bensama, Ridha Rabia, Lotfi Boublata. 2021. Normal pressure hydrocephalus. Results of shunting correlated with diagnostic tests in 55 patients. Res J Neuro N Disord. 1: 01-09.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2021; Fares Laouar
Publication history:
Received date: 24 September, 2021Accepted date: 29 September, 2021
Published date: 01 October, 2021
Abstract
Object: The purpose of this study was to evaluate the efficacy of ventricular shunting in normal pressure hydrocephalus (NPH).
Methods: The authors retrospectively studied outcomes in NPH patients in whom shunts were implanted. At follow-up examinations up to one year, clinical symptoms were recorded according to a new NPH outcome rating scale, the modified Rankin score and the Mini-Mental State Examination. Comorbidities and complications during this period were also analyzed.
Results: A total of 55 patients with NPH were included, with a male predominance (69% of men), an average age of 70 years. Comorbidities are multiple, hypertension is the most common factor in 55% of cases. 76% of patients are classified as having idiopathic NPH. The CSF tap test allows the evacuation of at least 40 ml of CSF and RCSF measurements in 55 patients. All these patients received a shunt withe programmable valve. An improvement in gait was observed in 88% of patients, 91% in balance and 84% in continence. The improvement in the field of neuropsychology is 34% after one year of shunt. 87% of patients were improved according to mRS. 27% of patients had complications and were treated conservatively or surgically.
Conclusions: Ventricular shunt implantation is a safe procedure and can improve symptoms in 98% of patients with NPH in the medium term.
Keywords: Cerebrospinal fluid (CSF) tap test; Normal pressure hydrocephalus (NPH); NPH assessment scores; Programmable valve; Symptomatic triade of Hakim
Introduction
Normal pressure hydrocephalus (NPH), sometimes referred to as chronic adult hydrocephalus, is a chronic neurological condition characterized by dilatation of the ventricular cavities associated with symptoms based on the clinical trial of gait disturbance, cognitive impairment and sphincter disorders [1]. This anatomo-clinical entity was first described by Hakim and Adams (1965) [2,3]. Since then, it has been accepted that the definition of NPH in adults is based on the association of suggestive clinical signs and brain imaging whose characteristics are compatible with this hypothesis. This is associated with an intracranial pressure considered normal or slightly increased [4]. The clinical picture included a symptomatic triad which has now become classic, composed of a gait disorder (postural instability, "slippery" steps, rigidity, astasia-abasia...), cognitive disorders (subcortico-frontal profile with especially attentional disorders, slowing down, apathy, dysexecutive syndrome) or even emotional (irritability, emotional instability) and urinary disorders (urinary urgency, nocturnal pollakiuria), which varies in intensity and in their components according to the patients [1]. The clinical symptoms of NPH can be improved by cerebrospinal fluid (CSF) drainage, which is obtained temporarily by lumbar puncture (LP) or external lumbar drainage, or permanently by placing a ventricular shunt. The objective of this article is to present the results obtained one year after shunt surgery of the patients with NPH using a new NPH outcome rating scale, the modified Rankin score (mRS) and the Mini-Mental State Examination (MMSE) as outcome measures.
Patients and Methods
Study methods:
This is a retrospective cross-sectional study of 55 cases of normal pressure hydrocephalus (NPH), collected at the Neurosurgery department of CHU Benbadis Hospital in Constantine, over a period from September 2016 until February 2020. This is an adult population (over 50 years of age), the inclusion criteria for the study were clinical symptoms and radiological findings compatible with NPH [4]: Presence of at least two of the components of the classic triad of Hakim and Adams meeting the definition of NPH and a magnetic resonance imaging (MRI) will confirm communicating hydrocephalus. The first admission of the patient to the Day Hospital will allow us to collect several epidemiological and anamnestic data (age, sex, risk factors, and duration of symptoms). The initial clinical and neurological examination based on numerous gait characteristics: the ability to walk in tandem and half-lap 3 meter round trip, the number of steps and the time required to walk a distance of 10 meter in free walking. Impairment on gait and balance was assessed using a scale designed for NPH. Mental disorders were assessed by the Mini-Mental State Examination (MMSE) [5]. Bladder disfunctions were assessed in the same way as walking. MRI was examined for ventricular dilatation with an Evans index (EI)>0.3.
At the end of the clinical examination, a high-volume lumbar puncture (HVLP) or CSF tap test was performed as described by Wikkelso et al [6] in the left lateral decubitus position, which allows the evacuation of a quantity of CSF>40 ml at least, with the possibility to measure the lumbar pressure coupled with a study of the resistance to CSF outflow (RCSF) by means of the perfusion technique via the lumbar space (the lumbar infusion test) [7]. The pressure measured by LP should be between 4 and 18 mmHg, so the CSF outflow resistance is high when RCSF > 13 mmHg/ml/min. 24 hours after CSF tap test, patients will be re-examined for each symptom. The gait assessment scale established on the day of hospitalization and after the 24 H lumbar puncture procedure were compared. Patients will be readmitted for ventriculoperitoneal or atrial shunt surgery if they had responded positively to CSF tap test. All patients will be treated with the same ventriculoperitoneal shunt model with an adjustable pressure valve.
Postoperative evaluation report:
The evaluation reporting on the same parameters of walking, posture, cognitive ability and sphincter disorders. Patients will benefit from a regular clinical and radiological follow-up allowing a short- and medium-term postoperative evaluation: at 1,3,6 and 12 months after the shunt surgery (including video evaluation of the gait). In addition to the examinations described above, patients were assessed at entry and 12 months after surgery using the modified Rankin Scale (mRS) [8,9] and a new specific scale designed for NPH [10]. The total score on the NPH scale is the mean score of assessments in four domains: gait, balance, and continence. Score in the gait domain in turn represents the mean of converted scores on three separate assessments/tasks, whereas the balance and continence domains are covered by ordinal scales.
The total score, the domain scores, and the scores on within-domain assessments/tasks all have a min–max range from 0 to 100, where 100 represent normal performance among healthy individuals in an NPH typical age range of 70-74 years [10]. Improvement was defined as follows: an increase of 1 step or more in the mRS and an increase of 5 points or more in the NPH scale.
Results
Epidemiological data:
NPH represents 2% of the total operative activity in our department and 14% compared to other types of adult hydrocephalus. There were 55 patients in our study population, comprising 69% men and 31% women. The mean age was 70 ± 9.3 years (extremes 50 and 85 years). 55% of patients have hypertension, which is the most frequent risk factor in our series, followed by diabetes and dyslipidemia (Table. 1), a single risk factor in 40%, only 5% combine 5 risk factors.
The delay between the first clinical manifestations and the discovery of the disease is often long > 1 year. In the study group, 64% (35/55) of patients have manifested the complete clinical triad, with gait disturbance which appears first in 82% of cases, then incontinence followed by memory disturbances.
The Difficulty in walking was present in 100% of the patients, 71% with memory disorders, most often with a mild cognitive deficit, and 91% with incontinence. 76% of our patients are classified as having idiopathic or primary iNPH, i.e. without any known cause, the remaining 24% are secondary sNPH, i.e. after a head trauma (44%), a stroke (31%), and a history of meningitis at childhood (in 25% of cases).
|
Table 1: Distribution of comorbidities and risk factors |
||
|
Comorbidities |
Number |
Percentage |
|
Arterial hypertension |
30 |
55% |
|
Diabetes |
18 |
33% |
|
Dyslipidemia |
17 |
31% |
|
Tobacco |
12 |
22% |
|
Benign prostatic hypertrophy (BPH) |
11 |
20% |
|
Head trauma |
8 |
15% |
|
Heart disease |
7 |
13% |
|
Stroke |
5 |
9% |
|
Meningitis |
4 |
7% |
|
Peripheral vasculopathy |
4 |
7% |
|
Lumber spinal stenosis |
2 |
4% |
|
Alzheimer's disease |
1 |
2% |
|
No history |
5 |
9% |
Result of clinical scores after CSF tap test:
The decision for shunt surgery was based on our results from the CSF tap test. Therefore, in this patient population improvement is observed in 60% on the total NPH scale (Figure 1), this rate is reduced by the lack of immediate improvement of continence after CSF tap test (for domains: table. 2).

Figure 1: Changes in total score for 55 patients with normal pressure hydrocephalus after SCF tap test.
|
Table 2: The improvement of total and domain scores on the normal pressure hydrocephalus (NPH) scale of the included patients with NPH after CSF tap test and 12 months after surgery. |
||
|
Improvement % Scores |
After CSF tap test |
12 months after surgery |
|
Tandem walking |
56% |
98% |
|
Number of steps |
34% |
89% |
|
Timed 10-meter walk test |
48% |
77% |
|
Balance |
42% |
91% |
|
Continence |
4% |
84% |
|
Total NPH scale |
60% |
98% |
Therapeutic data:
All 55 operated patients benefited from ventricular shunts, 35 VP and 20 VA shunts, with a programmable valve from Sophysa (Sophy®). The value of the optimal opening pressure found in our study in the majority of our patients is 140 mmH2O (whatever the type of shunt). After 12 months, 98% of the patients had improved by more than 5 points on the total NPH scale (for the domains: Table. 2). Improvement of gait was observed in 88% of patients, slightly less than in balance (91%) and better than continence (84%). The improvement in symptoms is maintained throughout the follow-up period up to one year postoperatively (Figure 2).
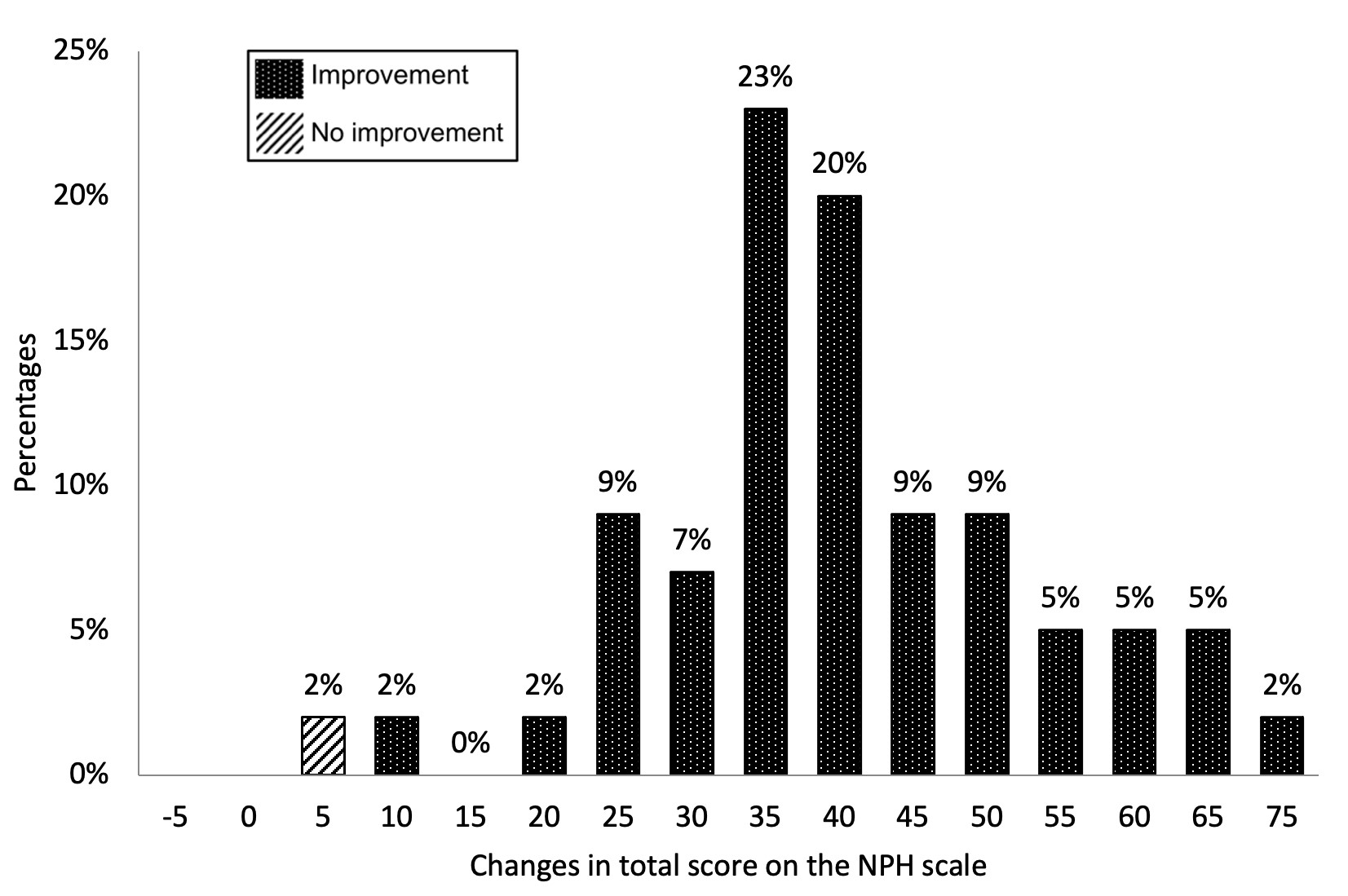
Figure 2: Changes in total score for 48 patients with normal pressure hydrocephalus after 1 year of shunt treatment.
The improvement in the field of neuropsychology is 34% after one year of the shunt, 36% of the patients have a normal mental state and 27% the deficit is mild. The severe and very severe deficit of dementia does not change after one year of shunt surgery. 87% of the 55 patients who could be evaluated 12 months after surgery had an improvement in mRS. 25% of patients were improved by one step, 44% by two steps, 12% by three steps, and 4% by four steps. The proportion of patients able to live independently (scores 0-2 on the mRS) was increased from 25% before surgery to 44% 12 months after. The distribution of changes measured by the NPH scale showed a similar pattern as the mRS changes (Figure 3).
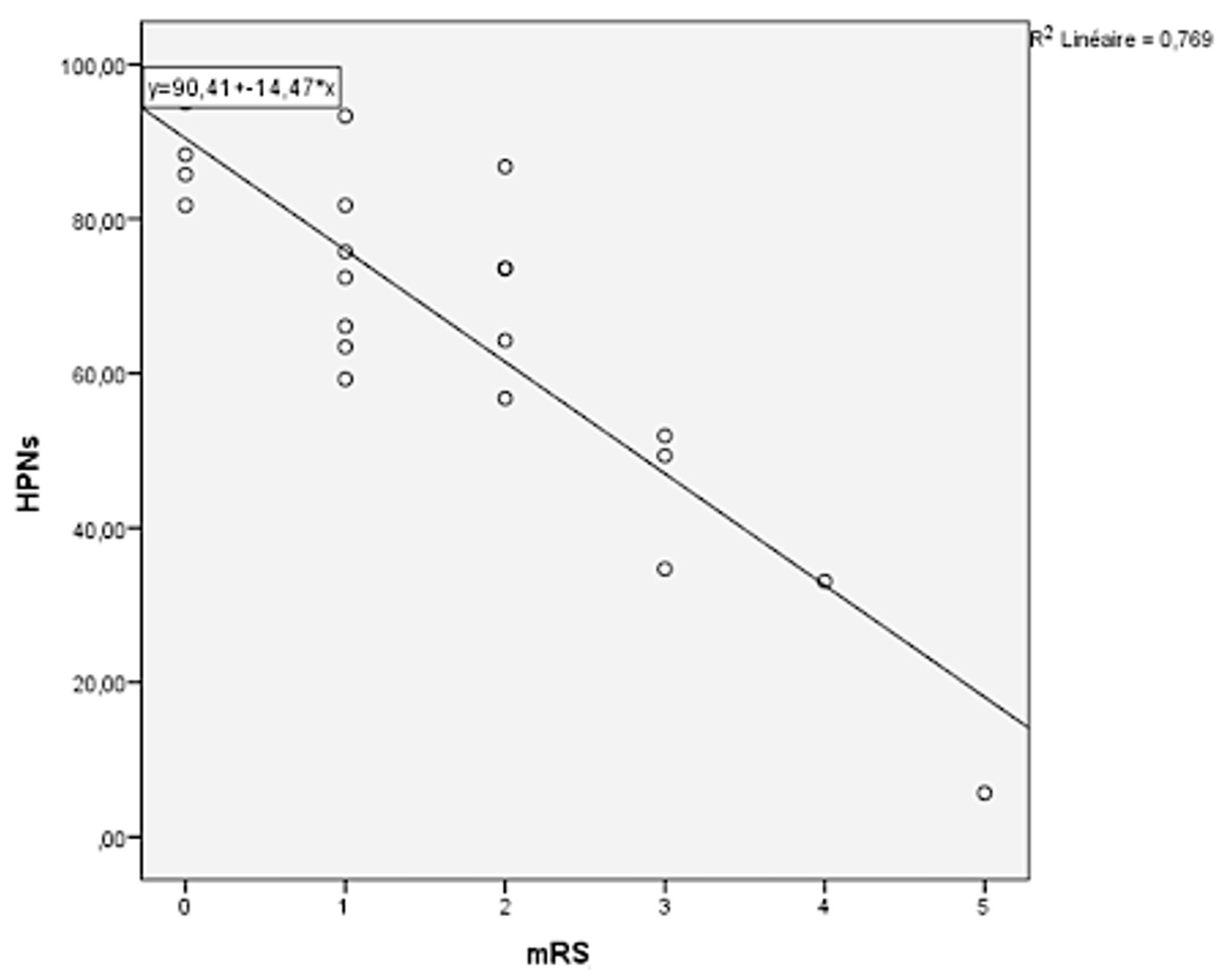
Figure 3: Distribution of changes in the modified Rankin scale and the normal pressure hydrocephalus scale (scores from entry to 12 months).
Shunt adjustments and complications:
48 of 55 patients that were followed for one year (49 patients at 3 months: because 2 deaths, 2 complications of pulmonary embolism and 2 lost to follow-up. At 6 months one patient was complicated by deep vein thrombosis worsening his gait) underwent shunt adjustments during the study due to hypodrainage or hyperdrainage; 7 (47%) had complications that could be treated conservatively and 5 (33%) of the complications required surgery. In our series, postoperative complications constituted 27% (n=15) of the cases, including 15% of complications unrelated to the shunt. 4% is the frequency of deaths in this study, of which 2% were not related to the shunt. Shunt infections were found in 4% of the cases requiring the removal of the material and Staphylococcus aureus is the germ often found.
Discussion
The present study has explored the characteristics of patients with normal pressure hydrocephalus, during a period from September 2016 until February 2020. with emphasis on the study protocol of NPH in our department and the distinction between the different series. Epidemiological studies show a wide variety of prevalence and incidence for iNPH. Studies based only on clinical findings [11] overestimate and studies based only on treated patients [12-14] clearly underestimate the "true" prevalence as well as the incidence of iNPH. The incidence of iNPH increases with age, and the highest incidence seems to be observed in people aged 70-79 years [13]. The diagnosis is strongly suspected in this age group. The mean age in our series is 70 years with extremes between 50 and 85 years. The most affected age group is between 60 and 69 years with 38%. In 34% of the cases, the age was between 70 and 79 years, which is consistent with published data in the literature. In our series, the distribution of men and women of our population shows a clear male predominance with 69% against 31% of women. The sex ratio was 2.2, which is consistent with literature data of major series (Trenkwalder et al [15], Iseki et al [16]).
In a retrospective study by Vanneste et al [17], 91 iNPH patients were selected for surgery based on their clinical and radiological criteria and they observed 65% improvement after surgery. In another retrospective analysis of 26 iNPH patients out of 74 sNPH, Larsson et al [18] concluded that there were no clinical parameters correlated with outcome in the 2-year postoperative period. This would suggest that optional tests such as CSF outflow resistance or external lumbar drainage, which can more effectively identify shunt responders, should be used. The resistance testing identifies the patient's opening pressure and absorptive capacity, and can be performed on an outpatient basis. In our study, we obtained results of the CSF tap test with subtraction of the CSF clear because there is no standardized follow-up protocol. In addition, there is no consensus on the short- and long-term time frame. In a prospective study of 42 iNPH patients, Malm et al [19] reported an overall improvement of 64% at 3 months versus 26% at 3 years. At 3 months, 74% of his patients were independent, at 3 years, the independent group represented only 28%. Sustained improvement at 5 years was noted by Raftopoulos et al [20] in 91% of iNPH patients. However, 57% of his patients died before their 5-year follow-up. We considered three months for our short-term follow-up and one year for long-term follow-up. As previously mentioned, at 1-year follow-up, patients still maintained an 88% improvement in walking. In addition, 84% retained their incontinence improvement and 34% retained improvement of memory 1 year after shunting. We also use the MMSE and our clinical judgment to account for and report an improved memory. However, in the case of incontinence, this was the patient self-assessment. If necessary, assessments of family members were also used.
The Improvements were also confirmed on all other scales used. In particular, the total score on the NPH scale, which is a valid and reliable scale for iNPH [21], has a very sensitive means of detecting change; this scale detected overall improvement in 98% of cases. The timed walking test (number and steps) also revealed improvements even in the subgroup with an unfavorable outcome, when no improvement or deterioration was recorded on the less sensitive mRS. Therefore, taking into account the low sensitivity of the mRS, the result of this study is acceptable. There is a wide variety of comorbidities in our study group, including stroke, heart disease, diabetes, and dyslipidemia. These factors were all associated with higher mRS scales at baseline and also at 1 year. However, neither of these nor hypertension had a negative influence on the degree of postoperative improvement 1 year after surgery. The study by Andrén et al [22] based on the evaluation of the effects of reoperation due to complications and vascular comorbidity (hypertension, diabetes, stroke, and heart disease) on outcome in iNPH patients 2-6 years after shunt surgery showed no negative impact of complications and only minor effects of vascular comorbidity on the long-term outcome in iNPH. Therefore, our study using programmable valves shows that a better outcome may result from better shunt technology, a fact that has not been found with several other types of shunts [23]. The overall complication rate of 27% was at the lower end of the published results [24]. Although long-term results have not been presented and it is known that other complications can still occur, the first postoperative year appears to be the most likely to cause complications [23]. Hopefully, these values will not increase dramatically. Hyperdrainage occurred in 29% of the complications (clinical and radiological) of our patients with programmable valves overall. This result is favorable compared to studies of other low pressure shunts (70%) [25]. It is almost identical to the value of 20% provided for conventional medium and high pressure shunts [24], and it is worse than the results with medium pressure gravitational valves (4%) [26,27].
Conclusion
The results of this prospective study in patients with NPH (iNPH and sNPH) diagnosed on clinical (gait appearance, degree of dementia and urinary incontinence) and dynamic (RCSF> 13mmHg/ml/min) criteria support shunt surgery (VA or VP shunt) in patients with Hakim's clinical triad and ventricular dilatation suggesting NPH. With appropriate diagnosis and management of NPH based on a fixed protocol, ventricular shunt surgery is a safe procedure that can improve symptoms in 98% of patients with NPH in the medium term.
Acknowledgments
All authors conceived and designed the study. Laouar Fares conducted the evaluation, analyzed the data and wrote the paper. All authors contributed to manuscript revisions. The authors declare that there is no conflict of interest.
References
1. Bret P, Guyotat J, Chazal J. 2002. Is normal pressure hydrocephalus a valid concept in 2002? A reappraisal in five questions and proposal for a new designation of the syndrome as «chronic hydrocephalus». J Neurol Neurosurg Psychiatry. 73: 9?12. Ref.: https://pubmed.ncbi.nlm.nih.gov/12082037/ DOI: https://doi.org/10.1136/jnnp.73.1.9
2. Adams RD, Fisher CM, Hakim S. 1965. Symptomatic occult hydrocephalus with « normal » cerebrospinal-fluid pressure.a treatable syndrome. N Engl J Med. 273: 117?126. Ref.: https://pubmed.ncbi.nlm.nih.gov/14303656/ DOI: https://doi.org/10.1056/nejm196507152730301
3. Hakim S, Adams RD. 1965. The special clinical problem of symptomatic hydrocephalus with normal cerebrospinal fluid pressure. Observations on cerebrospinal fluid hydrodynamics. J Neurol Sci. 2: 307?327. Ref.: https://pubmed.ncbi.nlm.nih.gov/5889177/ DOI: https://doi.org/10.1016/0022-510x(65)90016-x
4. Relkin N, Marmarou A, Klinge P. 2005. Diagnosing idiopathic normal-pressure hydrocephalus. Neurosurgery. 57: 4-16. Ref.: https://pubmed.ncbi.nlm.nih.gov/33316127/ DOI: https://doi.org/10.1111/ene.14671
5. Folstein MF, Folstein SE, Mchugh PR. 1975. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 12: 189-198. Ref.: https://pubmed.ncbi.nlm.nih.gov/1202204/ DOI: https://doi.org/10.1016/0022-3956(75)90026-6
6. Wikkelso C, Andersson H, Blomstrand C. 1986. Normal pressure hydrocephalus. Predic- tive value of the cerebrospinal fluid tap-test. Acta Neurol Scand. 73: 566-573. Ref.: https://pubmed.ncbi.nlm.nih.gov/3751498/ DOI: https://doi.org/10.1111/j.1600-0404.1986.tb04601.x
7. Katzman R, Hussey F. 1970. A simple constant-infusion man- ometric test for measurement of CSF absorption. I. Rationale and method. Neurology. 20: 534-544. Ref.: https://pubmed.ncbi.nlm.nih.gov/5463608/ DOI: https://doi.org/10.1212/wnl.20.6.534
8. Rankin J. 1957. Cerebral vascular accidents in patients over the age of 60. II. Prognosis. Scott Med J. 2: 200-215. Ref.: https://pubmed.ncbi.nlm.nih.gov/13432835/ DOI: https://doi.org/10.1177/003693305700200504
9. Bonita R, Beaglehole R. 1988. Recovery of motor function after stroke. Stroke. 19: 1497-500. Ref.: https://pubmed.ncbi.nlm.nih.gov/3201508/ DOI: https://doi.org/10.1161/01.str.19.12.1497
10. Hellström P, Klinge P, Tans J. 2012. A new scale for assessment of severity and outcome in iNPH. Acta Neurol Scand. 126: 229 237. Ref.: https://pubmed.ncbi.nlm.nih.gov/22587624/ DOI: https://doi.org/10.1111/j.1600-0404.2012.01677.x
11. Marmarou A, Young HF, Aygok GA. 2007. Estimated incidence of normal pressure hydrocephalus and shunt outcome in patients residing in assisted-living and extended-care facilities. Neurosurg Focus. 22: 1. Ref.: https://pubmed.ncbi.nlm.nih.gov/17613187/ DOI: https://doi.org/10.3171/foc.2007.22.4.2
12. Tisell M, Ho?glund M, Wikkelsø C. 2005. National and regional incidence of surgery for adult hydrocephalus in Sweden. Acta Neurol Scand. 112: 72?75. Ref.: https://pubmed.ncbi.nlm.nih.gov/16008530/ DOI: https://doi.org/10.1111/j.1600-0404.2005.00451.x
13. Brean A, Fredø HL, Sollid S. 2009. Five-year incidence of surgery for idiopathic normal pressure hydrocephalus in Norway. Acta Neurol Scand. 120: 314?316. Ref.: https://pubmed.ncbi.nlm.nih.gov/19832773/ DOI: https://doi.org/10.1111/j.1600-0404.2009.01250.x
14. Klassen BT, Ahlskog JE. 2011. Normal pressure hydrocephalus: how often does the diagnosis hold water? Neurology. 77: 1119?1125. Ref.: https://pubmed.ncbi.nlm.nih.gov/21849644/ DOI: https://doi.org/10.1212/wnl.0b013e31822f02f5
15. Trenkwalder C, Schwarz J, Gebhard J. 1995. Starnberg trial on epidemiology of Parkinsonism and hypertension in the elderly. Prevalence of Parkinson’s disease and related disorders assessed by a door-to-door survey of inhabitants older than 65 years. Arch Neurol. 52: 1017?1022. Ref.: https://pubmed.ncbi.nlm.nih.gov/7575219/ DOI: https://doi.org/10.1001/archneur.1995.00540340109020
16. Iseki C, Kawanami T, Nagasawa H. 2009. Asymptomatic ventriculomegaly with features of idiopathic normal pressure hydrocephalus on MRI (AVIM) in the elderly: a prospective study in a Japanese population. J Neurol Sci. 277: 54?57. Ref.: https://pubmed.ncbi.nlm.nih.gov/18990411/ DOI: https://doi.org/10.1016/j.jns.2008.10.004
17. Vanneste J, Augustijn P, Dirven C. 1992. Shunting normal-pressure hydrocephalus: do the benefits outweigh the risks? A multicenter study and literature review. Neurology. 42: 54?59. Ref.: https://pubmed.ncbi.nlm.nih.gov/1734324/ DOI: https://doi.org/10.1212/wnl.42.1.54
18. Larsson A, Wikkelso? C, Bilting M. 1991. Clinical parameters in 74 consecutive patients shunt operated for normal pressure hydrocephalus. Acta Neurol Scand. 84: 475?482. Ref.: https://pubmed.ncbi.nlm.nih.gov/1792852/ DOI: https://doi.org/10.1111/j.1600-0404.1991.tb04998.x
19. Malm J, Kristensen B, Stegmayr B. 2000. Three-year survival and functional outcome of patients with idiopathic adult hydrocephalus syndrome. Neurology. 55: 576?578. Ref.: https://pubmed.ncbi.nlm.nih.gov/10953197/ DOI: https://doi.org/10.1212/wnl.55.4.576
20. Raftopoulos C, Massager N, Bale?riaux D. 1996. Prospective analysis by computed tomography and long-term outcome of 23 adult patients with chronic idiopathic hydrocephalus. Neurosurgery. 38: 51?59. Ref.: https://pubmed.ncbi.nlm.nih.gov/8747951/ DOI: https://doi.org/10.1097/00006123-199601000-00014
21. Kubo Y, Kazui H, Yoshida T. 2008. Validation of grading scale for evaluating symptoms of idiopathic normal-pressure hydrocephalus. Dement Geriatr Cogn Disord. 25: 37?45. Ref.: https://pubmed.ncbi.nlm.nih.gov/18025828/ DOI: https://doi.org/10.1159/000111149
22. Andre?n K, Wikkelso? C, Sundstro?m N. 2018. Long- term effects of complications and vascular comorbidity in idiopathic normal pressure hydrocephalus: a quality registry study. J Neurol. 265: 178?186. Ref.: https://pubmed.ncbi.nlm.nih.gov/29188384/ DOI: https://doi.org/10.1007/s00415-017-8680-z
23. Drake JM, Kestle JR, Milner R. 1998. Randomized trial of cerebrospinal fluid shunt valve design in pediatric hydrocephalus. Neurosurgery. 43: 294?303. Ref.: https://pubmed.ncbi.nlm.nih.gov/9696082/ DOI: https://doi.org/10.1097/00006123-199808000-00068
24. Vanneste JA. Diagnosis and management of normal-pressure hydrocephalus. J Neurol. 247: 5?14. Ref.: https://pubmed.ncbi.nlm.nih.gov/10701891/ DOI: https://doi.org/10.1007/s004150050003
25. Boon AJ, Tans JT, Delwel EJ. 1998. Dutch Normal-Pressure Hydrocephalus Study: randomized comparison of low- and medium- pressure shunts. J Neurosurg. 88: 490?495. Ref.:
26. https://pubmed.ncbi.nlm.nih.gov/9488303/ DOI: https://doi.org/10.3171/jns.1998.88.3.0490
27. Meier U, Kiefer M, Sprung C. 2004. Evaluation of the Miethke dual- switch valve in patients with normal pressure hydrocephalus. Surg Neurol. 61: 119?127. Ref.: https://pubmed.ncbi.nlm.nih.gov/14751612/ DOI: https://doi.org/10.1016/j.surneu.2003.05.003
28. Kiefer M, Eymann R, Meier U. 2002. Five years’ experience with gravitational shunts in chronic hydrocephalus of adults. Acta Neurochir (Wien). 144: 755?767. Ref.: https://pubmed.ncbi.nlm.nih.gov/12181684/ DOI: https://doi.org/10.1007/s00701-002-0977-7




















