Indexing & Abstracting
Full Text
Research ArticleDOI Number : 10.36811/osjs.2019.110007Article Views : 26Article Downloads : 46
Adherence of Emergency Physicians to Pediatric Emergency Care Applied Research Network-Clinical Decision Rule (PECARN-CDR) in Minor Head Injuries Emergency Patients
Adel Hamed Elbaih MD1,4*, Zaynab Mohammed Elsayed MD2, Magda Ramadan El bahrawey MD2 and Maram Mahran Khalaf MSC3
1Associate Professor of Emergency Medicine, Faculty of Medicine, Suez Canal University, Ismailia Egypt
2Lecturer of Emergency Medicine, Faculty of Medicine, Suez Canal University, Ismailia Egypt
3Resident of Emergency Medicine, Faculty of Medicine, Suez Canal University, Ismailia Egypt
4Associate Professor of Emergency Medicine, Faculty of Medicine, Sulaiman Al-Rajhi Colleges, Saudi Arabia
*Corresponding Author: Dr. Adel Hamed Elbaih, Associate Professor of Emergency Medicine, Faculty of Medicine, Suez Canal University, Ismailia Egypt, Tel: 00201154599748; Email: elbaihzico@yahoo.com
Article Information
Aritcle Type: Research Article
Citation: Adel Hamed Elbaih, Zaynab Mohammed Elsayed, Magda Ramadan El bahrawey, et al. 2019. Adherence of Emergency Physicians to Pediatric Emergency Care Applied Research Network-Clinical Decision Rule (PECARN-CDR) in Minor Head Injuries Emergency Patients. Open Sci J Surg. 1: 43-56.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2019; Adel Hamed Elbaih
Publication history:
Received date: 12 April, 2019Accepted date: 19 July, 2019
Published date: 20 July, 2019
Abstract
Introduction: Pediatric Emergency Care Applied Research Network (PECARN) is the best accurately identify children at very low risk of clinically important traumatic brain injuries (ciTBIs) in the Emergency Department (ED). Therefore, the implementation of evidence-based tools for clinical decision-making in the acute care setting has shown to improve quality of care as well as patients’ outcomes. This study aimed to assess the PECARN on quality of care in mild head injury children after improving competency of emergency physician.
Methods: The study is a cross-sectional, prospective study included 50 Children with mild head trauma attending to the Emergency Department (ED) of the Suez Canal university Hospitals. Patients divided into two groups according to their age (less or more than 2 years). We used the Statistical Package of Social Science (SPSS) program version 20 for data analysis.
Results: The most common cause of injury was direct head trauma, followed by motor car accidents and the least frequent injuries were due to fall from height. Our results regarding the adherence of residents to the PECARN CDR demonstrated that the residents were adherent largely to the rule with a level of adherence of about 92%.
Conclusion: the adherence of the emergency department physicians in SCUH to the PECARN CDR while managing pediatric mild TBI. PECARN proved its effectiveness as a clinically predictive tool to understand who can safely avoid a cranial CT scan after TBI and the risk stratification provided by it was significantly associated with positive CT scan findings.
Keywords: Pediatric care; Mild head injuries; Traumatic brain injuries
Introduction
Head injuries (HIs) are one of the most leading causes of mortality and morbidity in children; furthermore, HIs are considered as a major pediatric health problem [1]. In England, it was estimated that the incidence of HIs is 400 per 100 000 children younger than 15 years old [2]. At the same age population, 35% of children were reported with HIs in India [3]. In the United States, more than 700,000 of annually HIs cases were reported in children and many cases were not reported [4]. Luckily, most HIs in children are mild traumatic brain injury (mTBI). Most children (about 85%) recover from these injuries uneventfully when properly treated [5]. Nevertheless, in some patients, mTBIs can be associated with significant morbidity, including developmental and psychosocial delays as well as long-term disability [6].
Minor head injuries (MHIs) are major problem in pediatrics, representing one of the most common causes for visits in pediatric Emergency Department (ED) [7]. The management of these children has a common dilemma for emergency residences due to the need of head computed tomography (CT) scan for intracranial injury (ICI) identification on one hand, and of limiting the sedation associated and radiation [8,9].
A CT scan is main tools for the diagnostic and evaluation of TBI because it has a rapid acquisition time, is easy to interpret, is universally available, and is reliable; it accurately and rapidly identifies traumatic brain injuries, with reducing morbidity and mortality [10]. However, it is costly, exposes patients to radiation and may be difficult with many other obstacles to obtaining CT for children [11,12]. Clinical guidelines may have proved useful for guiding clinical decision-making for children with mild traumatic brain injuries by potentially increasing recognition of injuries and reducing the frequency of CT requests [13].
To optimize the balance, availability of effective and valid clinical decision rules (CDR) in the ED is essential and vital [14]. Of the published decision rules for mild head traumas in children, the recent Pediatric Emergency Care Applied Research Network (PECARN) rule and valid attain the largest multicenter prospective study cohort with high methodological standards, appears to be the best to accurately identify children at very low risk of clinically important traumatic brain injuries (ciTBIs) in the ED [15]. The implementation of evidence-based medical tools for clinical decision-making in the acute care setting has shown to improve quality of care as well as patients’ outcomes by simple and easy clinical tools for offer the potential broad use in the ED [16]. PECARN’s CDR deal with children with mild head trauma presenting within a 24-hour period and aims to determine patients unlikely to have a clinically important traumatic brain injury who can safely and easily discharged without a CT scan [17]. In addition, PECARN has derived different CDRs for children aged less than two years and children aged two years and older. The PECARN score is a low risk population in whom cranial CT scans can routinely obviated. PECARN’s is the only CDR which has been validated externally and internally [18].
Therefore, we conduct this study to assess the PECARN on quality of care of mild head injury children after improving competency of emergency physician. This study considered adherence of the emergency department physicians in the Suez Canal University Hospital to the PECARN-CDR while managing pediatric mTBI. PECARN proved its effectiveness as a clinically predictive tool to understand who can safely avoid a cranial CT scan after TBI and the risk stratification provided by it was significantly associated with positive CT scan findings [19]. The adherence to PECARN-CDR helps the emergency physicians to decrease the time of diagnosis with better triage of patients. Furthermore, it is worth noting that adherence to PECARN-CDR will help pediatric patients to avoid the hazards of unnecessary exposure to radiation [14]. In this study, we aimed to promote the quality of care of Emergency residences to mild head trauma children using PECARN CDR in the Emergency Department of Suez Canal University Hospital.
Patients and Methods
Study Design: This was an observational, cross sectional, prospective study that was conducted on the children with mTBI under 18 years old who admitted to the Emergency Department, Suez Canal University Hospital, over a period of 9 months from January to August 2018. Ethical approval was obtained from the responsible authorities in the Suez Canal University Hospital. Verbal and written consent was obtained from the patients or them parents after explaining the aim and content of the study without any obligation.
Inclusion criteria: We included all children from both genders with 18 years old or younger. Also, children presented with mTBI (Glasgow Coma Scale, GCS: 14-15) or with HI within 24 hours.
Exclusion criteria: We excluded all patients with the following conditions: 1) GCS less than 14 after 30 minutes from the event; 2) Presented to the ED after 24 hours from the event; 3) Patients known to have bleeding tendency or coagulopathies; 4) Patients known to have chronic neurological disease (Congenital anomalies, Cerebral palsy, Epilepsy); and 5) Patients with penetrating head injury, brain tumor, or other significant injuries that may affect conscious level i.e. chest injuries causing hypoxia, external bleeding or internal hemorrhage causing hypovolemia.
Primary End-point: The adherence of the emergency residences to PECARN CDR with mild head trauma children in Emergency Department Suez Canal University Hospital.
Secondary End-points: 1) The barriers on applying PECARN CDR with mild head trauma children; and 2) The knowledge, attitude, and practice of the emergency residences with mild head trauma children using PECARN CDR.
Sample Size Calculation: We targeted all children with mild head trauma less than 18 years with (GCS 14-15) who admitted to our department January and August 2018. We used the non-probability convenience sampling method for calculation. The sample size was
calculated using the following formula [20]:
Where: n = sample size; (The critical value that divides the central 95% of the Z distribution from the 5% in the tail); Zβ = 0.84 (The critical value that separates the lower 20% of the Z distribution from the upper 80%); P1 = Prevalence/proportion in the study group = 30% [10]; P2 = Prevalence/proportion in the control group = 70% [10]; and q = 1-p. Therefore, by calculation, the sample size is equal to 21 cases. Adding 10% dropout ratio raises the sample size to 25 cases per group. The sample size is 50 cases in total [20,21].
Data Collection Tools: Data were collected in data sheet from patients fulfilling inclusion criteria. Patients were assessed clinically and managed by the ABCD protocol (airway and cervical spine control, breathing, circulation, dysfunction of central nervous system and exposure). After stabilizing the patient, the following data were studied: 1) Patient age and sex and 2) Trauma data such as:
- Time of injury and time of hospital arrival
- Mechanism of injury
- Clinical presentation
- Symptoms as agitation, vomiting, loss of consciousness, severe headache
- Signs as skull hematoma, sings of fracture base (raccoon eye, bleeding per ear or nose, battle’s sign)
- Associated injuries.
All patients were assigned to a full clinical examination (Vital signs, initial assessment of ABCDE, neurological examination, Regional examination of head, neck, chest, abdomen, extremities, and back, and then assess the condition of the patients either stable or unstable, which determined the needed investigations and plane of management).
PECARN: The PECARN CDR consists of two age specific rules: one for children less than two years of age, one for children two years and older. The elements for both age groups overlap but are not identical. We used the following criteria in our decision:
1. Very low risk: no CT required.
2. Higher risk: based on altered mental status or signs of skull fracture - CT required.
3. Intermediate Risk: may be managed by CT or observation over a period of time without CT depending on other factors such as, multiple rather than isolated findings, worsening symptoms or signs, physician experience and parental preference [12].
Investigations: All patients were subjected to the following investigations: 1) Laboratory investigations, as complete blood count, blood typing and cross match and coagulation profile; and 2) CT scan of the brain ordering and its results if CT was done.
Statistical Analysis: The data were collected, cleaned, filtered, coded and entered into the computer. We used the Statistical Package of Social Science (SPSS) program version 20 for data analysis. Data were analyzed and presented using tables, and graphs in mean and slandered deviation (SD) for continuous variables, and frequency and percentage for categorical data. Significance tests were used such as chi-square test for qualitative data and t-test for quantitative data. The significant level was considered when p value < 0.05.
Results
Our study included 50 children patients with mTBI. Patients divided into two groups according to their age (less or more than 2 years); meanwhile, to evaluate the adherence of the emergency residences to PECARN CDR in children with mTBI. Table 1 shows demographic data, clinical, laboratory, and radiological assessment of the studied patients. The most common cause of injury was direct head trauma, followed by motor car accidents and the least frequent injuries were due to fall from height. On admission, the mean of all vital signs including pulse, blood pressure (BP) and respiratory rate were within normal ranges, except for blood pressure where the mean systolic and diastolic BP was 103.9 and 67 mmHg, respectively. Regarding CT findings, 46% of children showed neurological insult and 54% of them had a free CT.
Our analysis shows the symptoms/signs of PECARN CDR among studied population where vomiting (40%) was the most reported symptom/sign followed by LOC >5 seconds (28%) then GCS < 15 (24%). Whereas, no cases reported with palpable skull fracture, table 2.
Regarding the level of adherence to PECARN CDR parameter in patients younger than 2 years, all high-risk symptoms and signs were assessed by the residents among the whole 16 patients except for Palpable skull fracture and altered mental status (AMS; agitation, somnolence, slow response, and repetitive questions) where both of them were assessed in all patients except one. Not all intermediate risk symptoms and signs were assessed in all patients; the presence of scalp hematoma and not acting normally per parents were assessed in 14 patients, severe mechanism of injury were checked in 15 patients, the exception was LOC >5 seconds which was assessed in all 16 patients. Table 3 shows the clinical assessment and level of adherence to PECARN CDR Parameter among residents in patients younger than 2 years.
All the patients presented to ER, around half of them was admitted to inward or intensive care unit (ICU) departments, 31.25 % needed neurological consultation and 18.75% discharged from ER and only once case (6.25%) died after admission. All the patients younger than 2 years presented to ER, 43.75% managed by observation, 37.5% needed surgical intervention and 18.75% discharged from ER.
|
Table 1: Demographic data, clinical, laboratory, and radiological assessment of the studied patients CT: computed tomography; PT: Prothrombin time; INR: International normalized ratio. |
||
|
Parameters |
N (%) |
|
|
Age groups |
< 2 years |
16 (32) |
|
> 2 years |
34 (68) |
|
|
Gender |
Male |
29 (58) |
|
Female |
21 (42) |
|
|
Mechanism of injury |
Motor car accident |
16 (32) |
|
Fall from height |
14 (28) |
|
|
Direct Head trauma |
20 (40) |
|
|
Blood typing |
AB |
10 (20) |
|
A |
23 (46) |
|
|
B |
13 (26) |
|
|
O |
4 (8) |
|
|
Rh |
Positive |
43 (86) |
|
Negative |
7 (14) |
|
|
CT findings |
Positive findings |
23 (46) |
|
Free CT |
27 (54) |
|
|
Vital signs |
Pulse |
92.7 ± 13.3 |
|
Systolic Blood pressure (mmHg) |
103.9 ± 4.9 |
|
|
Diastolic Blood pressure (mmHg) |
67 ± 5.3 |
|
|
Respiratory rate |
18.1 ± 3.5 |
|
|
Complete blood count |
Total leucocytic count (cell x103/mm2) |
6.24 ± 1.89 |
|
Hemoglobin (mg/dl) |
12.17 ± 0.93 |
|
|
Platelets count (cell x103/mm2) |
217.5 ± 10.51 |
|
|
Coagulation profile |
PT (second) |
14.5 ± 0.81 |
|
INR |
1.2 ± 0.2 |
|
|
Table 2: Symptoms/ signs of PECARN CDR among studied population (n=50). |
||
|
Variables |
Present |
Absent |
|
n (%) |
n (%) |
|
|
GCS < 15 |
12 (24) |
38 (76) |
|
0 |
15 (30) |
|
|
Signs of basilar skull fracture (raccoon eye, bleeding per nose or ear) |
5 (10) |
27 (54) |
|
Vomiting |
20 (40) |
13 (26) |
|
AMS (agitation, somnolence, slow response, repetitive questions) |
13 (26) |
27 (54) |
|
Scalp hematoma (excluding frontal) |
4 (8) |
11 (22) |
|
Not acting normally per parent |
9 (18) |
6 (12) |
|
LOC >5 seconds |
14 (28) |
36 (72) |
|
Severe headache |
5 (10) |
22 (44) |
|
Severe mechanism of injury |
7 (14) |
38 (76) |
|
AMS: Altered mental status, GCS: Glasgow Coma Scale, LOC: loss of consciousness. |
||
|
Table 3: Clinical assessment and level of adherence to PECARN CDR Parameter among residents in patients younger than 2 years (n=16). |
||||
|
Variables |
Level of adherence |
Clinical assessment |
||
|
Yes |
No |
Present |
Absent |
|
|
n (%) |
n (%) |
n (%) |
n (%) |
|
|
High risk symptoms/ signs |
||||
|
GCS < 15 |
16(100) |
0 (0) |
8(50) |
8(50) |
|
Palpable skull fracture |
15(93.8) |
1(6.2) |
0 |
15(100) |
|
AMS (agitation, somnolence, slow response, repetitive questions) |
15(93.8) |
1(6.2) |
9(60) |
6(40) |
|
Intermediate risk symptoms/ signs |
||||
|
Scalp hematoma (excluding frontal) |
14(87.5) |
2(12.5) |
4(28.6) |
10(71.4) |
|
Not acting normally per parent |
14(87.5) |
2(12.5) |
9(64.3) |
5(35.7) |
|
LOC >5 seconds |
16(100) |
0(0) |
7(43.8) |
9(56.2) |
|
Severe mechanism of injury |
15(93.8) |
1(6.2) |
3(20) |
12(80) |
|
AMS: Altered mental status, GCS: Glasgow Coma Scale, LOC: loss of consciousness |
||||
Regarding the level of adherence to PECARN CDR parameter in patients older than 2 years, GCS<15 was assessed in all patients, Signs of basilar skull fracture were assessed in most of the patients (32) and AMS (agitation, somnolence, slow response, repetitive questions) were the least to be assessed; in only 25 patients. Intermediate risk symptoms and signs were not assessed in all patients; presence of vomiting was checked in almost all patients (33), severe headache and severe mechanism of injury were assessed in 27 and 30 patients, respectively. Like with the patients younger than 2 year, LOC>5 seconds was the only sign that was assessed in all patients. Table 4 shows the clinical assessment and level of adherence to PECARN CDR Parameter among residents in patients older than 2 years.
|
Table 4: Clinical assessment and level of adherence to PECARN CDR Parameter among residents in patients 2 years or older (n=34). |
||||
|
Variables |
Level of adherence |
Clinical assessment |
||
|
Yes |
No |
Present |
Absent |
|
|
n (%) |
n (%) |
n (%) |
n (%) |
|
|
High risk symptoms/ signs |
||||
|
GCS < 15 |
34 (100) |
0 (0) |
4 (11.8) |
30 (88.2) |
|
Signs of basilar skull fracture (raccoon eye, bleeding per nose or ear) |
32 (94.1) |
2 (5.9) |
5 (15.6) |
27 (84.4) |
|
AMS (agitation, somnolence, slow response, repetitive questions) |
25 (73.5) |
9 (26.5) |
4 (16) |
21 (84) |
|
Intermediate risk symptoms/ signs |
||||
|
Scalp hematoma (excluding frontal) |
33 (97.1) |
1 (2.9) |
20 (60.6) |
13 (39.4) |
|
Not acting normally per parent |
34 (100) |
0 (0) |
7 (20.6) |
27 (79.4) |
|
LOC >5 seconds |
27 (79.4) |
7 (20.6) |
5 (18.5) |
22 (81.5) |
|
Severe mechanism of injury |
30 (88.2) |
4 (11.8) |
4 (13.3) |
26 (86.7) |
|
AMS: Altered mental status, GCS: Glasgow Coma Scale, LOC: loss of consciousness |
||||
Children aging two years or older had different fate where half of them was needed neurological consultation, 20.6 % of them were admitted to in-wards or ICU, 23.5% discharged from ER and 2 cases (5.9%) died after admission (Figure 1). All the patients 2 years and older presented to ER, 32.43% managed by observation, 27.03% needed surgical intervention and 21.62% discharged from ER (Figure 2). There was a statistically significant relationship between CT findings and risk stratification as shown in table 5.
|
Table 5: Association between findings in CT scan and risk stratifications among. |
|||
|
Risk stratifications |
CT finding |
p-value |
|
|
Positive (n=23) |
Negative (n=27) |
||
|
N (%) |
N (%) |
||
|
High |
13 (56.5) |
7 (25.9) |
0.008* |
|
Intermediate |
10 (43.5) |
12 (44.4) |
|
|
Low |
0 |
8 (29.6) |
|
|
patients |
|||

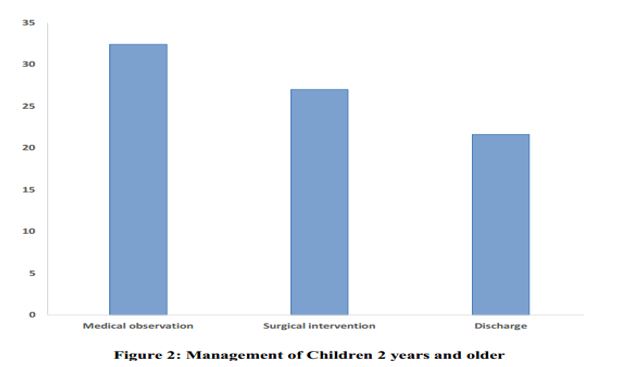
Table 6 showed level of adherence of PECARN CDR Parameter among residents in studied population where average level of adherence children younger than 2 years was 93.77% while average level of adherence children 2 years or older was 90.19%. Average total level of adherence between both age groups was 92.01%.
|
Table 6: Average level of adherence of PECARN CDR Parameter among residents in studied population (n=50). |
|
|
Variable |
Level of adherence |
|
Children younger than 2 years |
|
|
High risk symptoms/ signs |
95.87% |
|
Intermediate risk symptoms/ signs |
92.23% |
|
Average level of adherence |
93.77% |
|
Children 2 years or older |
|
|
High risk symptoms/ signs |
89.20% |
|
Intermediate risk symptoms/ signs |
91.17% |
|
Average level of adherence |
90.19% |
|
Total Level of adherence |
92.01% |
Discussion
Although the CT is essential diagnostic tool in pediatric head injuries but the rising costs and the ionizing radiation exposure hazards are still to cause growing concern. Considerable efforts devoted to provide the required optimum balance [22]. Thus, to be able to identify the high-risk children in the management of pediatric mild TBI, several scoring systems are suggested but the most famous is “Pediatric Emergency Care Applied Research Network (PECARN) TBI prediction rules” [13]. Adherence of physicians to such scores and Clinical Decision Rules (CDRs) in the management of head injuries is the core for ensuring the best resource utilization and clinical outcomes [23].
This prospective, cross-sectional, observational study was set with the aim of evaluating the adherence of emergency residents in the emergency department of Suez Canal University Hospital to PECARN CDR, while dealing with pediatric patients with mild head trauma. In our study, we included 50 patients, 58 % of whom were males and 42 % were females. Around two thirds (n=34) of them were above 2 years old and one-third (n=16) were below 2 years old.
We found that there was a statistically significant relationship between CT findings and risk stratification (p=0.008) indicating the value of PECARN rule in prediction of clinically important traumatic brain injury (ciTBI) in children with mild TBI. Several lines of the literature considerably support this finding. Nakhjavan Shahraki and colleagues reported that PECARN rule had a proper calibration in prediction of ciTBI and CT scan findings. Moreover, they found that Brier score (overall performance) of PECARN rule in predicting ciTBI in children under 2 and 2-18 years were 1.5 and 1.2, respectively. Furthermore, PECARN had a sensitivity and specificity of 92.3 and 40.6%, respectively, in predicting ciTBI in children under 2 years, 100.0, and 57.8%, respectively, in individuals between the ages of 2 and 18 [24].
Another study by Easter et al., [25] evaluated the prediction ability of three different CDRs (Canadian Assessment of Tomography for Childhood Head Injury, Children’s Head Injury Algorithm for the Prediction of Important Clinical Events, and PECARN) as well as the physician judgment in prediction of ciTBI in children with minor head injuries presenting to the emergency department. Interestingly, they found that only PECARN [Sensitivity= 100% (95% CI 84% to 100%)] and physician practice [Sensitivity= 95% (95% CI 76% to 100%)] had the ability to identify all clinically important TBIs.
Regarding the risk stratification for patients 40% of them were classified as high risk, 44% as intermediate risk and 16% as low risk of development of ciTBIs. These results were rather inconsistent with previous studies. For example, in the study by Abouzeid et al., [12], 20.6% of patients were classified as high risk which is lower than the current study (40%), 45.3% as intermediate risk, and 35% as the low risk of developing ciTBI which is higher than the current study (16%). A Possible cause of these differences can be the different mechanism of injury. In the current study, direct head trauma was recorded to be the most common cause of injury (40%) and fall from height was the least common (28%). In contrast, in the study of Abouzeid and colleagues, fall from a height was the most common cause of mTBI (60%) and the direct head injury was the second most common cause (30%).
Furthermore, Nathan Kuppermann et al., [13], in their multi-centre cohort study, revealed that 14% of patients were classified as High Risk, 29% as Intermediate Risk, and 57% as Low Risk of developing ciTBI. This inconsistency can be perfectly explained by the huge difference in sample size as they included 42,412 children in their multi-centre study and because of the exclusion of patients with GCS equal 13 in out of the study.
Our results regarding the adherence of residents to the PECARN CDR demonstrated that the residents were adherent to a large extent to the rule with a level of adherence of about 92%. Regarding infants younger than two years, they assessed almost all the high-risk symptoms and signs and most of the intermediate-risk symptoms and signs except for “the presence of scalp hematoma” and “not acting normally per parents in patients “which were not assessed in only two infants and “severe mechanism of injury” which were missed in only one infant. Similarly, regarding patients of the age of two years or older, the high-risk symptoms and signs were perfectly assessed except for “signs of basilar skull fracture” and “AMS” which were missed in two and seven patients, respectively. The intermediate-risk symptoms and signs were also assessed in most of the patients; however, severe headache and severe mechanism of injury were assessed only in 27 and 30 patients out of 34, respectively.
These results are consistent with the other studies assessing the level of adherence of the physicians to PECARN CDR Criteria. For example, in their retrospective study conducted in a 2-campus hospital to determine adherence to PECARN criteria, Maria and colleagues reported a high level of adherence to the criteria among the different specialties dealing with minor pediatric head trauma represented by 97.7% of the pediatric emergency residents, 90.1% of emergency residents, and 98.3% of general practioners [26].
In another study held in an Italian care academic Pediatric Emergency Room describing the implementation of an adapted version of the PECARN rule and evaluating the process in terms medical staff adherence and satisfaction, Schonfeld and colleagues resulted level of adherence to the PECARN rule of 93.5% [24]. In contrast, in his multicenter retrospective study, Velasco R investigated the compliance with the PECARN CDR as a diagnostic approach in mild head trauma patients who are younger than 2 years old and the results revealed that the level of compliance with PECARN CDR was low with an average of 62.2% compliance to the CDR [27]. It was a multi-center study conducted in four hospitals with different levels of health care while the present study is a single-center study (ED of SCU Hospital). Additionally, sample size was 1361 patients (four hospitals), compared to only 50 patients in the current study. These two causes can explain this inconsistency of the results.
Another study by Ahmed Abouzeid and colleagues, yet similar to the current study being a single-centre one and held in the same setting (ED of SCU Hospital), also demonstrated a low level of adherence to the PECARN CDR of 62.9% while evaluating CT scan ordering in comparison to the PECARN clinical decision rule (CDR). This matter of inconsistency might have been resulted from the difference in severity of cases of head trauma, with which each study had dealt. To illustrate, in the current study, about 40% of all the cases were considered high-risk which represent over two thirds of the patients younger than 2 years old and 30% of patients older than 2 years old. On the other hand, in the study of Ahmed Abouzeid and colleagues, only 20.6% of patients were classified as high risk [12]. Table 7 shows the Comparison of current study results with Nakhjavan-Shahraki et al [24] and Abouzeid A et al, [12].
|
Table 7: Comparison of current study results with Nakhjavan-Shahraki et al and Abouzeid A et al. |
|||
|
Variables |
Current study |
Nakhjavan-Shahraki et al |
Abouzeid A |
|
Sample size (N) |
50 |
594 |
97 |
|
Age (years), mean ± SD |
6.3±3.5 |
7.9±5.3 |
- |
|
Age groups, n (%) |
|
|
|
|
< 2 years |
16(32) |
114(19.2) |
20(20.7) |
|
≥ 2 years |
34(68) |
480(80.8) |
77(79.3) |
|
Gender, n (%) |
|
|
|
|
Male |
29(58) |
417(79.3) |
- |
|
Female |
21(42) |
123(20.7) |
- |
|
CT findings, n (%) |
|
|
|
|
Positive findings |
23(46) |
81(24.6) |
- |
|
Free CT |
27(54) |
248(75.4) |
- |
|
PECARN risk group |
|
|
|
|
Age <2 years |
|
|
|
|
Very low risk |
1(6.3) |
42(36.8) |
- |
|
Intermediate risk |
5(31.3) |
64(56.1) |
- |
|
High risk |
10(62.5) |
8(7) |
- |
|
Age ≥2 years |
|
|
|
|
Very low risk |
7(20.6) |
253(52.7) |
- |
|
Intermediate risk |
17(50) |
202(42.1) |
- |
|
High risk |
10(29.4) |
25(5.2) |
- |
|
Outcome of patients |
|
|
|
|
Neurosurgical consultation |
22(44) |
- |
22(36) |
|
Admission in the inward or ICU |
14(28) |
- |
6(9.8) |
|
Surgical intervention |
16(32) |
- |
7(11.5) |
|
Discharged |
11(22) |
- |
26(42.6) |
This study showed a considerable adherence of the emergency department physicians in the Suez Canal University Hospital to the PECARN CDR while managing pediatric mild TBI. PECARN proved its effectiveness as a clinically predictive tool to understand who can safely avoid a cranial CT scan after TBI and the risk stratification provided by it was significantly associated with positive CT scan findings.
The adherence to PECARN CDR helps the emergency physicians to decrease the time of diagnosis with better triage of patients. Furthermore, it is worth noting that adherence to PECARN CDR will help pediatric patients to avoid the hazards of unnecessary exposure to radiation.
It is recommended to increase the awareness of the emergency physicians about the importance of adherence to CDRs and their full comprehension of the PECARN CDR and its effectiveness as a predictor of ciTBI. Implementation of the PECARN CDR which will lead to decrease the unnecessary CT scan ordering in children with mTBI and help them avoid the hazardous over exposure to radiation. Regular workshops provided by hospitals will help to ensure perfect adherence of emergency physicians to such scores. Lectures covering the up-to-date guidelines and strategies regarding triage and patients’ assessment would undoubtedly affect the performance of emergency physicians.
Limitations: This study has many limitations such as a small sample size, single center study, which make the generalization of the results not possible. Another limitation is the probability of the selection bias due to the convenience sampling. In younger patients, sometimes it was hard to get clear information from the family regarding trauma history and symptoms. Some parents exaggerated the history of trauma or symptoms to get a CT scan.
In conclusion, the emergency residents at Suez Canal University Hospital were highly adherent to the PECARN CDR while managing pediatric mild TBI. We found a statistically significant relationship between CT findings and risk stratification, indicating the value of PECARN rule in prediction of clinically important traumatic brain injury (ciTBI) in children with mild TBI.
Our study recommends:
• Increasing the awareness of the emergency physicians about the importance of adherence to CDRs.
• Full comprehension of the emergency physicians of the PECARN CDR and its role in guiding the CT ordering decision.
• Raising the awareness about the effectiveness of PECARN CDR as a predictor of ciTBI.
• Full comprehension of the emergency physicians of the hazardous consequences of over exposure to radiation especially in young ages.
Further studies assessing the possible barriers that may hinder the complete adherence of physicians to such rules should considered.
References
References
1. Robertson BD, McConnel CE, Green S. 2013. Charges associated with pediatric head injuries: a five-year retrospective review of 41 pediatric hospitals in the US. J Inj Violence Res. 5: 51-60. Ref.: https://bit.ly/2LlIiY5
2. Trefan L, Houston R, Pearson G, et al. 2016. Epidemiology of children with head injury: a national overview. 101: 527-532. Ref.: https://bit.ly/2NTZBBh
3. Bhargava P, Singh R, Prakash B, et al. 2006. Pediatric head injury: An epidemiological study. J Pediatr Neurosci. 6: 97-98. Ref.: https://bit.ly/2NXglI4
4. Schneier AJ, Shields BJ, Hostetler SG, et al. 2006. Incidence of Pediatric Traumatic Brain Injury and Associated Hospital Resource Utilization in the United States. Pediatrics. 118: 483-492. Ref.: https://bit.ly/2ShTiGx
5. Caskey RC, Nance ML. 2014. Management of pediatric mild traumatic brain injury. Adv Pediatr. 61: 271-286. Ref.: https://bit.ly/2JIi7rb
6. Daneshvar DH, Riley DO, Nowinski CJ, et al. 2011. Long-term consequences: effects on normal development profile after concussion. Phys Med Rehabil Clin N Am. 22: 683-700. Ref.: https://bit.ly/2YWhTmv
7. Chen C, Peng J, Sribnick EA, et al. 2018. Trend of Age-Adjusted Rates of Pediatric Traumatic Brain Injury in U.S. Emergency Departments from 2006 to 2013. Int J Environ Res Public Health. 15. Ref.: https://bit.ly/2Y7Vq8X
8. Taylor CA, Bell JM, Breiding MJ, et al. 2017. Traumatic Brain Injury-Related Emergency Department Visits, Hospitalizations, and Deaths - United States, 2007 and 2013. MMWR Surveill Summ. 66: 1-16. Ref.: https://bit.ly/2JzhuRP
9. Brenner DJ, Elliston CD, Hall EJ, et al. 2001. Estimated Risks of Radiation-Induced Fatal Cancer from Pediatric CT. Am J Roentgenol. 176: 289-296. Ref.: https://bit.ly/32ufHVJ
10. Mutch CA, Talbott JF, Gean A. 2016. Imaging Evaluation of Acute Traumatic Brain Injury. Neurosurg Clin N Am. 27: 409-439. Ref.: https://bit.ly/2Y7W723
11. Amyot F, Arciniegas DB, Brazaitis MP, et al. 2015. A Review of the Effectiveness of Neuroimaging Modalities for the Detection of Traumatic Brain Injury. J Neurotrauma. 32: 1693-1721. Ref.: https://bit.ly/2XHMOqe
12. Abouzeid A, Shaban M, Elemam T, et al. 2018. EVALUATIONS OF COMPUTED TOMOGRAPHY (CT) SCAN ORDERING IN CHILDREN WITH MILD HEAD INJURY AT EMERGENCY DEPARTMENT AT SUEZ CANAL UNIVERSITY HOSPITALct-scan-children-mild-head-injury First Introduction. Ref.: https://bit.ly/2Z5o9s8
13. Kuppermann N, Holmes JF, Dayan PS, et al. 2009. Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet. 374: 1160-1170. Ref.: https://bit.ly/2Geuvyc
14. Stiell IG, Bennett C. 2007. Implementation of Clinical Decision Rules in the Emergency Department. Acad Emerg Med. 14: 955-959. Ref.: https://bit.ly/2SkBKcF
15. Pickering A, Harnan S, Fitzgerald P, et al. 2011. Clinical decision rules for children with minor head injury: a systematic review. Arch Dis Child. 96: 414-421. Ref.: https://bit.ly/2xNKHBN
16. Armon K, MacFaul R, Hemingway P, et al. 2004. The impact of presenting problem-based guidelines for children with medical problems in an accident and emergency department. Arch Dis Child [Internet]. 89: 159-164. Ref.: https://bit.ly/2Jzi81H
17. Babl FE, Lyttle MD, Bressan S, et al. 2014. A prospective observational study to assess the diagnostic accuracy of clinical decision rules for children presenting to emergency departments after head injuries (protocol): the Australasian Paediatric Head Injury Rules Study (APHIRST). BMC Pediatr. 14: 148. Ref.: https://bit.ly/2NWFlPH
18. Schonfeld D, Bressan S, Da Dalt L, et al. 2014. Pediatric Emergency Care Applied Research Network head injury clinical prediction rules are reliable in practice. Arch Dis Child. 99: 427-431. Ref.: https://bit.ly/2JKkxWm
19. Atabaki SM, Jacobs BR, Brown KM, et al. 2017. Quality Improvement in Pediatric Head Trauma with PECARN Rules Implementation as Computerized Decision Support. Pediatr Qual Saf. 2: 19. Ref.: https://bit.ly/2JIjWV3
20. Dawson B, Trapp RG. 2004. Basic & clinical biostatistics. 4th ed. New York: Lange Medical Books-McGraw-Hill, Medical Pub. Division.
21. McKinlay A, Grace RC, Horwood LJ, et al. 2008. Prevalence of traumatic brain injury among children, adolescents and young adults: Prospective evidence from a birth cohort. Brain Inj. 22: 175-181. Ref.: https://bit.ly/2SkCSNr
22. Andrade F, Montoro N, Oliveira R, et al. 2016. Pediatric minor head trauma: do cranial CT scans change the therapeutic approach? Clinics. 71: 606-610. Ref.: https://bit.ly/2XVrloW
23. Ballard DW, Rauchwerger AS, Reed ME, et al. Emergency Physicians’ Knowledge and Attitudes of Clinical Decision Support in the Electronic Health Record: A Survey-based Study. Carpenter CR, editor. Acad Emerg Med. 20: 352-360. Ref.: https://bit.ly/30BxEQw
24. Nakhjavan-Shahraki B, Yousefifard M, Hajighanbari MJ, et al. 2017. Pediatric Emergency Care Applied Research Network (PECARN) prediction rules in identifying high risk children with mild traumatic brain injury. Eur J Trauma Emerg Surg. 43: 755-762. Ref.: https://bit.ly/2xRPqTa
25. Easter JS, Bakes K, Dhaliwal J, et al. 2014. Comparison of PECARN, CATCH, and CHALICE Rules for Children with Minor Head Injury: A Prospective Cohort Study. Ann Emerg Med. 64: 145-152. Ref.: https://bit.ly/2XOQWoz
26. Tama M, Andharia N, Bufano C, et al. 2017. Does Specialty Training and Practice Setting Affect Adherence to the Pediatric Emergency Care Applied Research Network Criteria for Pediatric Head Trauma? Pediatr Emerg Care. 1. Ref.: https://bit.ly/32svyE8
27. Velasco R, Arribas M, Valencia C, et al. 2015. Compliance with the PECARN and AEP guidelines in diagnostic approach of mild head trauma in patients younger than 24 months old. An Pediatría. 83: 166-172. Ref.: https://bit.ly/2XTTM6A




















