Indexing & Abstracting
Full Text
Case BlogDOI Number : 10.36811/ojrmi.2021.110011Article Views : 89Article Downloads : 49
Basilar neuralgia vs. dolichoectasia: A report of three cases
Abdulwahab Alahmari
Radiology Specialist, Radiology Department, Al-Namas General Hospital, Ministry of Health, Al-Namas City, Saudi Arabia
*Corresponding Author: Abdulwahab Alahmari, Radiology Specialist, Radiology Department, Al-Namas General Hospital, Ministry of Health, Tel: +966562428716; Email: afaa99@hotmail.co.uk
Article Information
Aritcle Type: Case Blog
Citation: Abdulwahab Alahmari. 2021. Basilar neuralgia vs. dolichoectasia: A report of three cases. O J Radio Med Img. 4: 01-09.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2021; Abdulwahab Alahmari
Publication history:
Received date: 21 December, 2020Accepted date: 15 January, 2021
Published date: 19 January, 2021
Abstract
Basilar artery dolichoectasia is a vague term that describe too many normality and abnormalities under one term. Basilar artery occlusion is a rare finding in a healthy patient in his 40s. This case will present the role of basilar neuralgia in forming a basilar artery occlusion which lead to many neurological events that was documented on multiple CT scans.
Keywords: Basilar neuralgia; Dolichoectasia; Basilar artery occlusion; Infarctions; CT
Introduction
The basilar artery can be affected by calcification, tortuousness, curvatures, dilatation causes occlusion. The occlusion will lead to stroke usually in the basilar artery supplied territory including (cerebellum, pons, posterior cerebral artery territory). The basilar artery gives branches which are; the inferior cerebellar, pontine, superior cerebellar arteries, perforating artery, and finally, it bifurcates into two posterior cerebral arteries. Basilar neuralgia is a new term used to describe this condition. This paper will discuss and set standards for this medical condition. Basilar artery occlusion is rare and it occurs in 1% of the ischemic cases [1].
The first case of basilar artery occlusion
A forty-eight-year-old male Indonesian patient came to the ER in a secondary hospital with history of hypertension, vomiting, dizziness, chronic headache (for almost 2 years), and the patient lost his consciousness suddenly in his house. The patient was in this condition for 24 hours before he was shifted to a tertiary hospital and the patient was suffering from a dyspnea (oxygen saturation was very low 52 mm Hg and the patient was on a ventilator). The patient was suspected to have a cerebrovascular accident (CVA). A CT scan was done for the brain, chest, abdomen, and pelvis. Then, the patient was admitted to intensive care unit (ICU). The CT showed multiple ill-defined faint hypo−attenuated areas at the right parietal lobe, right occipital lobe, and bilateral cerebellum which appears like an old infarction. There is a small like hole infarction in the posterior limb of the internal capsule on the right side. Two calcified structures present in multiple areas in the basilar artery and the left vertebral artery. The average Hounsfield unit for the calcified structures is 142 and 120 for the basilar artery and the left vertebral artery respectively. The right vertebral artery is crossing from the right side to join the dominant left vertebral artery on the left side to form the basilar artery. The basilar artery is dilated and curved. The basilar artery is crossing from the left side to the right side in pre-pontine space then re-crosses from the left side to the right side on top of the Sella. The basilar artery in this case, fits with the criteria of basilar neuralgia criteria mentioned previously in two cases. The CT scan of the chest revealed an aspiration pneumonia. The CT chest shows a ventilator and a nasogastric tube placed in the patient. A Foley catheter was seen in the urethra on the abdomen/pelvis CT. After two days of admission to ICU, the patient suffered from a bradycardia (two times) and a resuscitation was done. The patient kidney function collapsed since he was admitted, as a result a CT scan with contrast can’t be performed to check if there is any filling defect in the basilar artery. A second plain CT was done 72 hours after the admission, which revealed a second calcified structure was formed see (figure 1 through 21).

Figure 1: A calcified left vertebral artery.

Figure 2: The right vertebral artery crosses to the left side to join the dominant left vertebral artery to form the basilar artery (CT image, axial section, brain scan).
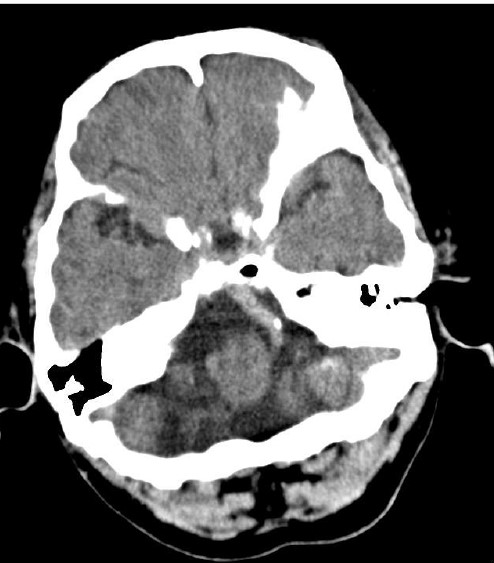
Figure 3: The dilated dense curved basilar artery containing some calcified structure (occluded basilar artery). The basilar artery crosses from the left side to the right side in the basilar cistern (CT image, axial section, brain scan).
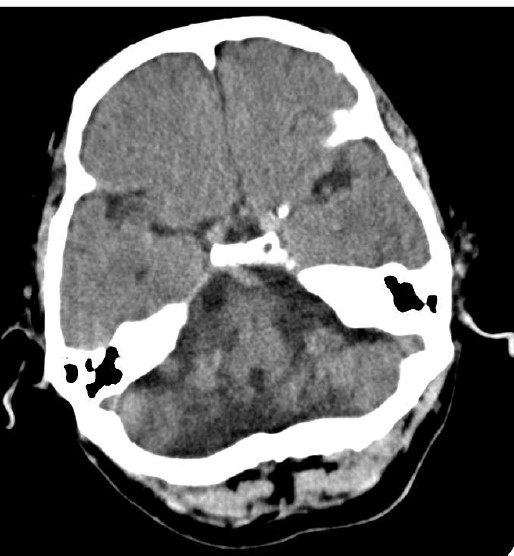
Figure 4: The basilar artery is dilated and located on the left side (CT image, axial section, brain scan).
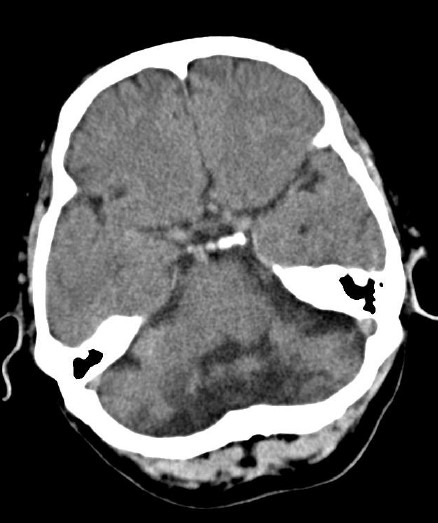
Figure 5: There is a hypo-attenuated area in the cerebellum (CT image, axial section, brain scan).
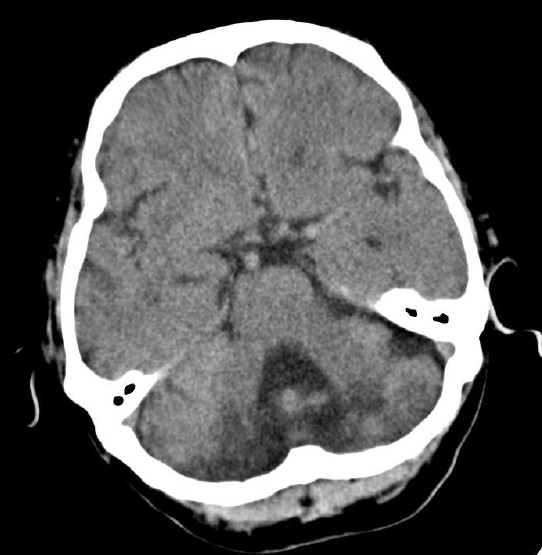
Figure 6: There is a hypo-attenuated area in the cerebellum looks like an acute infarction and dilated 4th ventricle (CT image, axial section, brain scan).
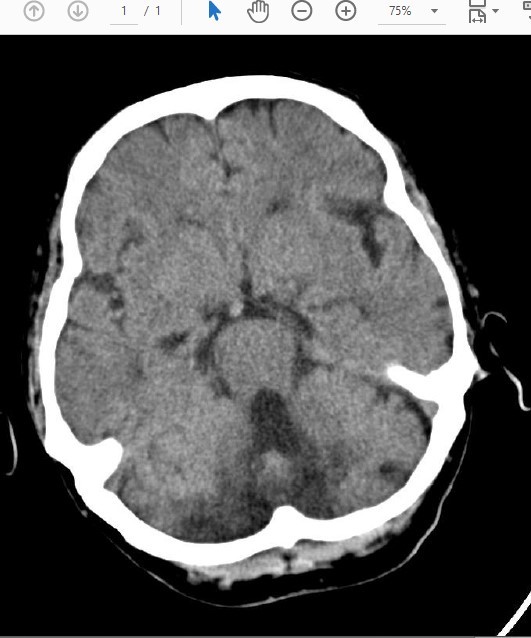
Figure 7: There is a hypo-attenuated area in the cerebellum looks like an acute infarction and dilated 4th ventricle (CT image, axial section, brain scan).
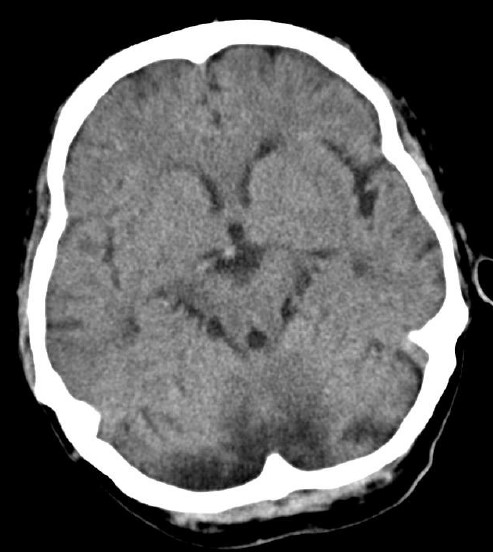
Figure 8: There is a hypo-attenuated area in the cerebellum (CT image, axial section, brain scan).
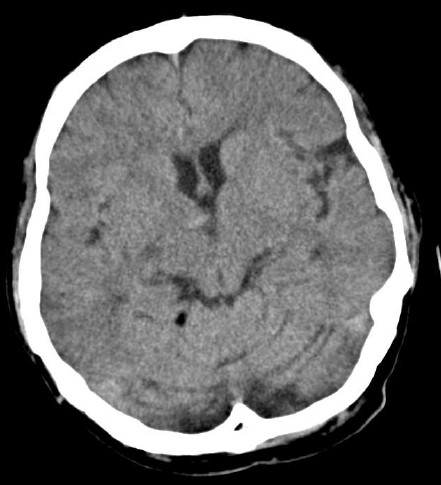
Figure 9: There is a hypo-attenuated hole like area in the right cerebellar hemisphere looks like an old infarction (CT image, axial section, brain scan).
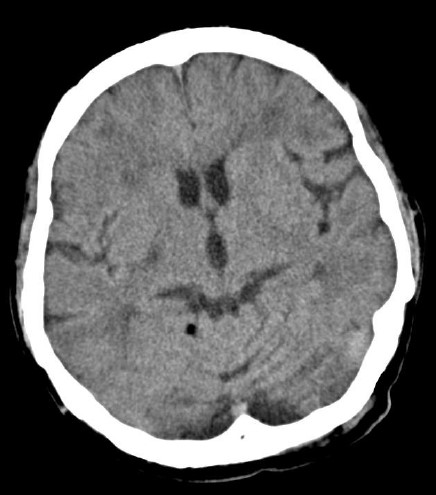
Figure 10: There is a hypo-attenuated hole like area in the right cerebellar hemisphere looks like an old infarction (CT image, axial section, brain scan).
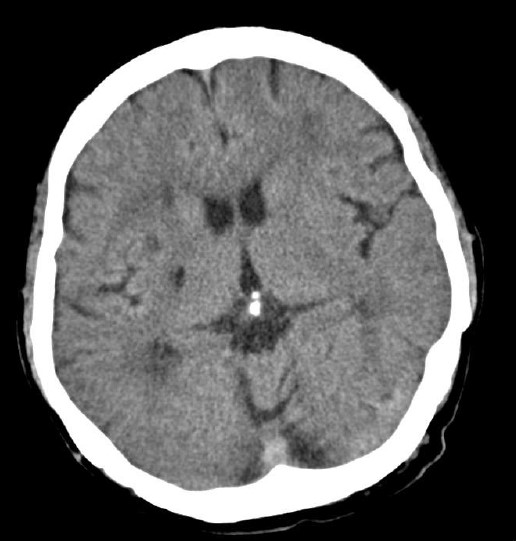
Figure 11: There is a hypo-attenuated hole like area in the posterior limb of the right internal capsule looks like an old infarction (CT image, axial section, brain scan).
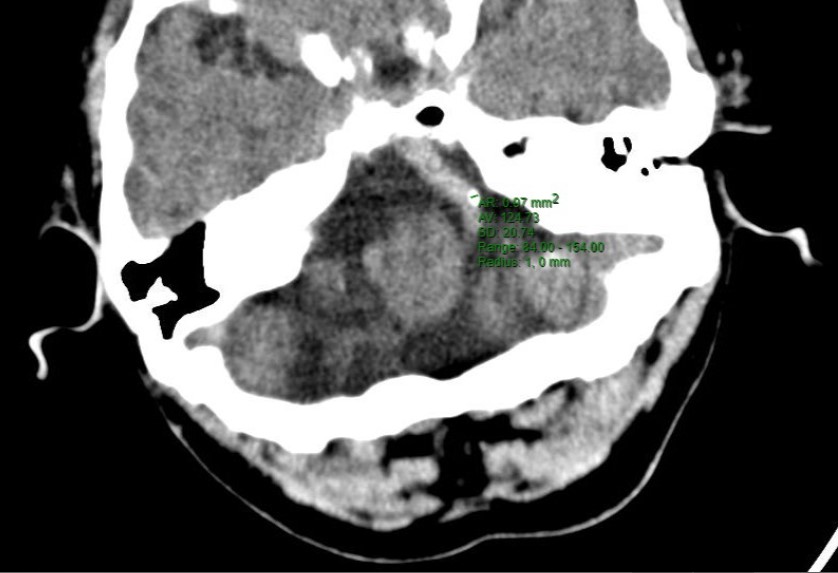
Figure 12: The Hounsfield unit of the calcified structure (occluded basilar artery) in the basilar artery is 124 Hounsfield units (CT image, axial section, brain scan).
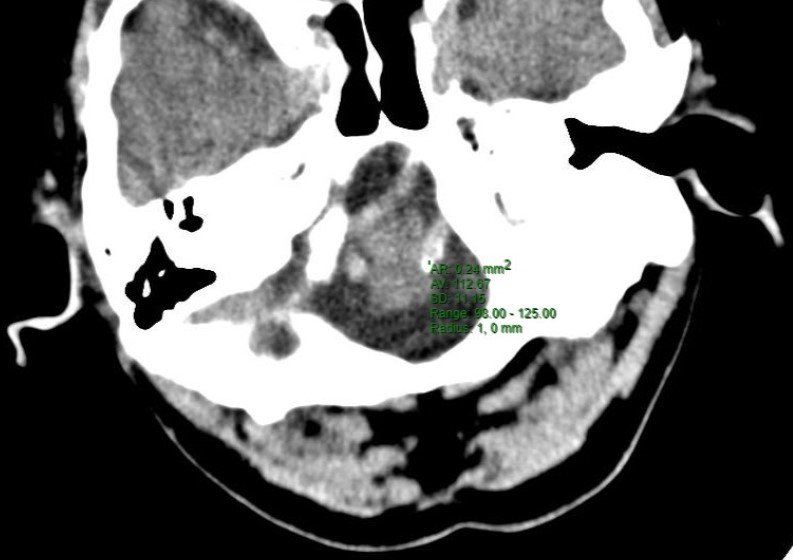
Figure 13: The Hounsfield unit of the calcified structure in the left (dominant) vertebral artery is 112 Hounsfield units (CT image, axial section, brain scan).

Figure 14: The basilar artery is curved (134? on the right side and 136? on the left side) the average degree of curvature is 135? (CT image, axial section, brain scan).
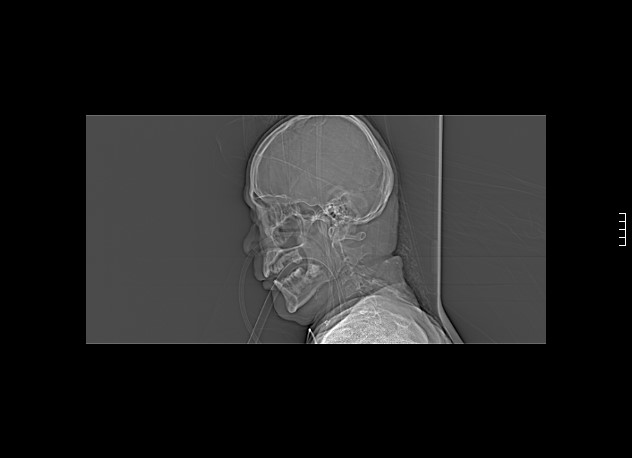
Figure 15: CT tomogram shows the nasogastric tube and the ventilator placed inside the patient during the CT scanning.
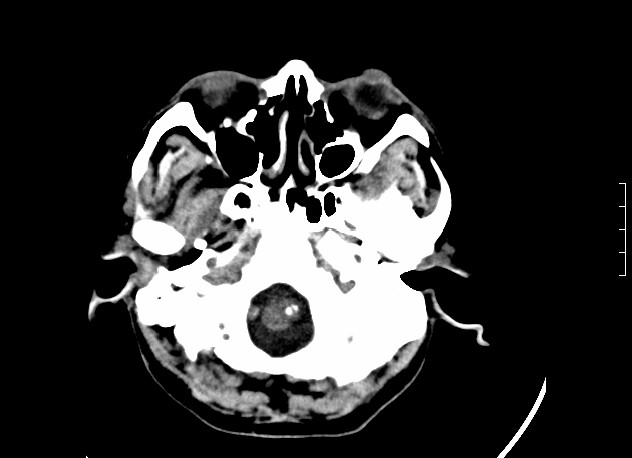
Figure 16: A repeat CT scan after 72 hours showing the calcified left vertebral artery.
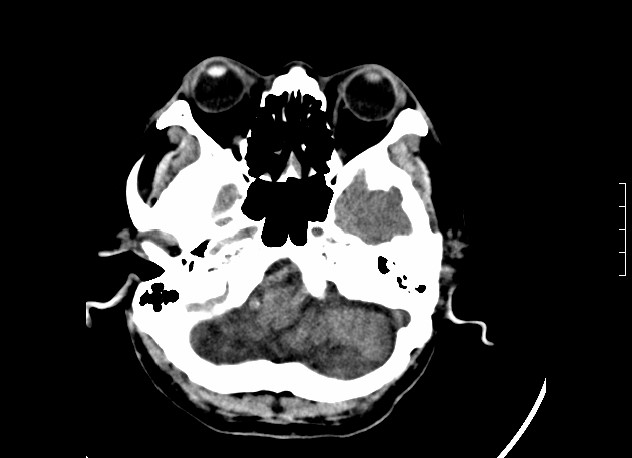
Figure 17: A repeat CT scan after 72 hours showing the crossing of the right vertebral artery.
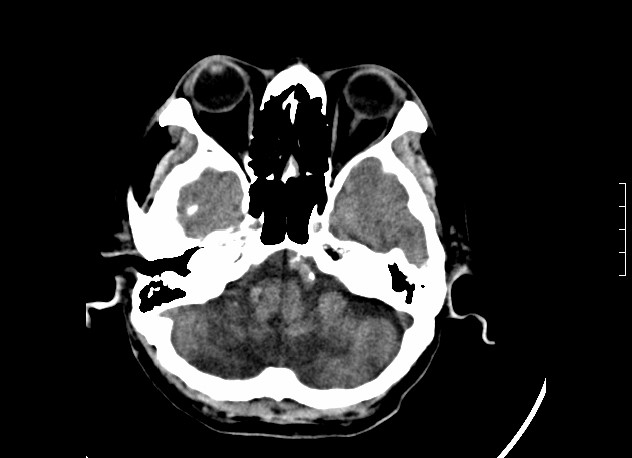
Figure 18: A repeat CT scan after 72 hours showing the curved basilar artery (occluded basilar artery). The second structure became calcified in 72 hours.

Figure 19: A repeat CT scan after 72 hours showing dilated 4th ventricle.
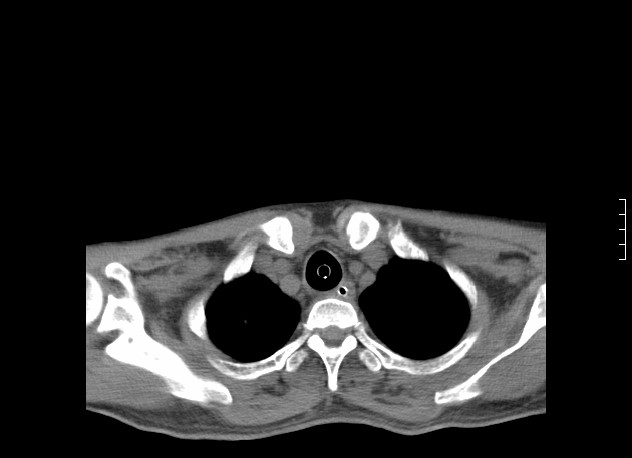
Figure 20: A CT chest shows the nasogastric tube more inferior in the esophagus and the ventilator placed in the respiratory pathway superior (mediastinal window).

Figure 21: A CT scan shows aspiration pneumonia affecting both lung due to aspirating the stomach contents when the patient lost his conscious.
The second case of chronic headache
A sixty-nine-year-old male patient who suffers from a severe headache for many years. He has no health issue or chronic disease. A CT scan was done for him and his CT scan showed a normal finding except an enlarged calcified basilar artery. The vertebral arteries appear non-tortious and non−curved. The diameter of the basilar artery is below the required width of the basilar artery dolichoectasia (below 4.5 mm). The basilar artery appears dense more than the brainstem on the CT scan see (figure 22 through 26).

Figure 22: The vertebral arteries are not tortious, but the right vertebral artery look more centralized.
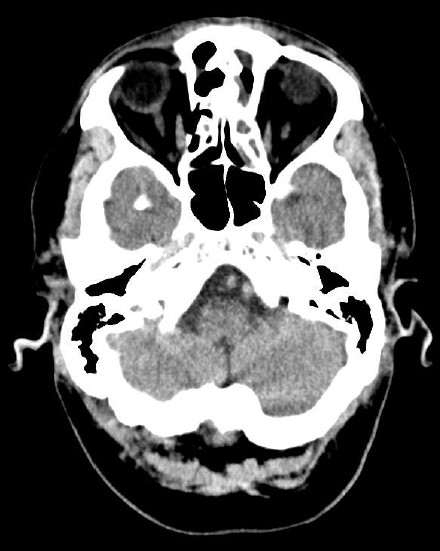
Figure 23: Both vertebral arteries are not curved, but the right vertebral artery located more centralized and anterior to the brainstem.
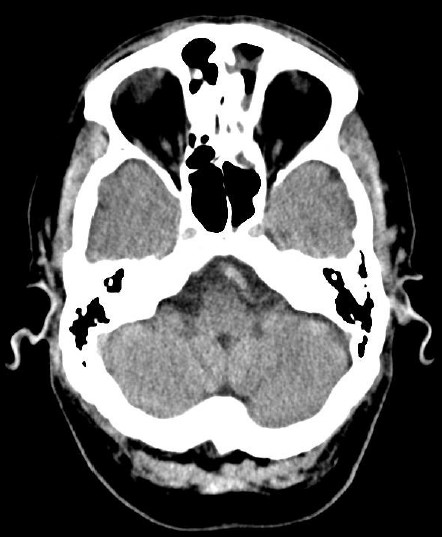
Figure 24: The basilar artery appears calcified, curved, and crossing from the left side to the right side.

Figure 25: The basilar artery located on the right-side posterior to the Sella.

Figure 26: The basilar artery re-crosses to the left side.
Third case of a curved calcified artery causing headache
A seventy-year-old female patient suffers from a severe headache for 2 years. She has no health issue or hypertension. The patient visited the ER multiple times and no abnormal findings were noticed on her CT scans. The basilar artery was considered normal because the dolichoectasia criteria that the basilar artery diameter must be above 4.5 mm which this case does not fit in. The CT scan shows the basilar artery surrounding and compressing the brainstem. A three measurements were taken from the most dilated parts on the CT scan and the biggest part measured 4.48 mm see (figure 27).

Figure 27: A brain CT scan shows the basilar artery partially calcified, curved, surrounding the brainstem. The diameter is below 4.5 mm which does not fit with dolichoectasia on three measurements (1st measurement = 4.47 mm, 2nd measurement = 4.42 mm, and 3rd measurement = 4.18 mm).
Arterial calcification criteria
Vascular calcification is classified based on different mechanisms and affected layer. Atherosclerosis is accumulation of lipid, inflammation, fibrosis, plaques which will result in affecting the intima layer of the artery (endothelium) which will narrow the artery and cause a clot [2]. Arteriosclerosis will calcify the artery wall usually is metabolic or age-related condition that affect tunica media layer of the artery (muscle and elastic fiber layer) which will result in arterial stiffness [2]. Therefore, the artery stiffness is caused by arteriosclerosis not atherosclerosis [2]. There is not published criteria to define which artery is calcified, but there is a criteria of coronary arteries calcification which considered a calcified coronary artery to have above 130 Hounsfield units on a CT scan [3]. Due to the location of the coronary artery, it needs a high number to be considered calcified, but it could be 100 Hounsfield units in case of a basilar artery or any intracranial arterial calcification because it’s not closes to the heart like coronary arteries. To consider any cranial artery calcified, it must have above 100 Hounsfield units on a CT scan. An atherosclerotic artery will not have that score (i.e., 100 Hounsfield units). Therefore, any atherosclerotic artery is not considered calcified.
Dolichoectasia vs. basilar neuralgia
Dolichoectasia is a vague broad general term used to describe any elongated and dilated artery. It is usually associated with normal basilar artery. It is asymptomatic most of the time. It has a criterion in the basilar artery to considered a basilar artery dolichoectasia which to have a diameter above 4.5 mm. The basilar artery can be tortious in case of dolichoectasia. Dolichoectasia can be caused by dissection. Dolichoectasia can be symptomatic & asymptomatic, atherosclerotic & non-atherosclerotic, cause neurovascular compression syndrome & be normal anatomical variation, cause death & cause no harm, have a normal basilar artery & have a very tortious basilar artery, etc. All the previously mentioned criteria of dolichoectasia does not make any sense. It makes a very normal patient in the same category with brain death patient by using this term. Therefore, another accurate criterion must be made to separate patient who have anatomical variations in the brain vasculature from symptomatic patients who could have infarctions and brain death. Basilar neuralgia is a new term described by the author of this paper to distinguish sick patients from normal individuals. Basilar neuralgia patients will be symptomatic. Basilar neuralgia can cause neurovascular compression on any cranial nerve (3rd, 5th, 6th, 7th, and 8th) and on the brainstem. It does not need the vertebral artery to be curved or tortious. It must be calcified fully or partially due to hypertension or ageing process. Basilar neuralgia has a classic “S” shaped course. Compared to dolichoectasia, basilar neuralgia will cause dissection, occlusions, infarctions, and brain death.
Basilar neuralgia criteria
It must be fully or partially calcified or atherosclerotic due to ageing process or hypertension. The basilar artery must be curved and crossing from one side to another side of the brainstem outside the pre-pontine groove. One of the vertebral arteries must be crossing to the other side of the brainstem. One of the vertebral arteries must be dominant. The basilar artery must be dilated see (figure 27). It’s can come with tortious or calcified vertebral arteries. Basilar neuralgia can cause chronic headache, cerebrovascular accident (CVA), basilar artery dissection, basilar artery occlusion, locked in syndrome, etc. The basilar artery mostly affects geriatric patients, but it can affect hypertension patients who are below 50-year-old as well. A basilar artery must score 100 Hounsfield units on a CT scan.
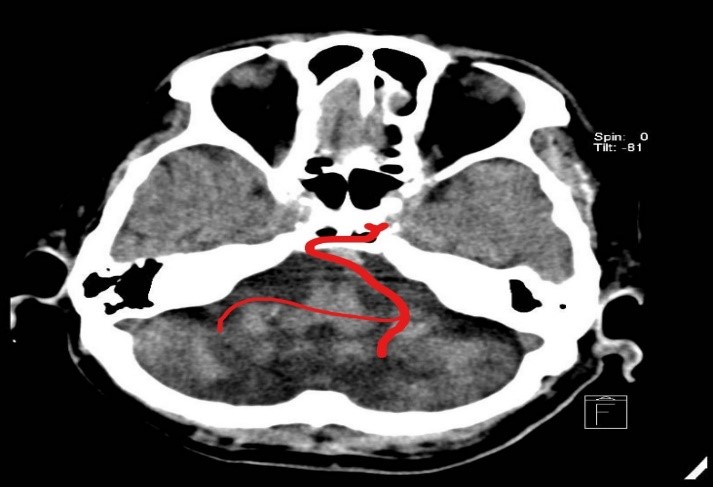
Figure 28: An illustration of the basilar artery and vertebral arteries course (on a CT scan) in a basilar neuralgia case. The dominant vertebral artery on the left side continue on the same course to become a basilar artery after joining of the non-dominant right vertebral artery ass illustrated. The basilar artery is curved like “S” shape and hyper-dense more than the surrounding soft tissue.
Discussion
All the two previously published cases and the three reported cases in this paper, have a dominant left vertebral artery which could be an indication of the dominant left hemisphere. There are two cases published previously and 3 cases in this paper about this topic which all do not fit with dolichoectasia criteria including; all the 5 cases have a diameter smaller than 4.5 mm, un-tortious vertebral arteries (but one dominant vertebral artery and another one crossing to the opposite side), calcifications, “S” shaped basilar artery, all have a left dominant vertebral artery, and all cases are symptomatic [4,5]. Smoker’s criteria for basilar dolichoectasia required the basilar artery to be dilated above 4.5 mm and any artery below 4.5 mm is a normal artery according to Smoker’s criteria. Based on smoker’s criteria all the reported cases of basilar occlusion and chronic headache does not fit in the criteria which ignore personalized medicine approach. Based on a published review not all the patients are the same in terms of sizes of the cranial arteries diameter [6]. In addition, Smoker’s criteria must be applied on a CTA or MRI. It’s alleged to be an accurate criterion for the vertebrobasilar system only and can’t be used for other cranial arteries [7]. This criterion was proposed in 1986 and it obviously does not work.
Conclusion
Basilar neuralgia is an accurate term describes a specific condition that affect the basilar artery which could lead to serious consequences like basilar artery occlusion, infarction, brain death, neurovascular compression syndrome, and chronic headache which affect life quality. Dolichoectasia should be used for normal anatomical variations that has no effect.
References
1. Rhodes CE, Kelleher T, Plamoottil CI. 2020. A Case Report of Basilar Artery Occlusion in a Healthy 36-Year-Old Female. Cureus, 12: 8904. Ref.: https://pubmed.ncbi.nlm.nih.gov/32742871/
2. Mackey RH, Venkitachalam L, Sutton-Tyrrell K. 2007. Calcifications, arterial stiffness and atherosclerosis. In Atherosclerosis, Large Arteries and Cardiovascular Risk. 44: 234-244. Ref.: https://pubmed.ncbi.nlm.nih.gov/17075212/
3. Rennenberg RJ, Schurgers LJ, Kroon AA, et al. 2010. Arterial calcifications. Journal of cellular and molecular medicine, 14: 2203-2210. Ref.: https://pubmed.ncbi.nlm.nih.gov/20716128/
4. Alahmari A. 2020. Giant Curved Calcified Basilar Artery Causing Headache: A Case Report. Clin Res Neurol. 3: 1-4.
5. Alahmari AA. 2020. Second Case of Giant Atherosclerotic Basilar Artery Causing Headache: A Case Report. 3: 1-3.
6. Alahmari A. 2020. Cross-sectional angiographic imaging of anatomical variations in the circle of Willis: A literature review. Eur. J. Anat. 24: 297-309.
7. Gutierrez J, Sacco RL, Wright CB. 2011. Dolichoectasia-an evolving arterial disease. Nature Reviews Neurology. 7: 41-50. Ref.: https://pubmed.ncbi.nlm.nih.gov/21221115/




















