Indexing & Abstracting
Full Text
Research ArticleDOI Number : 10.36811/ojrmi.2020.110010Article Views : 110Article Downloads : 59
Impact of COVID-19 on the volume of emergency CT studies in a neuro-trauma reference center
José Pablo Martínez-Barbero1* and Rosa Macías-Ruíz2
and Rosa Macías-Ruíz2
1Neuroradiologist. MD. PhD. EDiNR. Neuroimaging section. Hospital Universitario Virgen de las Nieves, Granada, Spain
2Cardiologist. MD. PhD. Hospital Universitario Virgen de las Nieves, Granada, Spain
*Corresponding Author: José Pablo Martínez-Barbero Neuroradiologist. MD. PhD. EDiNR. Neuroimaging section. Hospital Universitario Virgen de las Nieves, Granada, Spain. Tel: +34 625207879; Email: jpmbhg@hotmail.com
Article Information
Aritcle Type: Research Article
Citation: José Pablo Martínez-Barbero, Rosa Macías-Ruíz. 2020. Impact of COVID-19 on the volume of emergency CT studies in a neuro-trauma reference center. O J Radio Med Img. 3: 38-45.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2020; José Pablo Martínez-Barbero
Publication history:
Received date: 02 October, 2020Accepted date: 09 October, 2020
Published date: 12 October, 2020
Abstract
Rationale and Objectives
The covid-19 pandemic has been a challenge for health systems, given the large number of affected patients and mortality rates. However, it has conditioned a decrease in non-covid imaging studies. Our intention is to quantify the decrease in emergency neuroimaging studies caused by the pandemic.
Materials and Methods
A retrospective study was carried out on the number of CTs requested from the emergency department. The total amount of CT performed, brain-CT, and the CT studies for stroke code were quantified, week by week. The analogous weeks of 2019 and 2020, before and after the declaration of the state of alarm, were compared.
Results
The total amount of CTs requested from the ED during 2020 in weeks 1-12 was 1266, and decreased compared with 1745 exams during weeks 1-12 in 2019 (p value 0.045). During weeks 1-12 in 2020, 947 brain-CTs were performed, compared to 1328 in 2019 (p value 0.032). When comparing the 1-6 weeks in 2020 with those affected by the pandemic, a decrease was observed from 887 emergency CTs to 419 (p value 0.002). There was a decrease (p value 0.002) in the number of brain-CTs, from 664 in weeks 1-6, to 303 in weeks 7-12. No statistically significant differences were found in the number of stroke code studies.
Conclusion
The COVID-19 pandemic has led to a huge drop in urgent imaging studies during the state of alarm at a reference neurotrauma center, except for stroke code studies.
Keywords: Covid-19; Neuroimaging; Stroke imaging; Emergency imaging; CT
Introduction
The SARS-COVID-19 pandemic, initially described by Zhu et al [1], has posed a challenge for health systems around the world during the first half of 2020. In Spain, at present, it has affected at least to 250,545 people, confirmed by PCR, with 28385 confirmed deaths [2]. In the Andalusia region, on 4th July /2020, there were 18,065 confirmed patients and 1,441 deaths. In the province of Granada, where our health area is located, 3392 confirmed patients and 287 deceased had been counted [3]. The pandemic has conditioned major changes in healthcare in the world's most shaved regions, causing changes in the structure of services and in their ability to provide healthcare [4]. In medical imaging services, the pandemic has caused an enormous alteration, both in the provision of health care due to the need to adapt the facilities, and in training and research [5,6]. In addition, changes in patient flows are forcing imaging services and societies to make contingency plans in order to, on the one hand, attend to new patients affected by SARS-COVID-19 and, on the other, rethink the assistance of other patients [7,8]. The economic prospects of doctors and imaging companies have also been affected, since they foresee a great decrease in their healthcare volume [9]. However, despite the worrying figures of the pandemic, there are different studies that show that health assistance for other causes have experienced a sharp decline, just as difficulties have arisen in the provision of assistance services. As examples, the Hong Kong study by Tam and others [10] demonstrated an evident decrease in the number of primary angioplasties during the weeks of the pandemic, as well as a delay in seeking assistance from the time of symptom onset. A similar phenomenon has been described in a Spanish multicenter study on coronary angioplasties during the state of alarm, detecting a decrease in the number of coronary therapeutic procedures of up to 48% [11]. Likewise, significant decreases have been reported in the attendance of patients to emergencies for non-COVID pathologies in the United Kingdom of up to 25% [12]. The number of patients with strokes, as well as the number of treatments for recanalization, has also decreased markedly [13,14], and concerns have been raised about the patients' refusal to request assistance [15,16]. In the field of medical imaging, the decrease in healthcare has also been notable. Thus, an international study carried out through a survey on the activity of nuclear medicine services has shown that 90% of the services consulted have experienced a decrease in diagnostic procedures of more than 20% [17]. This decrease has also affected the number of Computerized Tomography (CT) scans performed in the emergency services for non-covid pathologies, with decreases of up to 61% [18]; as well as with falls greater than 40% in the programmed and urgent studies according to the data provided by companies in the sector [19]. Furthermore, the study by Naidich et al. showed a significant decrease in the volume of imaging studies in their group, with a total decrease of 28.10% during the pandemic. The decrease reached up to 45.56%, 4.15%, and 87.55% for emergency department, inpatient, and outpatient imaging respectively at the last week of those included in their study [20]. In addition, the study by Vagal [21] et al demonstrated a significant decrease in overall imaging volume (53.4%) as compared to same period in 2019, as well as a decrease in imaging in the inpatient (40.5%) and emergency department (ED) (48.9%) settings. Given the impact of the pandemic on volume in medical imaging services, the objective of this paper is to assess the impact of COVID-19 on the volume of CT imaging studies in the ED at our hospital, analyzing it week by week during the pandemic, and its comparison with the previous year and this year's pre-pandemic period.
Material and Methods
A retrospective review of the CT scans performed in our hospital and requested from the ED was made, in a weekly basis. It was considered for study as the period most severely affected by the pandemic from March 16, 2020, when the state of alarm was declared, to April 26, 2020, when the most severe restrictions on mobility were lifted after an evident improvement in the figures for the pandemic in Spain. The pre-pandemic period was defined from February 3 to March 15, 2020. In order to be able to compare with the previous year, we used as references with the pre-pandemic period from February 4 to March 17, 2019, and as a reference with the pandemic period from March 18 to April 28, 2019. The ethics committee of our institution approved the performance of this retrospective study. Our center is reference for neuro traumatological pathology in our region, and only patients with acute neurological, traumatic and neck pathology are admitted at the ED. We have a CT at the ED, and another CT that normally performs inpatients and outpatients, but during the alarm period it was reserved for COVID-19 suspicious patients, as part of an specific circuit. For the analysis carried out, all the CT requested from the ED were considered, regardless of the CT where they were performed. Imaging studies were grouped for analysis into 3 categories: total amount of CT studies requested from the ED, brain-CT requested from the ED, and CT studies for stroke code, which included in addition brain CT-perfusion and CT-angio of supra-aortic vessels and circle of Willis. The dataset was split for analysis to compare the pre-COVID-19 period in 2020 (weeks 1-6) and post-COVID period in 2020 (weeks 7-12). In the 2019 data, weeks were adjusted to match with 2020 workweeks in Spain (Monday to Sunday), and data were also splitted into two periods, parallel to the pre and post-COVID in 2020. Easter week, whose exact date varies each year depending on the religious calendar, was included in both 2019 and 2020 in weeks 7-12, which allowed avoiding biases, since a decrease in the influx of patients is usually observed. A comparison was made between the pre-COVID data in 2020 and the analogous weeks in 2019, to verify that there was no relevant difference in the number of cases between years that could have biases the results of our study. The frequency data for each week was summed for the total weeks 1-12 in 2019 and 2020, differentiating pre-COVID-19 and post-COVID-19 periods according to imaging modality. Descriptive frequency data was plotted to demonstrate the trend in the weekly imaging case volumes in 2020. The percent difference between imaging case volumes was calculated by week for the total weeks 1-12, pre- COVID-19 and post-COVID-19 periods, compared to the 2019 imaging volumes, stratified by imaging modality. The differences in the imaging volumes in the 2020 calendar year were compared to the same weeks in 2019 to assess the degree of change accounting for monthly or seasonal variation within the same calendar year. The mean weekly imaging volumes were calculated for each imaging modality for the total weeks 1-12, pre-COVID-19 and post-COVID-19 periods in 2020 and analogue weeks in 2019. Statistical analysis Independent-samples t-tests were performed comparing the mean weekly imaging case volumes in year 2020 and 2019 for each imaging modality type stratified by patient service locations for the total weeks 1-16, pre-COVID-19 and post-COVID-19 periods. Statistical significance was considered for p-values <0.05. All statistical analyses were performed using SPSS v26.0.
Results
The total amount of CTs performed at our institution and requested from the ED during 2020 in weeks 1-12was 1266 with an average of 108.8studies per week, and experienced an obvious drop compared with 1745 exams during weeks 1-12 in 2019, when 145studies were carried out on average, per week (Figure 1). The difference was statistically significant (p value 0.045). During weeks 1-12 in 2020, 947 brain-CTs were performed, compared to 1328 in 2019.A statistically significant difference was found (p value 0.032). In contrast, no significant differences were detected in the number of CT studies for stroke code, despite a slight decrease (Table 1).
|
Table 1: Comparison of the number of CTs requested from the ED and performed in 2019 and 2020 during the total period of the study (12 weeks). Values ??expressed as mean ± standard deviation. |
||||
|
Total amount of CT studies |
145,4 ±18,1 |
108,8±44,1 |
0,045 |
1,0-72,2 |
|
Brain-CT studies |
110,7 ±15,9 |
78,9 ±32,8 |
0,032 |
3,3-60,2 |
|
Stroke code CT studies |
9,2 ±3,1 |
7,9 ±2,9 |
0,388 |
-1,9-4,6 |
No differences were found in the comparison between weeks 1-6 of 2019 and 2020 (Table 2).
|
Table 2: Comparison of the number of CTs requested from the ED and performed in 2019 and 2020 during the pre-alarm period of the study (weeks 1-6). Values ??expressed as mean ± standard deviation. |
||||
|
2019 weeks 1-6 |
2020 weeks 1-6 |
P value |
CI 95% |
|
|
Total amount of CT studies |
138,5 ± 9,2 |
147,8 ± 20,9 |
0,420 |
-36,6-18,0 |
|
Brain-CT studies |
102,8 ± 19,5 |
107,3 ± 19,5 |
0,703 |
-33,1-24,1 |
|
Stroke code CT studies |
9,5 ± 3,3 |
9,3 ± 3,3 |
0,949 |
-6,2-6,5 |
Regarding the period affected by the COVID-19 pandemic (weeks 7-12), during 2020, 419 urgent CT scans were performed. In comparison, during 2019 at weeks 7-12, 914 urgent CT scans were performed. A statistically significant difference was found (p value 0.002). During pandemic period in 2020, 303 brain- CT´s were performed. In comparison, during 2019 at weeks 7-12, 711 brain-CT scans were made. A statistically significant difference was found (p value 0.001). CT stroke code studies decreased from 54 studies in 2019 to 39 studies in 2020 during weeks 7-12, but no significant difference was found (Table 3).
|
Table 3: Comparison of the number of CTs requested from the ED and performed in 2019 and 2020 during the state of alarm (weeks 7-12). Values ??expressed as mean ± standard deviation. |
||||
|
2019 weeks 7-12 |
2020 weeks 7-12 |
P value |
CI 95% |
|
|
Total amount of CT studies |
152,3 ±22,7 |
69,8 ±14,2 |
0,002 |
46,7-118,3 |
|
Brain-CT studies |
118,5 ±18,0 |
50,5 ±6,6 |
0,001 |
44,5-91,5 |
|
Stroke code CT studies |
9,0 ±3,2 |
6,5 ±1,9 |
0,212 |
-2,0-7,0 |
When comparing the 6 weeks prior to the state of alarm in 2020 with those affected by the pandemic, an evident decrease was observed from 887 emergency CT scans to 419, with a statistically significant difference (p value 0.002). There was also an evident statistically significant decrease (p value 0.002) in the number of brain CTs performed, from 664 in weeks 1-6 of the study, to 303 in weeks 7-12. No statistically significant differences were found in the number of studies by stroke code, although the total number decreased slightly from 56 to 39 (Table 4).
|
Table 4: Comparison of the number of CTs requested from the ED and performed in 2020 before and during the state of alarm (weeks1-6 vs weeks 7-12). Values ??expressed as mean ± standard deviation. |
||||
|
2020 weeks 1-6 |
2020 weeks 7-12 |
P value |
CI 95% |
|
|
Total amount of CT studies |
147,8 ±20,9 |
69,8 ±14,2 |
0,002 |
45,0-111,0 |
|
Brain-CT studies |
107,3 ±19,5 |
50,5 ±6,6 |
0,002 |
31,7-82,0 |
|
Stroke code CT studies |
9,3 ±3,3 |
6,5 ±1,9 |
0,095 |
-0,7-6,4 |
Regarding the week-by-week results, figure 1 shows the total numbers of emergency CT scans performed in 2019 and 2020 during the 12 weeks of the study, and Figure.2 shows brain- CT studies. As can be seen, the maximum fall occurred in week 7 of the study, the first week of the state of alarm, in which only 49 emergency CT scans were performed, of which 41 were brain-CT. In comparison, in the previous week in 2019, 111 emergency CT scans were performed, of which 71 were brain- CTs, and in week 7 of 2019, 164 emergency CT scans, of which 124 were brain studies.
Discussion
The results of our study show a significant decrease in emergency CT studies in our center, a reference in neuro-traumatic pathology, during the period of greatest affectation due to the pandemic in our health area, compared to the previous year and to the pre-pandemic period of 2020, data consistent with others published in the literature. The decrease was especially severe in the first weeks of the state of alarm both in the set of emergency CT scans (Figure 1) and specifically, in the brain CT scans (Figure 2), with a gradual recovery. On the other hand, in the studies by stroke code, although there was a slight decrease, the difference was not significant.
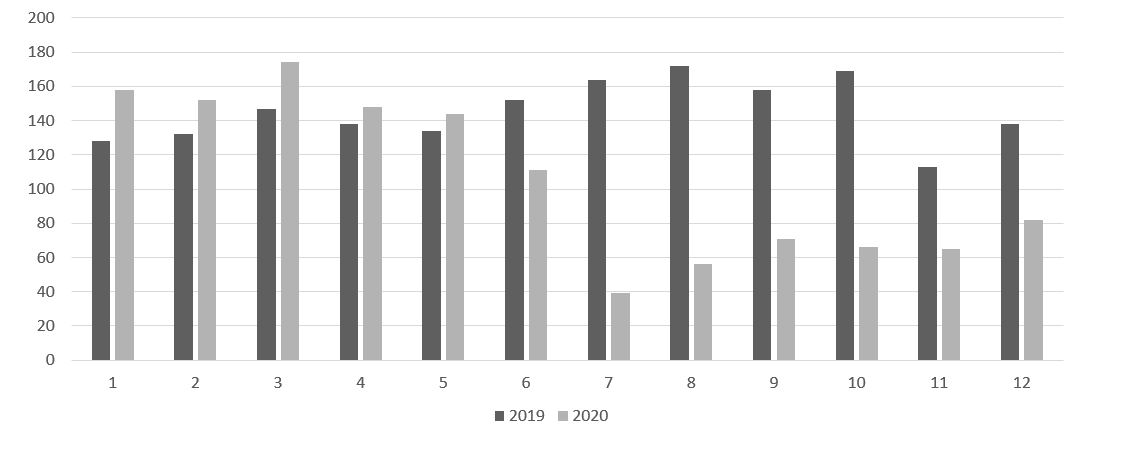
Figure 1: Number of CT performed and requested from the emergency service, week by week, comparing 2019 (dark grey) and 2020 (light grey).

Figure 2: Figure 1. Number of Brain-CT studies performed and requested from the emergency service, week by week, comparing 2019 (dark grey) and 2020 (light grey).
Naidich et al. study [20] detected a 45% decrease in the overall number of emergency CT scans, a figure similar to that shown in our study. The study by Vagal et al [21] showed a decrease in ED imaging studies over 40 %, in an amount similar to that detected in ours. The study by Boeke et al. [18] depicted a decrease of 60% in the CT of ED, superior to ours, but they only considered the period of March 16- 30, the most severely affected by the restrictions. If we exclusively compare the first weeks of the state of alarm (weeks 7-8, Figures 1 and 2), the decline in studies at our institution is comparable to theirs. The decrease in the overall number of emergency CT studies may be due, on the one hand, to a lower prevalence of traumatic pathology. For example, during the state of alarm, construction works were suspended, with the consequent disappearance of work accidents suffered by bricklayers. Furthermore, the reduction in road traffic has probably led to a notable decrease in traffic accidents. However, there are hardly any quality studies that have quantified the decrease in brain CT studies, the most frequent sectional imaging test in our setting. This study has shown that it suffered a significant decline both in comparison with 2019 and with the pre-covid period of 2020, with a great decline from a weekly average in 2019 of 110 studies to only 41 studies in the first week of the alarm state. The sharpest decline occurred in the first week of confinement, and then gradually increased, in parallel with the withdrawal of the most severe measures of social distancing. One of the concerns in the healthcare field in relation to the side effects of covid is the lack of confidence in the safety of the population's healthcare facilities, which could mean a decrease in requests for assistance and a delay in it, as in fact it has been demonstrated in the case of coronary syndromes [10,11] and stroke [14,22]. The enormous decrease in the influx of patients to the emergency services for non-covid pathology may be due in part to this loss of confidence, and that should not be a relevant problem for less serious pathologies such as migraine or osteoarticular pain, which they are a frequent cause of emergency healthcare, although of low potential severity in most cases. We consider that a significant number of the cranial CT studies not performed are due to patients with pathology of this nature who decided not to go to the emergency room. However, the greatest health impact due to the loss of care could occur in patients who, suffering from more serious pathologies, decided not to go to the emergency room. Within this group, our study highlights stroke patients. The studies by stroke code suffered a slight decrease with respect to the periods of normality, but without reaching a statistically significant difference, from an average of 9 studies in weeks 6-12 of 2019 and 9.3 studies in weeks 6-12 of 2020 to an average of 6.5 in weeks 6-12 of 2020. This decrease implies that there was probably a lower request for assistance, but with a less relevant drop than in other centers. Cases of stroke secondary to the pro-thrombotic state of covid have recently been published [23,24]. and this may have led to a higher prevalence of the disease that has supplied less emergency care for other causes. Unfortunately, we have not yet been able to have specific data on this in our environment. Despite the consistency of our results, we consider that the study has a number of weaknesses. On the one hand, it is a retrospective study. In addition, due to the nature of our center, we have focused on neuro trauma imaging studies, so we cannot assess whether the pandemic has led to a change in chest or abdomen studies. Likewise, we have not been able to assess the content of the radiological studies, so we do not know if the percentage of studies with pathology has changed.
Conclusion
The Covid-19 pandemic has been, and continues to be, a challenge for health systems around the world, with major changes in the flow of patients. In our referral center in neurotraumatological pathology, it has implied a great decrease in the number of urgent CT studies, especially evident in the skull CT, compared to the pre-pandemic periods. Subsequent studies should determine if there has been less pathology, or patients still with CNS pathology have not attended the emergency room, with the potential damage to their health that this would entail.
References
1. Zhu N, Zhang D, Wang W, et al. 2020. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 382: 727-733. Ref.: https://pubmed.ncbi.nlm.nih.gov/31978945/
2. Ministerio de Sanidad. Situación del COVID-19 en España Available from: https://cnecovid.isciii.es/covid19/. 2020. Accessed June 1, 2020.
3. Servicio Andaluz de Salud. Informe COVID-19 en Andalucía.
4. Maniscalco P, Poggiali E, Quattrini F, et al. 2020. The deep impact of novel CoVID-19 infection in an Orthopedics and Traumatology Department: the experience of the Piacenza Hospital. Acta Biome. 91: 97-105. Ref.: https://pubmed.ncbi.nlm.nih.gov/32420933/
5. Gholamrezanezhad A. 2020. COVID-19 Precautions : What the MRI Suite Should Know. J Am Coll Radiol. Epub ahead of print. Ref.: https://pubmed.ncbi.nlm.nih.gov/32473107/
6. Alvin MD, George E, Deng F, et al. 2020. The Impact of COVID-19 on Radiology Trainees. Radiology. 201222. Ref.: https://pubmed.ncbi.nlm.nih.gov/32216719/
7. Laghi A, Grassi R. 2020. Italian Radiology’s Response to the COVID-19 Outbreak. J Am Coll Radiol. 1440: 30406. Ref.: https://pubmed.ncbi.nlm.nih.gov/32348740/
8. Quraishi MI, Rizvi AA, Heidel RE. 2020. Off-Site Radiology Workflow Changes Due to the COVID19 Pandemic. J Am Coll Radiol. 5-8. Ref.: https://pubmed.ncbi.nlm.nih.gov/32425711/
9. Cavallo JJ, Forman HP. 2020. The Economic Impact of the COVID-19 Pandemic on Radiology Practices. Radiology. 06520: 201495. Ref.: https://pubmed.ncbi.nlm.nih.gov/32293225/
10. Tam CCF, Cheung KS, Lam S, et al. 2020. Impact of Coronavirus Disease 2019 (COVID-19) Outbreak on ST-Segment-Elevation Myocardial Infarction Care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2019: 2019-2021. Ref.: https://pubmed.ncbi.nlm.nih.gov/32182131/
11. Rodríguez-Leor O, Cid-Álvarez B, Ojeda S, et al. 2020. Impact of the COVID-19 pandemic on interventional cardiology activity in Spain. REC Interv Cardiol (English Ed. 2: 82-89.
12. Thornton J. 2020. Covid-19: A&E visits in England fall by 25% in week after lockdown. BMJ. 369: 1401. Ref.: https://pubmed.ncbi.nlm.nih.gov/32253175/
13. Thornton J. 2020. Stroke: “striking reductions” are seen in number of people with symptoms seeking help. BMJ. 369: 1406. Ref.: https://pubmed.ncbi.nlm.nih.gov/32253176/
14. Markus HS, Brainin M. 2020. EXPRESS: COVID-19 and Stroke - A Global World Stroke Organisation perspective. Int J stroke. 15: 361-364. Ref.: https://pubmed.ncbi.nlm.nih.gov/32310017/
15. Derraz I. 2020. Stroke Health Care Use and COVID-19. AJNR Am J Neuroradiol. 6563. Ref.: https://pubmed.ncbi.nlm.nih.gov/32381538/
16. Zhao J, Rudd A, Liu R. 2020. Challenges and Potential Solutions of Stroke Care During the Coronavirus Disease 2019 (COVID-19) Outbreak. Stroke. 51: 1356-1357. Ref.: https://pubmed.ncbi.nlm.nih.gov/32228369/
17. Annunziata S, Bauckneht M, Albano D, et al. 2020. Impact of the COVID-19 pandemic in nuclear medicine departments: preliminary report of the first international survey. Eur J Nucl Med Mol Imaging. Epub ahead of print. Ref.: https://pubmed.ncbi.nlm.nih.gov/32462398/
18. Boeken T, Berre A Le, Mebazaa A, et al. 2020. Non-COVID-19 emergencies : where have all the patients gone ? Eur Radiol. 1-2. Ref.: https://pubmed.ncbi.nlm.nih.gov/32458174/
19. Walach E. 2020. COVID-19 IMPACT ON CT IMAGING VOLUME.
20. Naidich JJ, Boltyenkov A, Wang JJ, et al. 2020. Impact of the COVID-19 Pandemic on Imaging Case Volumes. J Am Coll Radiol. Epub ahead of print. Ref.: https://pubmed.ncbi.nlm.nih.gov/32425710/
21. Vagal A, Mahoney M, Allen B, et al. 2020. Rescheduling Non- Urgent Care in Radiology: Implementation during the COVID-19 Pandemic. J Am Coll Radiol . Epub ahead of print. Ref.: https://pubmed.ncbi.nlm.nih.gov/32473108/
22. Rudilosso S, Laredo C, Vera V, et al. 2020. Acute Stroke Care Is at Risk in the Era of COVID-19. Stroke. 51: 1-5. Ref.: https://pubmed.ncbi.nlm.nih.gov/32438895/
23. Medeiros BC. 2020. Large-Vessel Stroke as a Presenting Feature of Covid-19 in the Young. new engl J Med. 382: 60-63. Ref.: https://pubmed.ncbi.nlm.nih.gov/32343504/
24. Berekashvili K, Dmytriw AA, Vulkanov V, et al. 2020. Etiologic Subtypes of Ischemic Stroke in SARS-COV-2 Virus patients in a cohort of New York City hospitals. 1. Epub ahead of print.




















