Indexing & Abstracting
Full Text
Research ArticleDOI Number : 10.36811/ojprm.2020.110010Article Views : 3Article Downloads : 0
Commonsense Approaches to Minimizing Risks from COVID-19
Sunil J. Wimalawansa, MD, PhD, MBA, FACP, FRCP, FRCPath, DSc
Professor of Medicine, Endocrinology & Nutrition, Cardiometabolic and Endocrine Institute, N.J, USA
*Corresponding Author: Sunil J. Wimalawansa, Professor of Medicine 661 Darmody Avenue, North Brunswick, NJ 08902, Endocrinology & Nutrition, Cardiometabolic and Endocrine Institute, N.J, USA, Email: suniljw@hotmail.com
Article Information
Aritcle Type: Research Article
Citation: Sunil J. Wimalawansa. 2020. Commonsense Approaches to Minimizing Risks from COVID-19. Open J Pulm Respir Med. 2: 28-37.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2020; Sunil J. Wimalawansa
Publication history:
Received date: 02 October, 2020Accepted date: 13 October, 2020
Published date: 15 October, 2020
Abstract
Coronavirus belongs to a large family of viruses that usually affecting wild animals. COVID-19 is the latest virus from that family transmitted to human in late 2019 but the origin is not conformed. It causes predominantly lower respiratory tract syndrome but also affecting other epithelial cells and other systems such as the cardiovascular system. Approximately, 80% of the spread of COVID-19 is occur through aerosolized form via microdroplets and 80% of the affected are either asymptomatic or having a milder disease. Complications and the rates of deaths from COVID-19 differs from country to country, varying from 0.1 to 3.2%. The fundamental reason for developing serious complications and deaths from COVID-19 is having severe vitamin D deficiency that is associate with weak immune systems. There are no specific, safe, effective, and affordable antiviral or vaccines available yet. Despite claims and hypes, it is unlikely that such would materialize soon. Considering these, the most cost-effective approach to prevent and minimize complications and deaths from COVID-19 is through boosting the immunity through vitamin D adequacy. Meanwhile near total relaxation of public health precautions in certain countries, including allowing crowed gatherings, discouraging the use of face masks, spending time in public places, and allowing unprotected use of crowded public transport systems, failure in adhering to frequently washing hands, etc., (that are necessary for preventing the spread of COVID-19) will be proven as expensive mistakes. This article provides information on the current status of COVID-19 outbreak and commonsense precautions to minimize risks during the current second wave of COVID-19 and future coronaviral pandemics.
Keywords: Angiotensin; Coronavirus; Endocrine; Inflammation;innate immunity; Vitamin D; Pandemic; SARS-CoV-2
Introduction
During the winter, people are much more likely to get influenza B (the flu) than any other viral diseases. Those who have abnormalities in the immune system or who lack optimal immune protection are at a higher risk for contracting viral diseases [1]. There are many public health related precautions that can be taken to minimize the spread of COVID-19; these are somewhat similar to preventing other common viral diseases. Healthy people who are not in close contact with a person with COVID-19 are unlikely to be at risk for severe disease.
Sunlight contains UVA (320-400 nm), UVB (280-315 nm) and UVC (200-260 nm) spectra. Human coronaviruses are RNA viruses are sensitive to ultraviolet (UV) C radiation but not to UVA and UVB. Spectrum of UVC can inactivate coronaviruses, including severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2; COVID-19). Despite this, hardly anyone utilizing this important and cost-effective technology to destroy COVID-19 viruses.
Multiple laboratory studies have revealed that vitamin D is essential for proper functioning of the immune system. In addition, it suppresses excessive inflammatory and oxidative stresses, and regulates the RAS and keep it in balance [2]. Countries with the population serum 25(OH)D concentrations is low and limited availability of ultraviolet-B rays from the sun, have higher COVID-19-related complications and deaths. While COVID-19 is a serious respiratory viral illness, its clinical outcomes can be considered parallel to an extreme influenza epidemic.
Hypovitaminosis D is associate with increased risks and higher prevalence of acute respiratory tract infections [3-5] and supplementation of deficient persons with vitamin D significantly decreases risks of respiratory tract infections. In addition, the vast majority of PCR positive persons, especially those with COVID-associated complications reported to have vitamin D deficiency [5,6]. Many studies reported a strong inverse correlation of serum 25(OH)D concentrations with severity of COVID-19 [3,4]. Although COVID-19 is a viral illness, its manifestations and complications are mostly induced by immunological and endocrinological abnormalities.
Effective of facemasksagainstviruses
A respirator masks, also called disposable particulate respirators, are a verity of personal protective devices that cover the nose and mouth. Some of the face masks however currently sold, unless designed specifically to filter smaller particles such as viruses, are unlikely to prevent the inhalation of COVID-19 or any other virus. Respirator face mask types are rated and certified by the National Institute for Occupational Safety and Health (NIOSH), the CDC, and the Occupational Safety and Health Administration (OSHA). Disposable face masks/respirators are approved by National Institute for Occupational Safety and Health: these are rated as: N = Not resistant to oil; R = Resistant to oil; and P = strongly resistant (oil Proof). These three types of masks can be used to filter virus particles and any other airborne particulate matter, including dust and larger chemical particles. The CDC recommended face mask/respirator in the market, are falls into the following four categories: N95, N99, R95, or R99, based on the percentage efficiency of filtering capacity of particles, such as dust and viruses. Although P100 masks are effective, they are uncomfortable to use in normal travel circumstances. There are several other types of disposable particulate respirators (for more information, please visit https://www.osha.gov/SLTC/etools/respiratory/index.html). For non-infected people, the use of a respirator with an exhalation valve is more tolerable and easier to use. However, the CDC and the WHO failed to recommend wearing face masks for months into the pandemic when one is not in close contact with an infected person or traveling in crowded places.
Common Sense Measures to Prevent Infection
Adhering to infectious disease prevention guide lines against air-borne diseases are insufficient to curtail the COVID-19 spread, as the disease is also spread by asymptomatic carriers. Such principles include avoiding crowded places, employing regular hand washing with soap and water and using medical grade hand sanitizers (an alcohol-based disinfectant that contains at least 60% alcohol), and covering the nose and mouth with disposable tissues or inner elbow when coughing or sneezing etc. While, the primordial prevention eliminates risk factors, primary prevention reduces risks of exposure. Additional actions one could take to minimize infections are described on the CDC website [7]. Coronaviruses have the capacity to enter the body through any mucosal surface. Therefore, one should not touch with contaminated fingers, eyes, nose, or mouth, without first washing hands/figures thoroughly. Therefore, it is advisable to wash hands thoroughly with soap and water for when returning home. Measures such as staying at home when one has flu-like symptoms and/or an unexplained fever and keeping distance from people who have signs sofa respiratory tract infection, including runny nose, coughing, and sneezing, should be followed to minimize the risks of respiratory viral diseases.
Similar to COVID-19, highly infectious viral diseases, such as measles and chicken pox, and certain bacterial infections, such as tuberculosis, also have an air borne spread of the disease. These organisms that can travel distance in micro-droplets in air, that can reach up to 100 feet, and therefore, could infect people in a longer distance, than with COVID-19. Other viruses, such as HIV and hepatitis, are transmitted only through direct contact with the bodily fluids of an infected person. Figure 1 illustrates the three most important means of reducing the risk of contracting COVID-19.
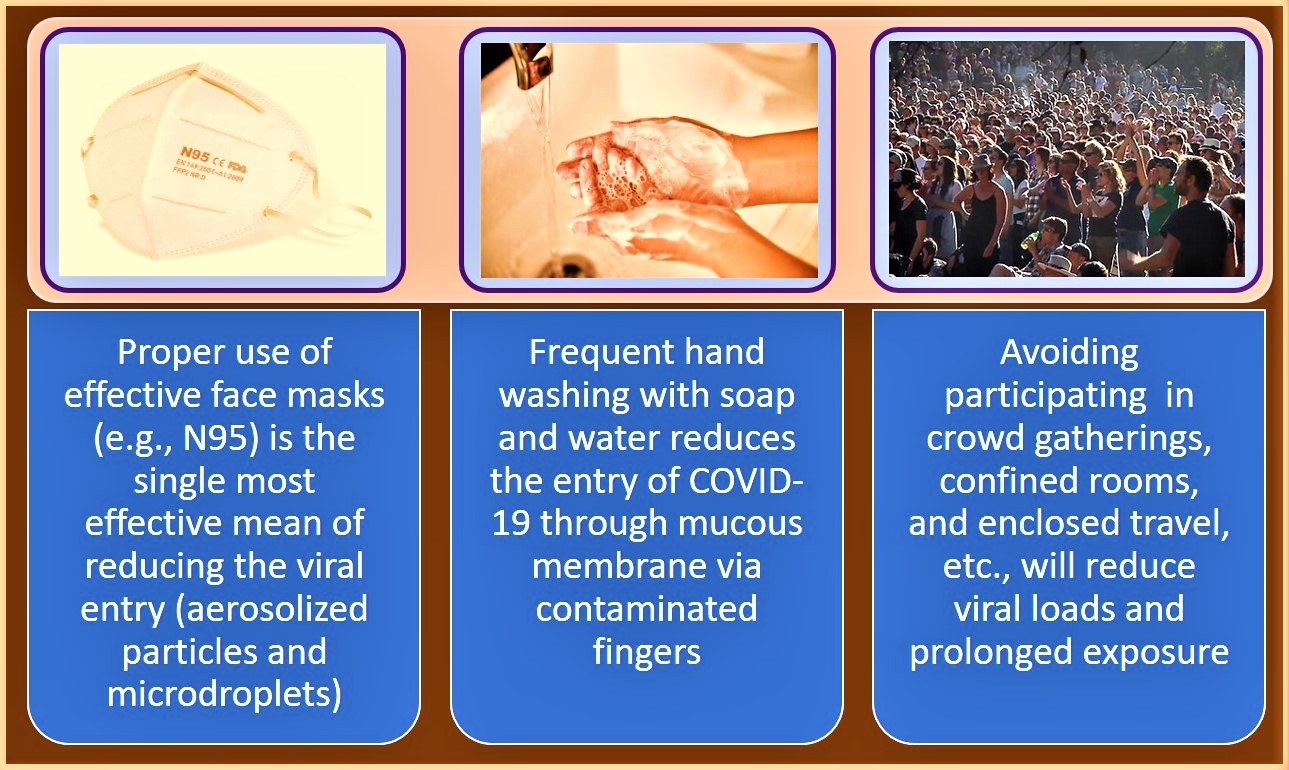
Figure 1: The proper use of face masks with right material, frequent hand washing, and avoiding crowded spaces are the three most important public health measures in reducing the risk of contracting COVID-19.
Wearing face masks reduces viral load in the individual and in the community, thus reducing the likelihood of getting infected and developing complications and reduces the spread of COVID-19. It can also reducing the risks of contracting COVID-19 or acquiring a mild infection that can facilitate the production of antibodies against COVID-19 and development of herd immunity quicker than otherwise would. However, when community serum 25(OH)D concentrations are maintained in excess of 30 ng/mL, many of the public health related community wide restrictions can be relaxed: hence the high importance of maintaining the population vitamin D sufficiency.
Human-to-Human transmission of COVID-19
Human-to-human transmission can be curtailed by taking efficient public health measures, such as well-organized tracking of individuals who had been in contact with an infected person, isolating sick people (quarantine measures), and large-scale public education. Health screening of suspected persons at ports of entry are helpful in the early identification and quarantining of people with illness. One of the least cost-effective means to identify those with the disease is obligatory temperature checking, which however seems to be one of the most popular methods used in the community.
Health authorities in many countries have taken effective public health measures to curtail COVID 19, which had a tangible impact on curtailing the spread of COVID-19. Focusing and implementing basic public health principles, some countries were successful in controlling the spread of COVID-19. Whereas, the countries that took a longer time to implement such had a wider spread of the disease and had significantly negative consequent on the populous, healthcare, and the economy. In the USA and Europe, vitamin D deficiency is highly prevalent during the winter months, mostly affecting the elderly people and migrants with darker skin color [8]. This is reflected by the fact that the average mortality rate from COVID-19 in European countries has a significant inverse correlation (p = 0.046) with serum 25(OH)D concentration [9].
Dissemination of the disease via air travelers
The spread of COVID-19 to countries outside China has occurred primarily through the air travel of Chinese tourists and workers and visitors returning home from Wuhan and other infected regions in China. How Beijing and Shanghai spared of COVID-19 is a mystery. In countries such as the United States, individuals arriving from areas where the coronavirus is present are strictly quarantined for a period of two weeks (in some countries, an additional two weeks home quarantine) to ensure that they are not infectious. When quarantine is performed humanely and not by force as in military camps, it is a useful public health measure in controlling spread of a communicable diseases.
The number of people infected with COVID-19 exponentially increased over the past few months, much faster than with the SARS virus (SARS-CoV) and MERS. When new information becomes available, key global public health organizations, such as the CDC, WHO, and similar organizations in China, should issue updated guidance and additional steps required to prevent disease spread.
The development of an effective and a safe vaccine for a viral disease could take a year or more. By the time an effective vaccine is developed, the likelihood is that the COVID-19 out-break will be over or the virus has mutated, so that vaccine is no more effective. In 2003, it took 20 months to develop a vaccine for the SARS outbreak; in contrast, in 2015 the Zika virus epidemic, a vaccine for was generated in 6 months. Because of the availability of RNA genomic sequences and encoded proteins of the COVID-19 virus, the author estimated six-months ago, that researchers will be able to generate an effective vaccine for the current coronavirus but not necessarily a safe or an affordable one.
The Cost-effective therapies to combat COVID-19
To-date, there is no effective, safe, and affordable treatments; antiviral agent or a vaccine against COVID-19 is not available. Although the final clinical outcome was controversial, the only cost-effective agent that has preventative effect on COVID-19 was hydroxychloroquine [10-12]. Chloroquine is awidely used against malaria and autoimmune diseases and is also known to block fusion of viruses and interfering with glycosylation, as in the case of SARS-CoV cellular receptors [13]. Antiviral drugs, such asr ibavirin, interferon, lopinavir-ritonavir, as well as corticosteroids have been studied in patients with SARS and MERS, although the efficacy of some drugs remains a matter of controversy [14].
A recent in vitro study reported that the combination of chloroquine and remdesivir is effective in the control of COVID-19 infection [15,16]. Preliminary data using animal models suggest that broad-spectrum antivirals, such as an RNA polymerase inhibitor, remdesivir and lopinavir/ritonavir and interferon-?might be effective against COVID-19, and previously was reported to be effective against MERS-CoV. Thus, researchers are experimenting with the use of nucleic acid vaccine platform approaches that have been used for generating vaccines against SARS-CoV and MERS-CoV.
What can be done right now to reduce disease risk and severity?
With corona viruses’ infections, early diagnosis is necessary, followed by isolation of persons, appropriate surveillance (track and trace), pro- vision of supportive treatment, and dynamic guidance to improve population immunity [17] and to avoid unnecessary panic. For individuals, good personal hygiene, wearing properly fitting masks, provision of appropriate ventilation, and avoiding spending time in crowded places will reduce risks of the spread of COVID-19 infection.
The effectiveness of appropriate face masks can be heightened by surfaces impregnation with ionic zinc oxide Zno;Zn2+-O2-) nanoparticles [18] with wurtzite stucture or PEGylated ZnO-nano-particles [19] or oxozinc; these components have been shown to have both antibacterial and antiviral activity [20,21]. Proper incorporation of ZnO- nanoparticles into materials can make them stable and able to kill pathogens on contact [22] and can be effectively use in personal protective equipment for added protection.
Biological effects that cause exacerbation of COVID-19 syndrome
COVID-19 and other coronaviruses enter human epithelial cells, such as pulmonary cells via membrane bound angiotensin 2 receptors (ACE-2); the enzyme that degrade angiotensin-II into a vasodilatory peptide, angiotensin [1-7,23]. However, many chronic diseases, such as diabetes, hypertension, obesity, and cardiovascular disease, reduce the cell surface- and soluble-ACE-2 concentration in blood, resulting over activation of the renin-angiotensinhormonal system (RAS) [24]. The resulting excess unopposed angiotensin-II causes pulmonary hypertension and edema, acute respiratory distress syndrome, and excessive stimulation of the expression of inflammatory cytokines [25,26]. Moreover, once COVID-19 enters into human cells, it markedly exacerbates the above vicious cycle that can lead to death [24,27].
Adequate vitamin D levels have been associated with reduced incidence and severity of enveloped viruses such as herpes zoster, Epstein-Barr, hepatitis, Ebola, HIV, dengue, measles, and mumps [28,29]. Studies have reported the administration of an oral dose of 50,000IU vitamin D reduces the risks of having in fluenza [4]. Vitamin D adequacy reduces the severity of pulmonary damage, pneumonia, cytokine storm, and acute respiratory distress syndrome (ARDS), which associated with coronaviral infections.Vitamin D is anatural vitamin, so the risk of adverse effects is minuscule.
Those who are with micronutrient deficiency, especially those with hypo vitaminosis D, are at a greater risk of developing viraldi [1] seases, including COVID-19 [30]. Thus, the most effective option is to have safe sun exposure and/or taking adequate doses of vitamin D supplements to raise and maintain serum 25(OH)D concentrations above 30ng/mL (see next section) to boost immunity before exposure [1,17,31]. This approach should reduce the risk not only of coronavirus but also of the common cold, influenza, and associated pneumonia, thus reducing deaths [4,31].
High-dose vitamin D and antioxidants reduce the risks and severity of coronavirus infection
Vitamin D is known to improve the immune system: whereas vitamin D deficiency increases vulnerability to viral infections, such as cold. and influenza [28,29]. During the winter months, unless supplements are taken, serum 25(OH)D concentrations are low in most people living in countries located in northern and southern latitudes. Considering its biological and physiological effects, there seems to be a multiple mechanism by which vitamin D causing immune regulatory effects [28].
Emerging data suggests that the maintenance of serum 25(OH)D concentrations in excess of 30ng/mL (75nmol/L) [1,32], preferably at a level greater than 40ng/L (100nmol/L). [1,33], together with sufficiency of other micronutrients, such as zinc, selenium, and antioxidants would provide a greater opportunity to prevent COVID-19.
Considering the inability to diagnose this corona virus early, during the early stages its several-day incubation period, people feeling unhealthy, who is having fever. In addition, those who might have been exposed to an infected person or contracted COVID-19 are likely to be benefited from loading dose of vitamin D. Such single oral doses include doses between 200,000 (four capsules of 50,000 or 60,000 IU) and 600,000 international units (IU). The efficacy of vitamin D could be increase by additional micronutrient supplements, including zinc, vitamin K2, magnesium, omega 3 fatty acids, quercetin, and resveratrol, to boost the immune system and to stimulate vitamin D receptors to synergize responses.
These can be repeated after few weeks. These approaches would allow strengthening of the innate. immune within three days of administration. This highly effective therapy cost no more than $8 per person and is expected to reduce the risk so contracting COVID-19, and its severity and reduce deaths. Even if the disease is experienced, unlikely to develop severe syndrome and death, and lead to speedy recovery. To significantly minimize viral infections, including COVID-19, one needs to maintain serum 25(OH)D concertation between 30 and 60 ng/mL, which is safe [31,34-36]. In general, to cause adverse effects from orally administered vitamin D, one needs to take daily doses higher than 20,000 IU for many months or take 1 million IU daily for a few days, reaching serum 25(OH)D concertation in excess of 125 ng/mL with signs and symptoms of hypercalcemia. Thus, the mentioned dose will not cause adverse effects; potential benefits far outweigh any theoretical risk.
A single high dose or a higher dose taken a week a par, as described above can be helpful in disease prevention and reducing its complications. From a disease prevention strategy point of view, the most cost-effective approach would be the prophylactic administration of high-dose vitamin D to the entire community at risk as a preventative measure. While this option was available during the first half of 2020, COVID-19 pandemic, no country had the wisdom to take that opportunity not even guiding its population on daily, safe sun exposure or vitamin D supplementation.
Conclusion
While people infected with COVID-19 reached unprecedented numbers the current death rate related to COVID-19 is significantly less than that associated with SARS or MERS. During the past six months, in many western countries, a large number of deaths occurred due to causes other than COVID-19 that had been documented as this viral illness, overestimating the reported statistics. Reasons for reporting such is complicated but include convenience, and to obtain extra financial incentives from federal governments by hospitals [37]. On the other hand, administrations of most tropical countries underestimated the incidence and deaths due to COVID-19 because they are conducting too little PCR testing (in fact, less than 5% per million population basis) and no community-based testing. Consequently, only a fraction of positive cases is diagnosed in the community. In either case, the statistics reported to the World Health Organization were erroneous and misleading.
Moreover, the incidence and mortality of COVID-19 strongly correlated with vitamin D status, that is intricately linked to effective exposure to UVB radiation. Therefore, it is logical to accept that the incidence, complications, and the mortality of COVID-19 are correlated with sun exposure and the serum 25(OH)D concentration. In those with hypovitaminosis have higher risks of developing the disease [38], the disease severity and deaths with COVID-19 [39]. There are a number of large randomized controlled clinical studies are currently underway that will be providing answers with reference to the efficacy of the vitamin D in controlling COVID-19 syndrome.
In most people, daily doses of between 2,000 and 5,000 IU are adequate for maintenance of serum 25(OH)D concentration above 30 ng/mL which is sufficient for improving most metabolic disorders. However, higher doses are likely needed in certain groups of people such as those with multiple comorbid conditions, such as, obesity, cancer, and to reduce all- cause mortality. In these person, the goal is to maintain serum 25(OH)D concentrations between 40 and 60 ng/mL, necessitating to take about 4,000 IU/day, significantly reducing the complications associated with hypovitaminosis D. Mentioned doses of vitamin D are safe and significantly minimize contracting viral.
Abbreviations
Acute respiratory distress syndrome (ARDS)
Angiotensin-converting enzyme 2 (ACE-2)
25-hydroxy vitamin D [25(OH)D]
1,25 dihydroxy vitamin D [1,25(OH)2D]
COVID-19 (SARS-CoV-2)
Randomized controlled trials (RCTs)
Renin–angiotensin hormonal system (RAS) Ultraviolet B (UVB) rays Vitamin D receptor (VDR)
Conflict of interest:
He received no funding for this work or assistance in professional writing for this article.
References
1. Wimalawansa SJ. 2020. Global epidemic of coronavirus-COVID-19: What can we do to minimize risks? European J. Biomed & Pharma Sci. 7: 432-438.
2. Kai H, Kai M. 2020. Interactions of coronaviruses with ACE2, angiotensin II, and RAS inhibitors-lessons from available evidence and insights into COVID-19. Hypertens Res. 43: 648-654. Ref.: https://pubmed.ncbi.nlm.nih.gov/32341442/
3. Merzon E, Tworowski D, Gorohovski A, et al. 2020. Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study. FEBS J. Ref.: https://pubmed.ncbi.nlm.nih.gov/32700398/
4. Grant WB, Lahore H, McDonnell L, et al. 2020. Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths. Nutrients. 12: 1626. Ref.: https://pubmed.ncbi.nlm.nih.gov/32252338/
5. Dancer RC, Parekh D, Lax S, et al. 2015. Vitamin D deficiency contributes directly to the acute respiratory distress syndrome (ARDS). Thorax, 70: 617-24. Ref.: https://pubmed.ncbi.nlm.nih.gov/25903964/
6. Tomaschitz A, Pilz S, Ritz E, et al. 2010. Independent association between 1,25-dihydroxyvitamin D, 25-hydroxyvitamin D and the renin-angiotensin system: The Ludwigshafen Risk and Cardiovascular Health (LURIC) study. Clin Chim Acta. 411: 1354-1360. Ref.: https://pubmed.ncbi.nlm.nih.gov/20515678/
7. CDC. Interim guidance for persons who may have 2019 Novel Coronavirus (2019-nCoV) to prevent spread in homes and residential communities.
8. Lips P. 2010. Worldwide status of vitamin D nutrition. J Steroid Biochem Mol Biol. 121: 297-300. Ref.: https://pubmed.ncbi.nlm.nih.gov/20197091/
9. Laird E, Rhodes J, Kenny RA. 2020. Vitamin D and Inflammation: Potential Implications for Severity of Covid-19. Ir Med J. 113: 81. Ref.: https://pubmed.ncbi.nlm.nih.gov/32603576/
10. Horby P, Mafham F, Jennifer LL, et al. 2020. Effect of Hydroxychloroquine in hospitalised patients with COVID-19: Preliminary results from a multi-centre, randomized, controlled trial. MedRziv (Preprint).
11. Chen Z, Hu J, Zhang Z, et al. 2020. Efficacy of hydroxychloroquine in patients with COVID-19: results of a randomised clinical trial.
12. Wallace DJ, Tse K, Hanrahan L, et al. 2019. Hydroxychloroquine usage in US patients, their experiences of tolerability and adherence, and implications for treatment: survey results from 3127 patients with SLE conducted by the Lupus Foundation of America. Lupus Sci Med. 6: 000317. Ref.: https://pubmed.ncbi.nlm.nih.gov/31168400/
13. Vincent MJ, Bergeron E, Benjannet S, et al. 2005. Chloroquine is a potent inhibitor of SARS coronavirus infection and spread. Virol J. 2: 69. Ref.: https://pubmed.ncbi.nlm.nih.gov/16115318/
14. Zumla A, F W Chan J, I Azhar E, et al. 2016. Coronaviruses - drug discovery and therapeutic options. Nat Rev Drug Discov. 15: 327-347. Ref.: https://pubmed.ncbi.nlm.nih.gov/26868298/
15. Farkas J. 2020. Remdesivir 5-day vs 10-day trial raises some red flags.
16. Tang W, Cao Z, Han M, et al. 2020. Hydroxychloroquine in patients mainly with mild to moderate Covid-19: An open label, randomized, controlled trial. Ref.: https://pubmed.ncbi.nlm.nih.gov/32409561/
17. Wimalawansa SJ. 2020. Fighting against COVID-19: Boosting the immunity with micronutrients, stress reduction, physical activity, and vitamin D. Nutrition and Food Science Journal (Sci Literature). 3: 1-4.
18. Krol A, Pomastowski P, Rafi?ska K, et al. 2017. Zinc oxide nanoparticles: Synthesis, antiseptic activity and toxicity mechanism. Adv Colloid Interface Sci. 249: 37-52. Ref.: https://pubmed.ncbi.nlm.nih.gov/28923702/
19. Ghaffari H, Tavakoli A, Moradi A, et al. 2019. Inhibition of H1N1 influenza virus infection by zinc oxide nanoparticles: another emerging application of nanomedicine. Journal of biomedical science. 26: 70-70.
20. Yung MMN, Antoine Fougères P, Hang Leung YU, et al. 2017. Physicochemical characteristics and toxicity of surface-modified zinc oxide nanoparticles to freshwater and marine microalgae. Sci Rep. 7: 15909. Ref.: https://pubmed.ncbi.nlm.nih.gov/29162907/
21. Kaushik N, et al. 2018. Zinc: A Potential Antiviral Against Hepatitis E Virus Infection? DNA Cell Biol. 37: 593-599. Ref.: https://pubmed.ncbi.nlm.nih.gov/29897788/
22. Sirelkhatim A, Mahmud S, Seeni A, et al. 2015. Review on Zinc Oxide Nanoparticles: Antibacterial Activity and Toxicity Mechanism. Nanomicro Lett. 7: 219-242. Ref.: https://pubmed.ncbi.nlm.nih.gov/30464967/
23. Xu J, Yang J, Chen J et al. 2017. Vitamin D alleviates lipopolysaccharide induced acute lung injury via regulation of the renin angiotensin system. Mol Med Rep. 16: 7432-7438.
24. Rhodes JM, Subramanian S, Laird E, et al. 2020. Perspective: Vitamin D deficiency and COVID-19 severity - plausibly linked by latitude, ethnicity, impacts on cytokines, ACE2, and thrombosis (R1). Ref.: https://pubmed.ncbi.nlm.nih.gov/32613681/
25. Meftahi GH, Jangravi Z, Sahraei H, et al. 2020. The possible pathophysiology mechanism of cytokine storm in elderly adults with COVID-19 infection: the contribution of "inflame-aging". Inflamm Res. 69: 825-839. Ref.: https://pubmed.ncbi.nlm.nih.gov/32529477/
26. Wang J, Jiang M, Chen Xin, et al. 2020. Cytokine storm and leukocyte changes in mild versus severe SARS-CoV-2 infection: Review of 3939 COVID-19 patients in China and emerging pathogenesis and therapy concepts. J Leukoc Biol. 108: 17-41. Ref.: https://pubmed.ncbi.nlm.nih.gov/32534467/
27. Du F, Liu B, Zhang S. 2020. COVID-19: the role of excessive cytokine release and potential ACE2 down-regulation in promoting hypercoagulable state associated with severe illness. J Thromb Thrombolysis.
28. Beard JA, Bearden A, Striker R. 2011. Vitamin D and the anti-viral state. Journal of clinical virology: the official publication of the Pan American Society for Clinical Virology. 50: 194-200. Ref.: https://pubmed.ncbi.nlm.nih.gov/21242105/
29. Gunville CF, Mourani PM, Ginde AA. 2013. The role of vitamin D in prevention and treatment of infection. Inflammation & allergy drug targets. 12: 239-245. Ref.: https://pubmed.ncbi.nlm.nih.gov/23782205/
30. Zemb P, Bergman P, Camargo Jr Ca, et al. 2020. Vitamin D deficiency and the COVID-19 pandemic. J Glob Antimicrob Resist. 22: 133-134. Ref.: https://pubmed.ncbi.nlm.nih.gov/32474141/
31. Wimalawansa SJ. 2020. Achieving population vitamin D sufficiency will markedly reduce healthcare costs. EJBPS. 7: 136-141.
32. Maghbooli Z, Ali Sahraian M, Ebrahimi M, et al. Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection. PLoS One. 15: 0239799. Ref.: https://pubmed.ncbi.nlm.nih.gov/32976513/
33. Wimalawansa SJ. 2020. What modelling and reproduction numbers are useful in predicting COVID-19 spread? Can J Biomed Res & Tech. 3: 1-4.
34. McDonnell SL, Baggerly C, B French C, et al. 2016. Serum 25-Hydroxyvitamin D Concentrations >/=40 ng/ml Are Associated with >65% Lower Cancer Risk: Pooled Analysis of Randomized Trial and Prospective Cohort Study. PLoS One. 11: 0152441. Ref.: https://pubmed.ncbi.nlm.nih.gov/27049526/
35. Kimball SM, Mirhosseini N, Holick MF. 2017. Evaluation of vitamin D3 intakes up to 15,000 international units/day and serum 25-hydroxyvitamin D concentrations up to 300 nmol/L on calcium metabolism in a community setting. Dermato-endocrinology. 9: 1300213-1300213. Ref.: https://pubmed.ncbi.nlm.nih.gov/28458767/
36. Wagner CL, Baggerly C, McDonnell S, et al. 2016. Post-hoc analysis of vitamin D status and reduced risk of preterm birth in two vitamin D pregnancy cohorts compared with South Carolina March of Dimes 2009-2011 rates. J Steroid Biochem Mol Biol. 155: 245-251. Ref.: https://pubmed.ncbi.nlm.nih.gov/26554936/
37. Annonymus. 2020. CARES Act Provider Relief Fund. Ref.: https://pubmed.ncbi.nlm.nih.gov/32867584/
38. D'Avolio A, Avataneo V, Manca A, et al. 2020. 25-Hydroxyvitamin D concentrations are Lower in patients with positive PCR for SARS-CoV-2. Nutrients. 12. Ref.: https://pubmed.ncbi.nlm.nih.gov/32397511/
39. Panagiotou G, Ann Tee Su, Ihsan Y, et al. 2020. Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalized with COVID-19 are associated with greater disease severity. Clin Endocrinol (Oxf). Ref.: https://pubmed.ncbi.nlm.nih.gov/32621392/




















