Indexing & Abstracting
Full Text
Letter to the EditorDOI Number : 10.36811/ojprm.2019.110001Article Views : 2575Article Downloads : 16
Community-acquired Pneumonia with Concurrent Multi-infections of Influenza A, Staphylococcus aureus, Streptococcus pneumoniae, Legionella and Invasive Pulmonary Aspergillosis in a Diabetic Patient
Chun-Chieh Yang, Chin-Ming Chen and Wen-Liang Yu*
Department of Intensive Care Medicine, Chi Mei Medical Center, Tainan City, Taiwan
*Corresponding author: Dr. Wen-Liang Yu, Department of Intensive Care Medicine, Chi Mei Medical Center, No. 901 Zhonghua Road, Yongkang District, 710 Tainan City, Taiwan. Fax: +886 6 283 3351; Email: Yuleon_md@yahoo.com.tw
Article Information
Aritcle Type: Letter to the Editor
Citation: Chun-Chieh Yang, Chin-Ming Chen, Wen-Liang Yu. 2019. Community-acquired Pneumonia with Concurrent Multi-infections of Influenza A, Staphylococcus aureus, Streptococcus pneumoniae, Legionella and Invasive Pulmonary Aspergillosis in a Diabetic Patient. Open J Pulm Respir Med. 1: 1-03.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2019; Chun-Chieh Yang
Publication history:
Received date: 18 March, 2019Accepted date: 27 March, 2019
Published date: 27 March, 2019
Keywords: Aspergillosis; Coinfection; Influenza; Legionellosis
Dear Editor
Invasive pulmonary Aspergillus infection during or after severe influenza infection in an immunocompromised patient or a previously healthy person has been reported in the literature [1-2]. In addition, coinfections of Staphylococcus aureus or Streptococcus pneumoniae with influenza are common, whereas simultaneous infections of legionellosis with aspergillosis are unusual in patients with influenza [2]. We herein report a diabetic patient who presented with a community-acquired pneumonia (CAP). The initial sputum culture yielded Aspergillus species and S. aureus, which were coinfected with influenza A, Pneumococcus and Legionella, with a deteriorated fatal course.
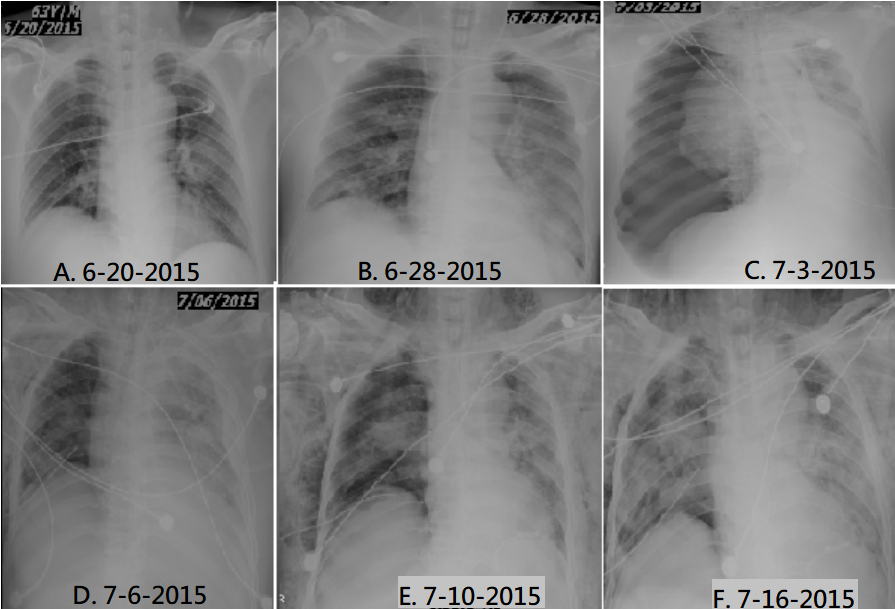
A 63-year-old man with diabetes mellitus felt general malaise and cough with sputum for 3 days. He was admitted to the intensive care unit (ICU) of the hospital on June 20, 2015 due to pneumonia with respiratory failure. There was no fever, diarrhea, headache, or skin rash. He denied travel and contact history. On examination, a blood pressure of 80/60 mmHg was noticed. The breath sounds revealed bilateral fine rales. Laboratory data included WBC 15,700/μL; band, 18%; CRP, 91.9 mg/L; BUN, 50 mg/dL; creatinine, 2.38 mg/dL; blood sugar, 221 mg/dL and HbA1C, 9.1%. The initial chest x-ray (CXR) film showed mild infiltration in perihilar area of left lung on June 20 (Figures 1A). The result of urinary Legionella Ag test was negative. Empirical antibiotic therapy included piperacillin-tazobactam and levofloxacin.
The initial sputum cultures yielded Aspergillus species and Staphylococcus aureus which was resistant to oxacillin. The blood Aspergillus Ag index using galactomannan assay was 4.89 (normal, <0.5), which was detected one week after hospitalization. The CXR film showed pneumonia in progression on June 28 (Figure 1B). Then, PCR for FluA of nasopharyngeal swab was positive. Pneumococcus Ag and follow-up Legionella Ag tests of urine samples became positive. Then antimicrobials were shift to oseltamivir, imipenem, levofloxacin, tigecycline and voriconazole.
As refractory hypotension and acute on chronic renal disease, continuous venovenous hemofiltration was performed. After therapy, the condition became improving with gradual recovery of urine output. However, massive tension pneumothorax occurred on July 3, the 14th day of hospitalization (Figure 1C). A chest tube was inserted and right lung expanded well (Figure 1D). Thereafter, sputum culture yielded carbapenem-resistant Acinetobacter baumannii (CRAB). The CXR films showed subcutaneous emphysema of bilateral neck and chest wall on July 10 (Figure 1E), with progressive worsening of infiltrates to diffuse lung fields on July 16 (Figure 1F). As unstable hemodynamics and poor left ventricular performance, family requested palliative care. The patient died on July 19, the 30th day of hospitalization.
Figure: 1: The chest films showing pneumonia in progression to pneumothorax (A-C), chest tube insertion (D), subsequent subcutaneous emphysema (E) and worsening pneumonia (F).
Coinfections caused by L. pneumophila and A. fumigatus were rarely reported, that might cause progression of Aspergillus disease [3]. Simultaneous L. pneumophila pneumonia and invasive aspergillosis could occur in an asthma patient receiving corticosteroid therapy [4]. On the contrary, intravenous administration of the corticosteroid to reduce severe inflammation of legionellosis might be associated with subsequent development of invasive aspergillosis [5]. The causes of deterioration in our case were multifactorial, especially a major event of tension pneumothorax.
Tracheobronchial aspergillosis with fibrinous sputum plugs mixed with Aspergillus fungal hyphae might cause check valve formation under positive-pressure ventilation, thus leading to life-threatening tension pneumothorax [6].
In conclusion, the human immunity will be diminished during post-influenza status. Thereby invasive Aspergillus infection may severely complicate the pneumonia, such as pneumothorax. On the contrary, influenza should also be diagnosed after sputum isolation of Aspergillus in a patient with CAP. Our case highlights the need to continue consider the potential multiple co-infections of influenza, aspergillosis, legionellosis, S. aureus and pneumococcal pneumonia.
Ethical approval
The study and waiver from the inform consent process were approved by the Institutional Review Board (IRB) of the Chi Mei Medical Center, Tainan city, Taiwan (IRB Serial number 10801-002).
References
- Schauwvlieghe AFAD, Rijnders BJA, Philips N, et al. 2018. Invasive aspergillosis in patients admitted to the intensive care unit with severe influenza: a retrospective cohort study. Lancet Respir Med. 6: 782-792. [Ref.]
- Ku YH, Chan KS, Yang CC, et al. 2017. Higher mortality of severe influenza patients with probable aspergillosis than those with and without other coinfections. J Formos Med Assoc. 116: 660-670. [Ref.]
- Guillouzouic A, Bemer P, Gay-Andrieu F, et al. 2008. Fatal coinfection with Legionella pneumophila serogroup 8 and Aspergillus fumigatus. Diagn Microbiol Infect Dis. 60: 193-195. [Ref.]
- Jiva TM, Kallay MC, Marin MG, et al. 1993. Simultaneous legionellosis and invasive aspergillosis in an immunocompetent patient newly treated with corticosteroids. Chest. 104: 1929-1931. [Ref.]
- Saijo T, Izumikawa K, Takazono T, et al. 2008. A case of Legionella pneumophila pneumonia followed by invasive aspergillosis. Jpn J Infect Dis. 61: 379-381. [Ref.]
- Matsuura H, Inoue S, Atagi K, et al. 2015. Life-threatening check valve formation due to tracheobronchial aspergillosis. JA Clin Rep. 1: 17. [Ref.]




















