Indexing & Abstracting
Full Text
Original ArticleDOI Number : 10.36811/ojor.2022.110017Article Views : 1Article Downloads : 1
Primary non-Hodgkin's lymphoma of the thyroid, type MALT: a case report from the Adolphe SICE General Hospital, Pointe Noire (Congo - Brazzaville)
Diembi S1*, Ngouoni GC2, Ondzotto G2, Itiere Odzili F2, Ngatali SF3, Willfred Akpo4, Moukassa D4, Otouana HB5, Brel D6 and Lallemant B7
1ENT Department, Adolphe SICE General Hospital, Pointe-Noire, Congo
2ENT Department, Centre Hospitalier et Universitaire, Brazzaville, Congo
3Oncology Department, Loandjili General Hospital, Pointe - Noire, Congo
4Department of Masters, Health and Human Biology, FSSA & HGELBO, Oyo, Congo
5ENT Department, Talangaï Reference Hospital, Brazzaville, Congo
6Centre de pathologie biterrois, Béziers, France
7ENT Department, CHU, Nîmes, France
*Corresponding Author: Dr. Sylvain Diembi, ENT Department, Adolphe SICE General Hospital, Pointe-Noire, Congo, Tel 0024205 538 41 52; Email: sdiembi@yahoo.fr
Article Information
Aritcle Type: Original Article
Citation: Diembi S, Ngouoni GC, Ondzotto G, et al. 2022. Primary non-Hodgkin's lymphoma of the thyroid, type MALT: a case report from the Adolphe SICE General Hospital, Pointe Noire (Congo - Brazzaville). Open J Otolaryngol Rhinol. 4: 01-08.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2022; Diembi S
Publication history:
Received date: 18 December, 2021Accepted date: 05 January, 2022
Published date: 07 January, 2022
Abstract
Primary lymphomas of the thyroid are rare tumours, representing less than 5% to 15% of thyroid cancers. These lymphomas develop on a pre-existing thyroid disease, notably Hashimoto's thyroiditis, or as a secondary site of a disseminated lymphoma. This pathology is aggressive and presents as a painful, rapidly evolving goitre with signs of compression. The most common histological types are non-Hodgkin's lymphoma type B. We report a case of thyroid non-Hodgkin's lymphoma of the MALT type in a 71 year old woman with a specific history; the positive diagnosis was made thanks to a histological study of the surgical specimen completed by an immunohistochemical study on paraffin sections. The postoperative clinical course after six years was favourable, with no local recurrence or distant metastasis.
Keywords: Goiter; Primary Lymphoma; Thyroid; MALT; Immunohistochemistry
Introduction
Primary thyroid lymphomas (PTL) are rare entities. They account for less than 5% of all thyroid cancers [1]. PTL is a histologically and clinically heterogeneous disease; its differential diagnosis is with differentiated thyroid carcinomas for indolent forms, and anaplastic carcinomas for aggressive and high-grade forms that may manifest as a painful, rapidly progressive and compressive mass. The most common forms are high-grade diffuse large B-cell primary thyroid lymphoma (LPT) and primary lymphoma arising from mucosa-associated lymphoid tissue (MALT) [1-3]. We report a case of thyroid non-Hodgkin's malignant lymphoma of the MALT type, the diagnosis of which benefited from immunohistochemical study on paraffin sections paraffin.
Medical observation
Mrs. GO Cl, 71 years old, living in the city of Pointe-Noire, consulted in February 2014 for an anterocervical mass associated with intermittent cervical pain. She has a history of diabetes and hypertension for 10 years, and also endoscopic cholecystectomy in 1971 in Marseille (France). The history of the disease dates back to 6 months before the consultation with the appearance of a progressive increase in the volume of the neck, followed a few weeks later by the sensation of a mass, pain and a sensation of cervical compression without dyspnoea or dysphonia which motivated the ENT consultation. The ENT examination noted a good general condition with normal mucocutaneous colouration, a temperature of 37°C, a blood pressure of 140/90 mm Hg and a heart rate of 88 beats per minute. On inspection, the neck is enlarged, palpation reveals a solid antero-cervical mass measuring 54 mm by 35 mm, mobile on swallowing, the skin covering is not very tense and normal in appearance. There is no turgidity of the jugular veins and auscultation of the cervical region registers a murmur synchronous with the pulse. The abdomen is soft with no visible mass or scarring. The lungs are free; she has no oedema of the lower limbs; pedal pulses are present and symmetrical. Cervical ultrasound revealed an enlarged thyroid gland at the expense of the two thyroid lobes and the isthmus (right lobe 65x45 mm, left lobe 70x55 mm, isthmus 35x30 mm) dotted with several nodules, the largest of which was 25x20 mm, with the presence of cervical lymphadenopathy.
The chest X-ray shows a slight tracheal deviation, on healthy lung parenchyma, the hormonal balance sheet, i.e. the thyroid hormone assay is normal (FT3=4µmol/l, FT4= 10 µmol/l and TSH=1.25 µg/l), the assay of the blood sugar level, as well as the anti-thyroglobulin antibody and the anti-peroxidase antibody are normal. The blood count is also normal. Initially, the clinical and paraclinical work-up was in favour of a multi-hetero-nodular goitre in euthyroidism in a 71 year old diabetic and hypertensive woman. The treatment consisted of a total thyroidectomy with recurrent lymph node dissection due to the presence of cervical lymphadenopathy. The postoperative course was simple, and the surgical specimen was subjected to anatomopathological analysis. Macroscopically, both thyroid lobes were swollen and multinodular with significant collateral circulation (Figure 1). On microscopic examination of systematic samples, the thyroid parenchyma was occupied by a lymphoid proliferation showing a diffusé and nodular architecture with some residual thyroid vesicular structures (Figure 2). At high magnification, the infiltrate consisted of a monomorphic population of small lymphocytes with rounded or angular nuclei with finely reticulated chromatin and no nucleoli (Figure 3). These tumour cells had a sparse, acidophilic cytoplasm showing slight plasma cell differentiation. The tumour infiltrate extended into the peri-thyroid fat. The immunohistological study by Bond Polymer Define Detection technique (Bond Max Automate) on deparaffinised sections after antigenic restoration by heat had been performed. The lymphoma cells strongly expressed the CD20 antigen (Figure 4), the BCL2 antigen and a slight overexpression of the Kappa light chain. In contrast, the anti-CD3 antibody marked a low residual T lymphoid population that was mainly internal. At the lymph node level, there is an inter-follicular T cell population. The residual thyroid vesicles had lympho-epithelial lesions labelled with anti-AE1/AE3 antibody (Figure 5). The clinical course after 1 month, 3 months, 6 months and 1 year was straightforward. The clinical check-up carried out after six years of follow-up did not note any local recurrence or progressive metastasis. The patient had not received postoperative chemotherapy.

Figure 1: Macroscopic features.

Figure 2: Diffuse profiliferation lymphoid.

Figure 3: Lymphoid proliferation at high magnification.
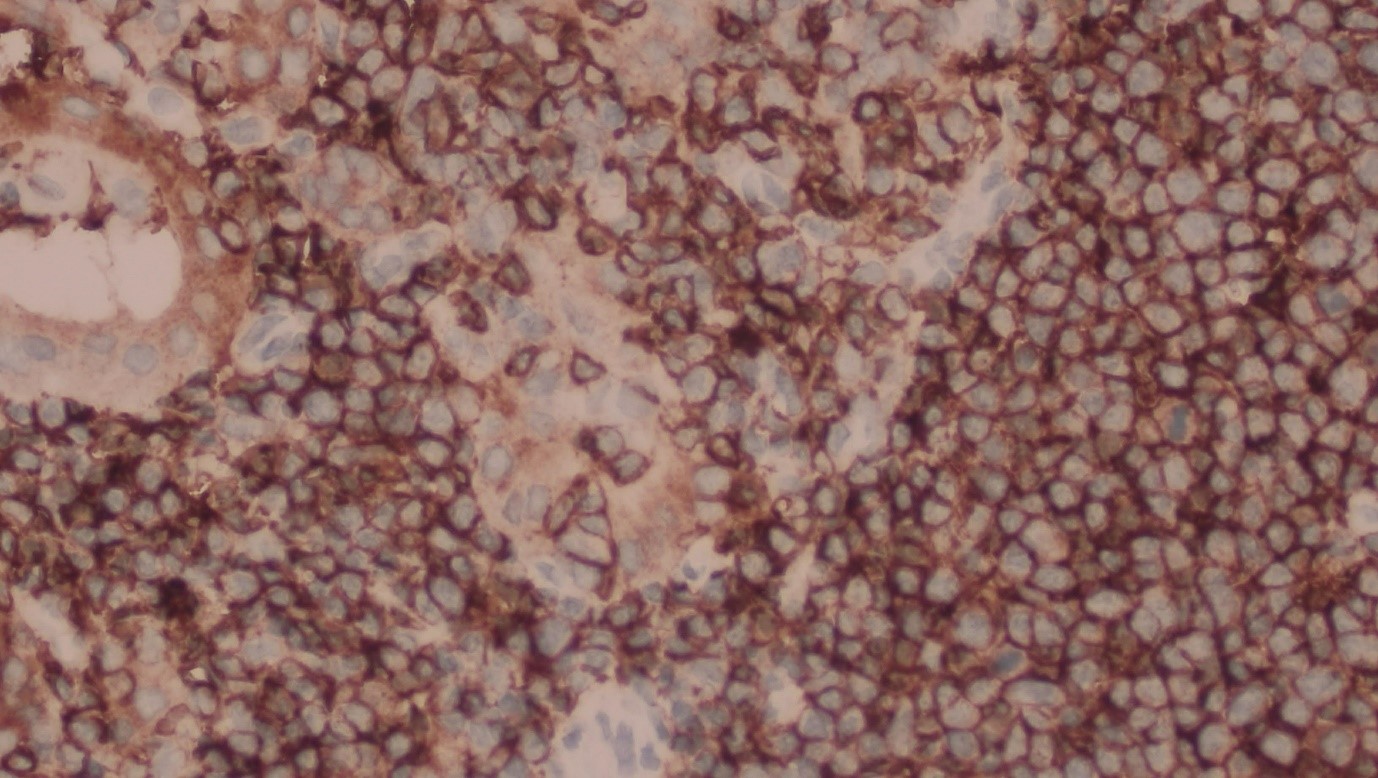
Figure 4: Immunohistochemistry, intense labelling with anti-CD20 antibody.
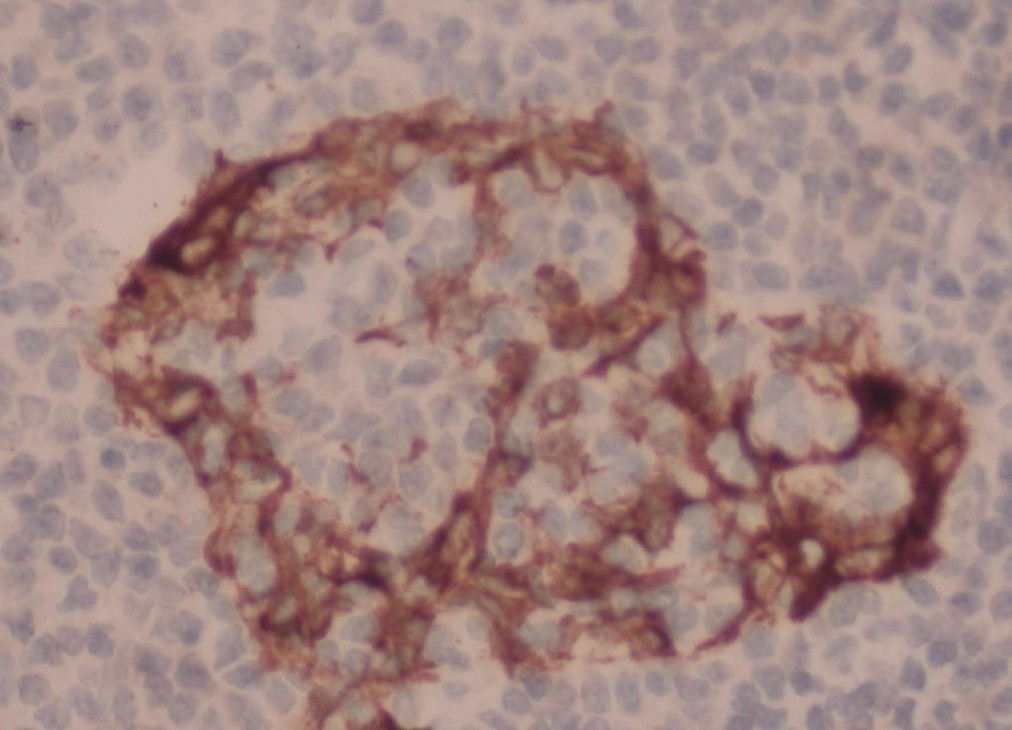
Figure 5: Immunohistochemistry, intense anti-AE1AE3 antibody labelling.
Discussion
Primary lymphomas of the thyroid gland are rare anatomical entities. They represent less than 5% of all thyroid cancers [1]. Their estimated incidence of 1.1-2.06/million population/year has increased in recent years [16]. Thyroid lymphoma classically occurs in women [1], aged between 60 and 70 years, with a female-to-male ratio of 1.5-1.4 depending on the study [1,9]. Primary thyroid lymphoma is a particular haematological entity that develops essentially on pre-existing thyroid lesions, notably Hashimoto's lymphocytic thyroiditis [1]. The association is found in 25 to 100% of cases depending on the series [1,12,13]. The relative risk of lymphoma in subjects with autoimmune thyroiditis is about 67 times higher than in healthy subjects [17]. Indeed, the thyroid gland does not normally contain lymphoid tissue, which accumulates during various pathologies, notably autoimmune diseases such as Hashimoto's thyroiditis. Indeed, the continuous antigenic stimulation during this pathology induces a proliferation of lymphocytes whose mutations may be the cause of lymphoma; however, not all Hashimoto's thyroiditis evolves into lymphoma [17].
The clinical picture is summarised by a rapidly evolving thyroid tumour causing a compressive syndrome in 20-25% of cases [16]; this was the case in our observation, which presented with a multiheteronodular goitre, adherent to the surrounding tissues with a painful character that would be in favour of the diagnosis. Satellite cervical adenopathies are found in 20% of cases [1], general signs such as fever, night sweats and weight loss may be present, biological hypothyroidism is encountered in 40% of cases but without clinical expression is rare [18]. Examination of the surgical specimen provided the diagnosis following histological examination coupled with immunohistochemistry performed on paraffin sections. Macroscopically, the tumour areas have a characteristic "fish-flesh" appearance, with a turgid vascular network, as can be seen on our surgical specimen (microphotograph n°2). On microscopic examination, the thyroid parenchyma was the site of a lymphomatous proliferation, not encapsulated, poorly limited, without necrosis or haemorrhagic areas. Histologically, the majority of lymphomas reported in the literature are non-Hodgkin's lymphomas of B phenotype and high grade of malignancy, large cells of diffuse type [18], a minority are of T phenotype, some thyroid lymphomas of low grade of malignancy fall within the framework of lymphomas developed on mucosa-associated lymphoid tissue (MALT) [17,18]. Histological diagnosis is not always easy and the difficulty may arise with chronic Hashimoto's thyroiditis, anaplastic carcinoma or, more rarely, RIEDEL's thyroiditis, in which case immunohistochemistry must be used to demonstrate a particular phenotype. The primary location constitutes 1-2.5% of all lymphomas [18]. The primary nature of thyroid lymphoma is retained after a complete extension work-up, in order to eliminate any associated disease. In addition to a complete clinical examination, the work-up will include a thoracic-abdominal-pelvic CT scan, a bone-medullary biopsy, a study of the cerebrospinal fluid, and an LDH and beta2microglobulin measurement. The rest of the work-up will be requested according to the signs of the disease [18].
The treatment of choice is determined primarily by the histological type of lymphoma and its extent [16]. The optimal treatment of thyroid lymphoma is a highly controversial topic in the literature. Currently, the indications for surgery have become increasingly limited, and it is reserved for strictly intracapsular thyroid tumours of low grade malignancy (of the MALT type and others), this surgery will be in the form of total thyroidectomy; as performed by our team (Figure 1). External cervical-mediastinal radiotherapy at a dose of 40 Gy ensures, according to some authors, the same result at this stage with a 5-year survival of 90% [18]. Surgery also plays an essential role in the initial management of patients with upper airway obstruction by performing a tracheotomy. For localized large cell lymphoma of type B and high grade of malignancy, representing the most frequent histological type, the reference treatment consists of CHOP chemotherapy, followed by locoregional irradiation at a dose of 35-45 Gy, our patient did not benefit from chemotherapy or radiotherapy because the histological type is a MALT lymphoma and therefore of low grade, it was just a question of clinical and paraclinical surveillance. Some authors report that the 5-year survival in this case approaches 100%. In case of disseminated lymphoma of high grade of malignancy, exclusive chemotherapy is indicated. In the case of compressive lymphoma, prednisolone allows a significant reduction in the volume of the goitre. The results of the literature are very variable with regard to prognostic factors. Clinical signs of locoregional extension have a negative impact on prognostic outcome; such as dyspnoea, dysphonia and/or dysphagia, extra-thyroid extension, stage, histological type, age and tumour size [1,8,18]. The importance of histological type in prognosis is controversial. Several authors have not found a correlation between histological type and prognosis; on the other hand, some believe that nodular lymphomas have a better prognosis than diffuse lymphomas [1,18].
Conclusion
Primary thyroid lymphomas are rare tumours. They should be considered in the presence of a rapidly enlarging cervical mass with signs of compression, including pain. Imaging and histopathological examination with immunohistochemical study of the tumour tissue contribute to a definite diagnosis. Thyroid lymphoma of the MALT type is a tumour with a good prognosis, and total thyroidectomy is the most recommended treatment in intracapsular forms. The prognosis is generally good in this histological type.
References
1. Taali L, Baghdadi, Abada A. 2016. Lymphome de la thyroïde, à propos d’un cas et revue de la littérature. Rév Méd Gd Lacs. 5: 104-111.
2. Benhammou A, Dib N, Mesbah H. 2008. Lymphome primitif de la thyroide (à propos de deux cas). La lettre du cancerologue. 6: 268-270.
3. Natsuko W, Hiroto N, Jaeduk YN. 2018. Long-term outcomes of 107 cases of primary thyroid mucosa-associated lymphoid tissue lymphoma at a single medical institution in japan. J Clin Endocrinol Metab. 103: 732-739. Ref.: https://pubmed.ncbi.nlm.nih.gov/29165612/ DOI: https://doi.org/10.1210/jc.2017-01478
4. Stein SA, Wartofsky L. 2013. Primary thyroid lymphoma : A clinical review. J Clin Endocrinol Metab. 96: 3131-3138. Ref.: https://pubmed.ncbi.nlm.nih.gov/23714679/ DOI: https://doi.org/10.1210/jc.2013-1428
5. Ruggiero FP, Frauenhaffer E, Stack BC. 2005. Thyroid lymphoma a single institution’s experience. OtoLaryngol Head Neck Surg. 133: 888-896. Ref.: https://pubmed.ncbi.nlm.nih.gov/16360509/ DOI: https://doi.org/10.1016/j.otohns.2005.07.040
6. Rummel MJ, Nederle N, Mashmeyer G. 2013. Studygroup indolent lymphomas bendamustine plus rituvimab versus CHOP plus rituximab as first live treatment for patients with indolent and mantle-cell lymphomas : An open-label, multicenter randomised phase3 non inferoirity trial. Lancet. 381: 1203-1210. Ref.: https://pubmed.ncbi.nlm.nih.gov/23433739/ DOI: https://doi.org/10.1016/s0140-6736(12)61763-2
7. Siun W, Aoife J, Denis E. 2013. Thyroid lymphoma : Recent advances in diagnosis and optimal management strategies. The oncologist. 18: 994-1003. Ref.: https://pubmed.ncbi.nlm.nih.gov/23881987/ DOI: https://doi.org/10.1634/theoncologist.2013-0036
8. Katua R, Shet T, Sengor M. 2013. Clinicopathologic study and outcom analysis of thyroid lymphomas. Experience from a tertiary cancer center. Head Neck. 35: 165-171. Ref.: https://pubmed.ncbi.nlm.nih.gov/22368156/ DOI: https://doi.org/10.1002/hed.22928
9. Yokoyama J, Ohla S. 2012. Problems of primary T-cell lymphoma of the thyroid gland a case report. World J Surg Oncol. 10-58. Ref.: https://pubmed.ncbi.nlm.nih.gov/22515161/ DOI: https://doi.org/10.1186/1477-7819-10-58
10. Paccalin M, Gouet D, Ribouleau V. 2001. Lymphome malin primitif de la thyroïde à propos de huit cas. Rev Med Interne. 22: 934-938. Ref.: https://pubmed.ncbi.nlm.nih.gov/11695316/ DOI: https://doi.org/10.1016/s0248-8663(01)00451-9
11. Onal C, Li XY, Miller RC. 2011. Treatment results andprognostic factors in primary thyroid lymphoma patients : A rare cancer network study. Ann Oncol. 22: 156-164. Ref.: https://pubmed.ncbi.nlm.nih.gov/20587509/ DOI: https://doi.org/10.1093/annonc/mdq310
12. Earnest LM, Cooper DS, Sciubba JJ. 2006. Thyroid MALT lymphoma in patients with a compressive goiter. Head Neck. 28: 765-770. Ref.: https://pubmed.ncbi.nlm.nih.gov/16628752/ DOI: https://doi.org/10.1002/hed.20424
13. Meyer GY, Sywak MS, Reeve TS. 2008. Surgical trends in the management of thyroid lymphoma. Eur J Surg Oncol. 34: 576-580. Ref.: https://pubmed.ncbi.nlm.nih.gov/17604588/ DOI: https://doi.org/10.1016/j.ejso.2007.04.016
14. Belal A, Allan A, Kandil A. 2001. Primary thyroid lymphoma a retrospective analysis of prognostic factor and treatment outcome for localized intermediate and high grade lymphoma, Am J clin Oncol. 24: 299-305. Ref.: https://pubmed.ncbi.nlm.nih.gov/11404505/ DOI: https://doi.org/10.1097/00000421-200106000-00019
15. Canan U, Yersu K, Grcan V. 2002. Primary thyroid lymphoma : A report of two cases. Turkish Journal of Endocrinology and Metabolism. 1: 41-45.
16. Michels C, Delcambre J, Mamey. 2002. Lymphomes thyroidiens primitifs, Etude clinicopathologique de 30 cas et revue de la littérature. Ann Pathol. 22: 10-17. Ref.: https://pubmed.ncbi.nlm.nih.gov/11937995/
17. Moshynska OV, Saxena A. 2008. Clonal relaionship between Hashimoto thyroiditis and thyroid lymphoma, J Clin Pathol. 61: 438-444. Ref.: https://pubmed.ncbi.nlm.nih.gov/18006670/ DOI: https://doi.org/10.1136/jcp.2007.051243
18. Thieblemont C, Mayen A, Dumontat C. 2002. Primary thyroid lymphoma is a heterogeneous disease. J Clin Endocrinol Metab. 87: 209-213. Ref.: https://pubmed.ncbi.nlm.nih.gov/11788631/ DOI: https://doi.org/10.1210/jcem.87.1.8156




















