Indexing & Abstracting
Full Text
Case ReportDOI Number : 10.36811/ojor.2021.110014Article Views : 85Article Downloads : 42
Cervical lymph node metastasis revealing a prostate adenocarcinoma: About two observations and Review of the Literature
Sylvain DIembi1, Boris Harold Otouana Dzon2, Gérard Chidrel Ngouoni3, Franck Arnaud Itiere OdzilI3, Synclair Ngotene Diembi1, Donatien Moukassa4, Gontran Ondzotto3
1ENT Department, Adolphe SICE General Hospital, Pointe-Noire
2ENT Department, Talangai Reference Hospital, Brazzaville
3ENT Department, Brazzaville University Hospital
4Department of Master, Health and Human Biology, FSSA (UMNG) - HGELBO, Brazzaville
*Corresponding Author: Dr. Sylvain Diembi, Department of Otolaryngology, Adolphe SICE General Hospital, Pointe-Noire (Congo), Pointe Noire, Tel: 00242055384152; Email: sdiembi@yahoo.fr
Article Information
Aritcle Type: Case Report
Citation: Sylvain DIembi, Boris Harold Otouana Dzon, Gérard Chidrel Ngouoni, et al. 2021. Cervical lymph node metastasis revealing a prostate adenocarcinoma: About two observations and Review of the Literature. Open J Otolaryngol Rhinol. 3: 27-34.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2021; Sylvain Diembi
Publication history:
Received date: 18 October, 2021Accepted date: 25 October, 2021
Published date: 26 October, 2021
Abstract
Prostatic adenocarcinoma is the most common cancer in men, and is the 3rd leading cause of death in men worldwide. This slow-growing, hormone-sensitive cancer occurs after the age of 50 years. Cervical lymph node metastases of prostate adenocarcinoma are rare. We report two anatomical observations over a ten-year period of activity. The two men were aged 80 and 72 years, respectively, and both presented with multiple cervical adenopathies of particular topography above the clavicle, associated with urinary signs such as dysuria, pollakiuria and incontinence. Microscopic examination coupled with immunohistochemistry (anti-PSA antibodies) of the excised biopsy of these lymph nodes contributed to the diagnosis of certainty.
Keywords: Adenocarcinoma; Prostate; Metastasis; Node; Neck; Immunohistochemistry
Introduction
Cervical lymph nodes are most often the preferred sites of metastasis of upper aerodigestive tract (UAD) cancers. These secondary metastatic cancers may develop at the expense of aerodigestive tissues and infiltrate the mucosal lining of the upper aerodigestive tract, the lymphoid tissues associated with the mucosa, the salivary glands, the thyroid and/or the skin lining [1,2]. Their primary origin may be local or distant ; in this case these metastases are considered as atypical sites. Indeed, cervical or cervicothoracic lymph node metastases of prostate origin are considered atypical sites and their diagnosis requires immunohistochemical investigation based on a panel of antibodies, of which the anti-PSA antibody is one of the most specific biomarkers in humans [1,3]. In rare cases, secondary cancers of the head and neck region, including lymph node chains, lung, kidney, bone and breast cancers seem to be the most reported in the literature [1,3-5]. In contrast, prostate adenocarcinoma, the most frequent cancer in men, being the 3rd most common cause of morbidity and mortality per year in men, exceptionally presents localisations in the "head and neck" sphere. We report two cases of cervical lymph node metastases revealing the evolution of a prostate adenocarcinoma.
Case Report
Observation n° 1:
Mr GOU. Ja, 80 years old, consulted in October 2014 for bilateral multiple cervical mass, bilateral axillary mass and bilateral inguinal mass evolving for 4 years. His history includes 10 years of arterial hypertension, well controlled on calcium channel blockers. The history of the disease goes back 4 years before the consultation with the installation of a mictional disorder of dysuria and pollakiuria completed later by an acute retention of urine, one year later appears masses at the inguinal level. These masses were bilateral, hard, firm and fixed, the largest measuring 4 cm in maximum diameter. One year later, these masses extend to the right and left axillary hollows, of approximately the same size as the inguinal masses. A few weeks later, bilateral cervical masses appear in the supra-clavicular region, hard, firm and mobile. The persistence of the cervical masses prompted an ENT consultation.
The ENT examination showed a preserved general state with a blood pressure of 140/90 mm Hg and a regular heart rate of 80/min. In addition, on rectal examination, the prostate was enlarged, with an invaded median groove, and the finger pad showed some traces of blood. The cervical examination showed cervical masses of different sizes, with a firm consistency, located in the supra-clavicular region (Figure 1). (Cervical ultrasound showed multiple cervical adenopathies of different sizes, and abdominal and pelvic ultrasound showed an enlarged prostate with irregular contours and deep adenopathies (Figure 2). Cervical and inguinal lymph node biopsy and excision was performed. The excised specimens consisted of six 20.8g fragments ranging in size from 20-25mm. The individual sections of these specimens were whitish, fairly firm, with foci of haemorrhage and necrosis (Figure 3). Microscopic examination of the lymph nodes showed massive destruction of the lymph node parenchyma by epithelial tumour proliferation, accompanied by a small, fibrous stroma. The proliferation formed polyadenoid masses with multiple glandular lumens sometimes containing foamy macrophages (Figure 4 and 5). This proliferation was lined by cubic or columnar cells with acetowhite cytoplasm. The tumour cells have enlarged, vesicular, highly nucleated nuclei. Mitoses are numerous with an average of five to six mitoses per field at high magnification (Figure 6). There are a few atypical mitoses. There are a few epitheliomatous masses centred by tumour necrosis, producing images of comedonecrosis. The immunohistochemical study using the Bond Polymer Define Detection technique (Automate Bond Max) on deparaffinised sections after antigenic restoration by heat revealed strong membrane and cytoplasmic expression of the anti-PSA antibody of the tumour proliferation (Figure 7). On the other hand, anti-CK7, anti-CK20 (digestive origin), anti-TTF1 (bronchopulmonary and thyroid origin) antibodies were negative. Anatomopathological examination concluded that it was a lymph node metastasis of a po orly differentiated prostate adenocarcinoma.
Observation n°. 2:
Mr Mal. No, 72 years old, male, consulted in February 2016 for a bilateral multiple cervical mass and a bilateral inguino-scrotal mass evolving for 2 years. His history included hypertension and diabetes dating back 15 years, both normo-balanced. The history of the disease goes back 2 years before the consultation with the installation of massent at the inguino-scrotal level. These masses were bilateral, hard, firm and fixed. One year later, mobile cervical masses appeared, bilateral, supra-clavicular, hard, and firm, associated with a discrete mictional disorder of pollakiuria. In view of the persistence of the cervical masses, an ENT consultation was requested. The ENT examination showed a preserved general state. The blood pressure was 140/90 mm Hg, with a regular heart rate of 80 beats/min. The cervical examination showed cervical masses of different sizes and firm consistency, located above the clavicle.
The rectal examination revealed an enlarged prostate, with a poorly appreciated median groove, and the finger pricker brought back some traces of blood. Cervical ultrasound confirmed the presence of multiple cervical adenopathies of different sizes, and abdomino-pelvic ultrasound showed the presence of deep intra-abdominal adenopathies. Cervical lymph node biopsy with histological study was performed. Macroscopically, nodular or cerebriform masses were noted; histologically, the microscopic appearance led to the conclusion of a lymph node metastasis of a prostatic adenocarcinoma.

Microphotograph n°1: Bilateral supra-clavicular lymph node package.
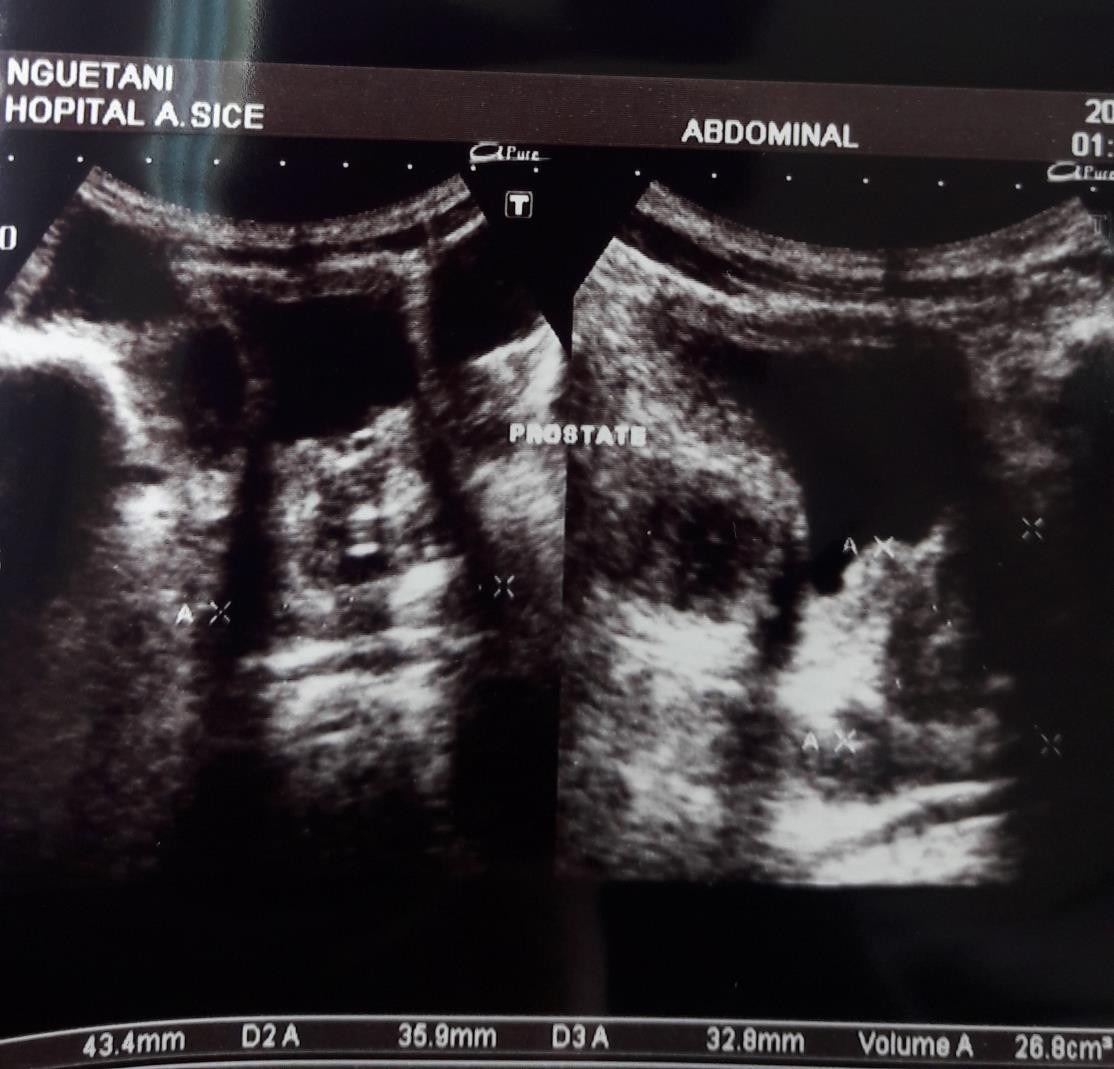
Microphotograph n°2: Abdominal-pelvic ultrasound homogeneous prostatic hypertrophy.

Microphotograph n°3: Biopsy of the cervical lymph node: large adenopathy of nodular and cerebriform appearance.
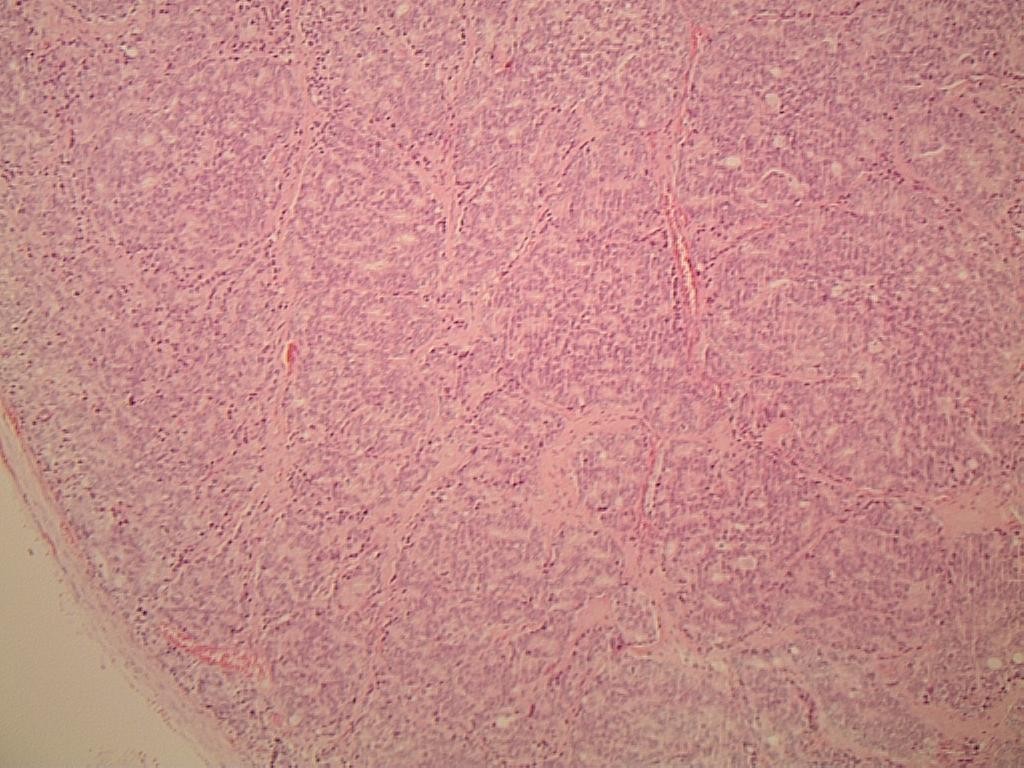
Microphotograph n°4: Haematoxylin and eosin (low magnification), sub capsular, diffuse and parenchymal infiltration of carcinoma cells of prostatic origin.
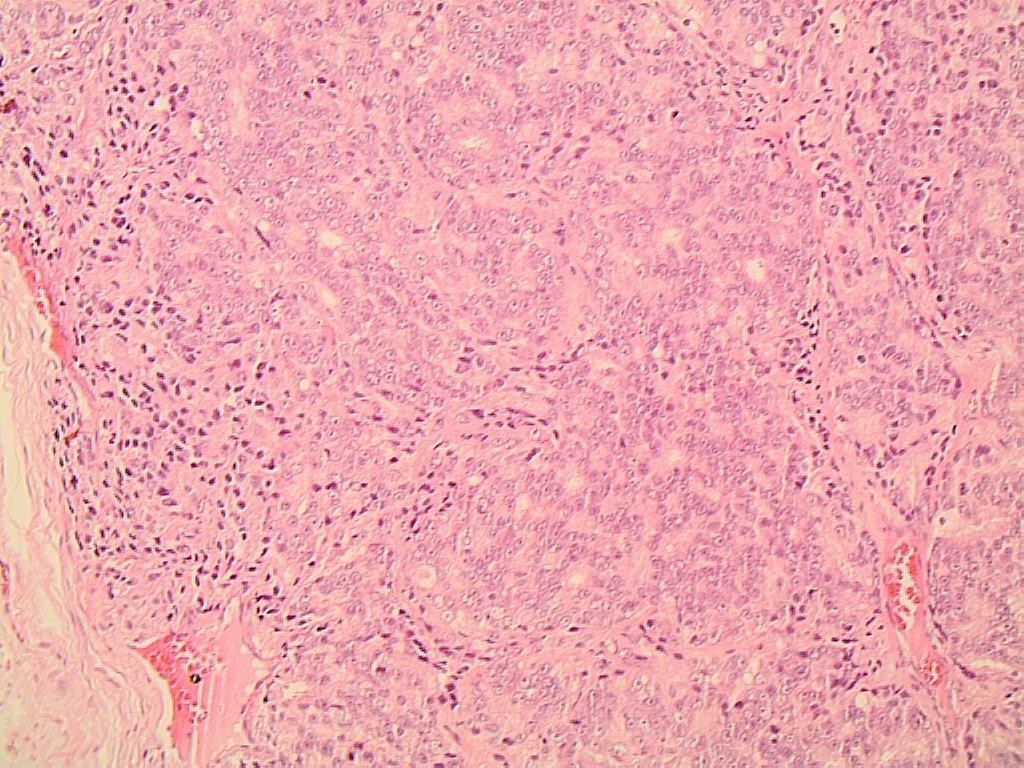
Microphotograph n°5: haematoxylin and eosin, medium magnification (GX40), subcapsular infiltration of carcinoma cells of prostatic origin.
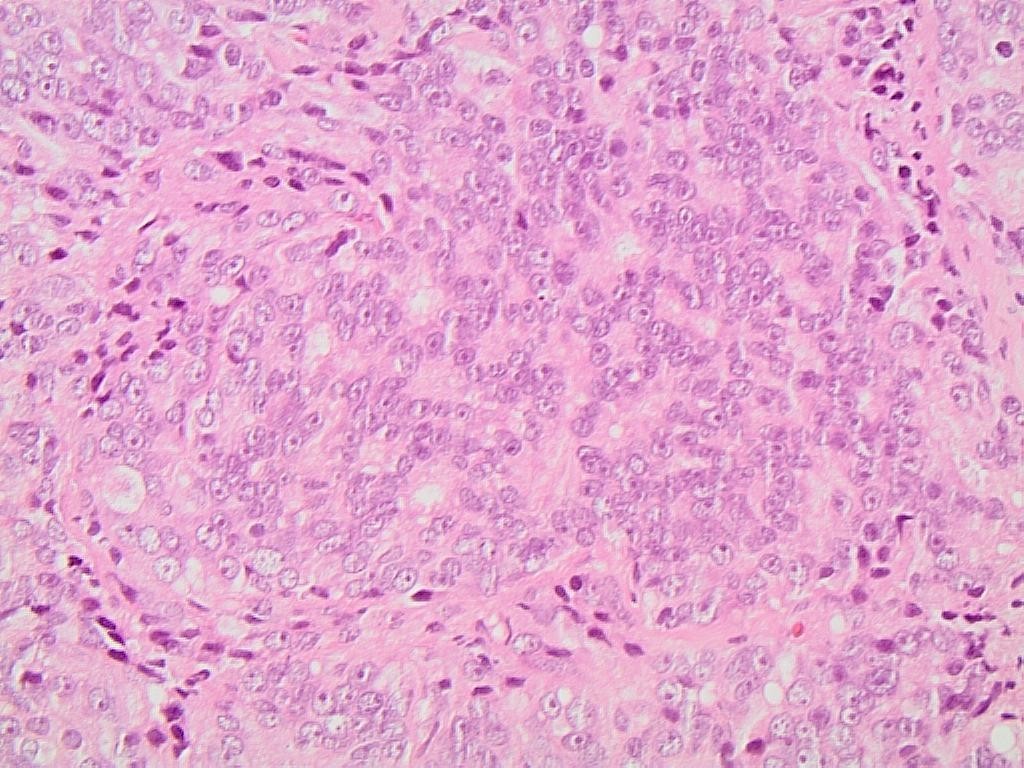
Microphotograph n°6: Haematoxylin and eosin, high magnification (GX60) Clusters of malignant tumour cells infiltrating the lymph node parenchyma.
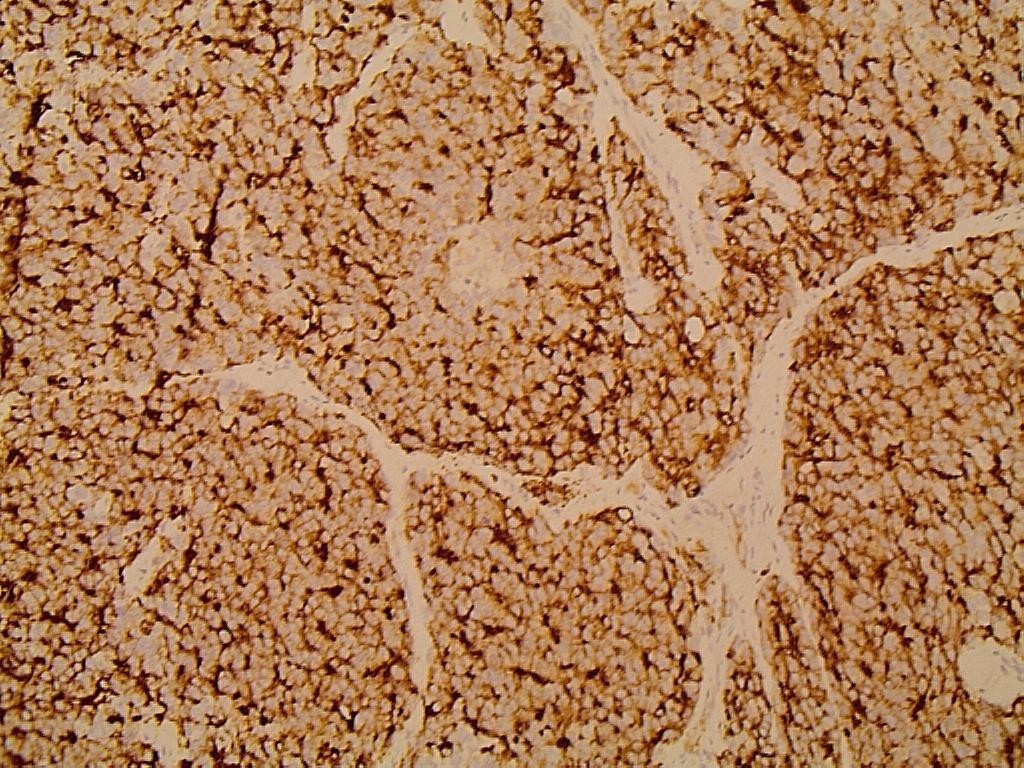
Microphotograph n°7: Immunohistochemistry on paraffin sections, GX20, anti-PSA antibody, membrane and cytoplasmic labelling.
Discussion
Prostatic adenocarcinoma is the most common cancer in men, and is the 3rd leading cause of death in men worldwide. In America, particularly in the USA, prostate adenocarcinoma is the leading cause of death in men with an incidence of 100,000 cases per year [1]. In our study, 2 cases out of approximately 100 patients with lymph node metastasis over 10 years of professional activity were collected, i.e. 2% of recorded cases. This rarity has been attested to by some authors. Indeed, Flocks et al report only 6 observations out of 1500 [9], while Hessan et al find respectively 0 cases out of 415 cases [4]. The two patients were respectively 72 and 81 years old; the average age of onset of these lesions is found by most authors [6]; however, in the USA, the study by B. Copeland et al found subjects aged 50 years [1]. The most frequent clinical symptoms of prostatic adenocarcinoma are dysuria, urinary retention, haematuria or incontinence. These symptoms were also found in our two patients at the time of diagnosis. The supraclavicular location of the cervical adenopathies is quite particular for our two observations, however some authors have found adenopathies on the upper jugulo - carotid chains. The histological diagnosis of cervical or supra-clavicular adenopathies allows us to determine the primary origin of these lymph nodes [6,7,10,11]. Diagnostic orientation is based on the tumour architecture where the infiltration is subcapsular and made up of trabeculae or lobules of carcinomatous cells (Figures 4 and 5). The appearance of the tumour cells can be well differentiated or undifferentiated requiring immunohistochemical study using anti-PSA or anti-cytokeratin antibodies (CK7, CK20). The tumour cells strongly express the PSA antigen with membrane and cytoplasmic labelling of the anti-PSA antibody (Figure 7). The differential diagnosis is made with adenocarcinoma metastasis of bronchopulmonary, thyroid and renal origin [12-14].
Conclusion
Cervical lymph node metastases from prostate adenocarcinoma are rare. Any cervical or suprasclavicular adenopathy in a male subject over 50 years of age should be biopsied and excised, followed by histological analysis including immunohistochemistry to look for PSA antibody positivity. This allows early management to be adapted and helps to improve the prognosis of these dreaded serious secondary tumours.
References
1. Benjamin C, J Madison, Amish Sura. 2001. Prostate Carcinoma metastatic to the cervical lymph nodes: Reportof two cases and review of the litherature. Am J Otolaryngol. 22: 1420-1423.
2. Guileyardo JM, Johnson WD, Welsh RA. 1980. Prevalence of latent prostate carcinoma in two us population. J Natl Cancer Inst. 65: 311-316. Ref.: https://pubmed.ncbi.nlm.nih.gov/6931251/
3. Mehra P, Cottrell DA, Booth DF. 1998. An unusual presentation of metastatic prostate cancer. J Oral Maxillo Surg. 65: 517. Ref.: https://pubmed.ncbi.nlm.nih.gov/9541357/ DOI: https://doi.org/10.1016/s0278-2391(98)90727-3
4. Hessan H, Strauss M, Sharkey F. 1986. Urogenital tract carcinoma metastatic to the head and neck. Laryngoscope. 96: 1352-1356. Ref.: https://pubmed.ncbi.nlm.nih.gov/3784739/ DOI: https://doi.org/10.1288/00005537-198612000-00007
5. Li Cy, Lam CT. 1980. Immunohistochemical diagnosis of prostatic cancer with metastasis. Cancer. 46: 706-712. Ref.: https://pubmed.ncbi.nlm.nih.gov/6156752/ DOI: https://doi.org/10.1002/1097-0142(19800815)46:4%3C706::aid-cncr2820460412%3E3.0.co;2-e
6. Rosental MA. 1998. Management of metastatic prostate. Cancer Med J Autralia. 169: 46-50. Ref.: https://pubmed.ncbi.nlm.nih.gov/9695702/ DOI: https://doi.org/10.5694/j.1326-5377.1998.tb141478.x
7. Rosenthal M. 2000. Advances in the management of prostate cancer. Aust N Z J Med. 30: 593-599. Ref.: https://pubmed.ncbi.nlm.nih.gov/11108070/ DOI: https://doi.org/10.1111/j.1445-5994.2000.tb00861.x
8. Budendorf L, SchopferA, WagnerU. 2000. Metastatic patterms of prostate cancer : An autopsy study of 1589 patients. Hum Pathol. 31: 578-583. Ref.: https://pubmed.ncbi.nlm.nih.gov/10836297/ DOI: https://doi.org/10.1053/hp.2000.6698
9. Flocks R, Boatman D. 1973. Incidence of head and neck metastasis from genito-urinary neoplasms. Laryngoscope. 83: 1527-1539. Ref.: https://pubmed.ncbi.nlm.nih.gov/4758761/ DOI: https://doi.org/10.1288/00005537-197309000-00011
10. Woo K, Wiectorek R, Turre P. 2001. Prostate adenocarcinoma presenting as a large supraclavicular mass. Rev Urol. 3: 102-105. Ref.: https://pubmed.ncbi.nlm.nih.gov/16985698/
11. Hematpour K, Bennett CJ, Rogr D. 2006. Heard CS Supraclavicular lymph node : incidence of unsuspected metastatic prostate cancer. Eur Arch Otorhinolaryngol. 263 : 872-874. Ref.: https://pubmed.ncbi.nlm.nih.gov/16830117/ DOI: https://doi.org/10.1007/s00405-006-0066-2
12. Chan G, Domes T. 2013. Supraclavicular lymphadénopathie as the initial presentation of metastatic prostate cancer : a case report and review of literature. Can Urol Assoc J. 7: 433-435.
13. Philips JK, Sabo A, Naraine R. 2018. Metastatic prostate cancer presenting as a virchow’s node. Asclepuis Med. 1: 1-3.
14. Haissam I, Mubaster I, Mohammad UI. 2019. Prostate cancer metastasis to cervical nod chain an unusual clinic pathological finding. J Ayub Med Coll Abbottabad. 31. Ref.: https://pubmed.ncbi.nlm.nih.gov/30868800/




















