Indexing & Abstracting
Full Text
Case ReportDOI Number : 10.36811/ojor.2021.110011Article Views : 74Article Downloads : 53
Trichilemmal cyst of the neck: case report and review of the literature
Othman El Houari*, Amal Hajjij, Ilias Tahiri, Mohamed Said Anajar, Loubna Taali, Mohammed Zalagh and Fouad Benariba
Otorhinolaryngology and Head and Neck Surgery Department, Cheikh Khalifa Hospital, University Mohammed 6 of Health Sciences, Casablanca, Morocco
*Corresponding Author: Othman El Houari, Otorhinolaryngology and Head and Neck Surgery Department, Cheikh Khalifa Hospital, University Mohammed 6 of Health Sciences, Casablanca, Morocco, Email: othman.elhouari@gmail.com
Article Information
Aritcle Type: Case Report
Citation: Othman El Houari, Amal Hajjij, Ilias Tahiri, et al. 2021. Trichilemmal cyst of the neck: case report and review of the literature. Open J Otolaryngol Rhinol. 3: 13-17.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2021; Othman El Houari
Publication history:
Received date: 05 August, 2021Accepted date: 17 August, 2021
Published date: 19 August, 2021
Abstract
Introduction: Trichilemmal cysts are lesions originating in the isthmus of the hair follicle. They are more common in women and occur in 90% on the scalp.
Presentation of case: A 10-year-old female patient presented with a hard, slightly painful, nonexophytic mass in the right cervical region (Ia). After surgical resection in healthy margins, the diagnosis of trichilemmal cyst was made on histopathological examination.
Discussion: The age of the patient as well as the cervical location of this type of lesion is an extremely rare presentation of trichilemmal cyst. Follow-up is rigorous in search of a triad: ichthyosis, keratosis, deafness, particularly in this patient.
Conclusion: Close follow-up in this clinical case is indicated because the risk of malignant degeneration and development of similar lesions is present.
Keywords: Follicular cyst; KID syndrome; Trichilemmal cyst; Neck surgery; Trichilemmal carcinoma
Introduction
Trichilemmal cysts (TCs) or pilar cysts, are lesions of the hair follicle filled with keratin. They originate from the outer root sheath of the pilar follicle. They occur in 5-10% of the population, with a female predominance [1] and may present a pattern of either autosomal dominant or sporadic inheritance [2] Trichilemmal cysts most often appear in areas with dense hair follicles. Thus, 90% occur on the scalp, while the face, groin, extremities and trunk are less frequently affected. Their clinical presentation includes non-neoplastic and aggressive forms, these latter are called proliferating trichilemmal cysts [3]. Aggressive forms are generally benign; however, cases of carcinomatous transformation have been reported [4]. Studies on trichilemmal cysts are few and published cases describe the clinical presentation, imaging findings and histology of these lesions [5]. Treatment is based on surgery with complete excision to prevent recurrence. We report here the case of a young patient who presented with a trichilemmal cyst, the particularity lies in the cervical seat (sub-mental territory) and the patient's age (10 years), representing an extremely rare presentation of this type of lesion.
Presentation of case
Patient M.O, 10 years old, presented 2 years before a mass of the right anterior cervical region (submental area) which gradually increased its size with subsequently remission and then reappearance of the mass with the same clinical characteristics. Clinical examination found a swelling of hard consistency 1 cm in diameter, non-exophytic, non-ulcerative, slightly painful to palpation. The opposite skin was not inflammatory and presented no drainage pore. The rest of the clinical examination, in particular of the integuments, scalp, trunk, perianal region, shoulder did not show a similar or other skin lesion. Ultrasound features revealed an oval hypoechoic lesion measuring 18 x 12 mm avascular with posterior enhancement. In our patient's history, no HPV + verrucous lesion, no notion of trauma or microtrauma, no prolonged sun exposure or skin irradiation was noted. No similar case after epidemiological investigation within the family was reported. The lesion was resected in one piece with respect of the capsular plane under general anesthesia. Intraoperatively, we found that the mass extended to the mylohyoid muscle behind and to the submandibular gland laterally without invading them.
The postoperative follow-up was simple
At 1 year postoperatively, ultrasound control showed no local recurrence and general examination did not find any other localization.
Discussion
We report the case of a rare localization of a trichilemmal cyst with review of the clinical, radiological, macroscopic and histopathological results of this type of lesion. Studies have shown that the majority of affected patients are women and that their average age is 44 years [6]. The most commonly affected site is the subcutaneous layer of the scalp [7]. The primary lesion arises from the follicular isthmus, but some authors have received patients with masses in the palm and fingers, where no hair follicle is present [8], as in our case. Appendages, trunk and the perianal region are exceptionally affected [7]. These lesions are usually slowly growing, asymptomatic or slightly painful, smooth and freely movable nodules in the scalp [8]. On ultrasound, trichilemmal cysts are firm and smooth with regular contours, the lesions are hypoechoic with characteristic echogenic foci, calcifications and posterior enhancement (Figure 1) [9]. The hair follicle in its isthmic part (between the opening of the sebaceous gland and the insertion of the erector pilaris muscle) has a sheath composed of an internal and an external segment. Trichilemmal cysts are benign cystic lesions, where the inner root sheath of the follicular isthmus disappears and the outer root sheath passes upon a specific form of keratinization known as trichilemmal [10]. Histologically, trichilemmal cysts are formed by eosinophilic keratin, opposed to the stratified keratin flakes present in epidermal cysts (1st etiology of follicular cyst) (Figure 2). Also, there is no longer a granular layer in contact with the cystic cavity, distinguishing trichilemmal cysts from epidermal cysts (Figure 3). Some authors have shown that trauma and inflammation can induce epithelial proliferation similar to that observed in pseudoepitheliomatous hyperplasia [11]. However, no traumatic history was found in our case. Proliferating trichilemmal tumors (main differential diagnosis) distinguish by clinical and histological characteristics which must suggest tumor aggressiveness: location other than the scalp (such as cervical), rapid growth, size greater than 5 cm, ulcerative and / or infiltrating character histologically [12]. Proliferating trichilemmal tumors can be benign or malignant, requiring in both cases appropriate therapeutic management.
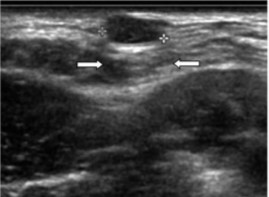
Figure 1: Ultrasound image of trichilemmal cyst: A lesion with regular contours, oval and homogeneous, with hypoechoic content and posterior reinforcement (arrows).
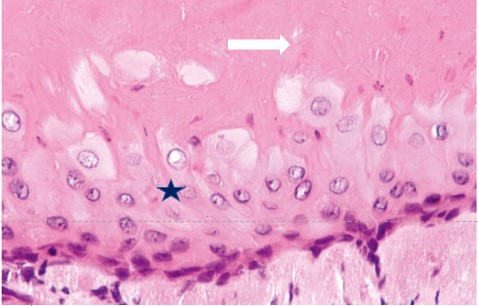
Figure 2: Histopathology of trichilemmal cyst: The cystic envelope is composed of a squamous epithelium made of large vertical cells (star) and the granular cell layer is absent. Keratin is eosinophilic and homogeneous (white arrow).
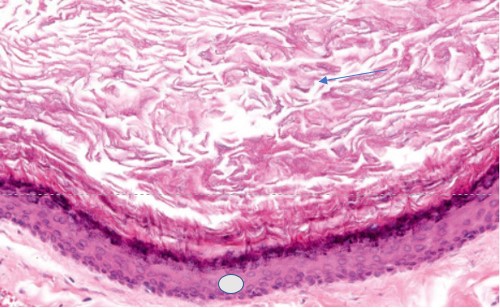
Figure 3: Histopathology of epidermoid cyst: The envelope of the cyst consists of a squamous epithelium and has a granular cell layer (circle). Note the laminated and stratified appearance of the intracity keratin (arrow).
Cellular atypia, mitosis and necrosis may be present
In addition, these tumors express capillary cytokeratin’s (cytokeratin 7) as well as CD34. Presence of a benign component bordered by an anaplastic one with anarchic development suggests carcinoma. The epidermoid cyst has a predilection site in the vulva and scrotum. Its consistency is soft and it presents a central punctum of sebum drainage [13]. The hybrid cyst is preferentially located in the eyelid [14]. Other differential diagnoses of follicular cysts include HPV + verrucous, dermoid and comedonal cysts. Complete resection of trichilemmal cysts and benign proliferating tumors is sufficient and curative with an excellent prognosis. However, no consensus is available to date for the management of proliferating malignant trichilemmal tumors given their rarity. Complete ablation with an excision margin in a healthy area is indicated. Neo-adjuvant radiotherapy with radical surgery may be indicated in metastatic cases. However, further studies of aggressive tumors similar to proliferating trichilemmal carcinoma are needed to establish the efficacy of neoadjuvant radiotherapy [12]. The peculiarity of our case lies in the age (10 years) of the patient. The other particularity of this clinical case lies in its location (cervical territory Ia), while approximately 90% of trichilemmal cysts occur in the scalp. Some patients with KID syndrome (keratitis, ichthyosis, and deafness) may present with trichilemmal tumors which can be malignant [15]. Ulceration, rapid and / or exophytic growth, extensive necrosis, infiltration, cellular atypia is suggestive of malignant transformation. This syndromic presentation justifies close follow-up in this young patient as well as a complete and regular dermatological examination (every 3 months) in search of another localization.
Conclusion
The trichilemmal cyst is the second most common type of follicular cyst (~ 10% to 15% of cases), historically referred to as a sebaceous cyst. Simple resection is most often curative. Clinically, it almost always occurs on the scalp, the cervical localization described in our case is a risk factor for proliferation. Close follow-up (ichthyosis, deafness, other cystic lesions) of our patient given her age (10 years) and the cervical localization is indicated because subjects with this triad are more prone to develop carcinomatous transformation of the trichilemmal cyst. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
1. Sadath HN, Ramachandra S, Kumar MA, et al. 2013. Multicentric calcified trichilemmal cysts with alopecia universalis affecting siblings. Indian J Dermatol Venereol Leprol. 79: 88-91. Ref.: https://pubmed.ncbi.nlm.nih.gov/23254735/ Doi: https://doi.org/10.4103/0378-6323.104675
2. Markal N, Kurtay A, Velidedeoglu H, et al. 1998. Malignant transformation of a giant proliferating trichilemmal tumor of the scalp: patient report and literature review. Ann PlastSurg. 41: 314- 316. Ref.: https://pubmed.ncbi.nlm.nih.gov/9746092/ Doi: https://doi.org/10.1097/00000637-199809000-00017
3. Mathis ED, Honningford JB, Rodriguez HE, et al. 2001. Malignant proliferating trichilemmal tumor. Am J ClinOncol. 24: 351-353. Ref.: https://pubmed.ncbi.nlm.nih.gov/11474259/ Doi: https://doi.org/10.1097/00000421-200108000-00006
4. Chang SJ, Sims J, Murtagh FR, et al. 2006. Proliferating trichilemmal cysts of the scalp on CT. AJNR Am J Neuroradiol. 27: 712-714. Ref.: https://pubmed.ncbi.nlm.nih.gov/16552022/
5. Kim HJ, Kim TS, Lee KH, et al. 2001. Proliferating trichilemmal tumors: CT and MR imaging findings in two cases, one with malignant transformation. AJNR Am J Neuroradiol. 22: 180-183. Ref.: https://pubmed.ncbi.nlm.nih.gov/11158906/
6. Wortsman X. 2012. Sonography of cutaneous and ungual lumps and bumps. Ultrasound Clin. 7: 505-523.
7. Melikoglu C, Eren F, Keklik B, et al. 2014. Trichilemmal cyst of the third fingertip: a case report. Hand Surg. 19: 131-133. Ref.: https://pubmed.ncbi.nlm.nih.gov/24641757/ Doi: https://doi.org/10.1142/s0218810414720113
8. Ikegami T, Kameyama M, Orikasa H, et al. 2003. Trichilemmal cyst in the pulp of the index finger: a case report. Hand Surg. 8: 253-255. Ref.: https://pubmed.ncbi.nlm.nih.gov/15002107/ Doi: https://doi.org/10.1142/s0218810403001765
9. He P, Chen W, Zhang Q, et al. 2020. Distinguishing a Trichilemmal Cyst from a Pilomatricoma with Ultrasound. Journal of Ultrasound in Medicine. 39: 1939-1945. Ref.: https://pubmed.ncbi.nlm.nih.gov/32333607/ Doi: https://doi.org/10.1002/jum.15298
10. Dewanda NK, Midya M. 2014. Baker’s dozen on the scalp: an interesting case of multiple trichilemmal cyst. J CutanAesthetSurg. 7: 67-68. Ref.: https://pubmed.ncbi.nlm.nih.gov/24761109/ Doi: https://doi.org/10.4103/0974-2077.129994
11. Perez LM, Bruce JW, Murrah VA. 1997. Trichilemmal cyst of the upper lip. Oral Surg Oral Med Oral Pathol Oral RadiolEndod. 84: 58-60. Ref.: https://pubmed.ncbi.nlm.nih.gov/9247952/ Doi: https://doi.org/10.1016/s1079-2104(97)90296-1
12. Satyaprakash AK, Sheehan DJ, Sangueza OP. 2007. Proliferating trichilemmal tumors: a review of the literature. Dermatol Surg. 33: 1102-110. Ref.: https://pubmed.ncbi.nlm.nih.gov/17760602/ Doi.: https://doi.org/10.1111/j.1524-4725.2007.33225.x
13. Ramakrishnaiah SB, Raiput SS, Gopinatan NS. 2016. Epidermoid cyst of the sole-A case report. J Clin Diagn Res. 10: 6-7. Ref.: https://pubmed.ncbi.nlm.nih.gov/28050432/ Doi: https://doi.org/10.7860/jcdr/2016/23225.8787
14. Requena L, Sánchez Yus E. 1991. Follicular hybrid cysts. Am J Dermatopathol. 13: 228-233. Ref.: https://pubmed.ncbi.nlm.nih.gov/1714246/ Doi: https://doi.org/10.1097/00000372-199106000-00003
15. Kim KH, Kim JS, Piao YJ, et. al. 2002. Keratitis, ichthyosis and deafness syndrome with development of multiple hair follicle tumors. Br J Dermatol. 147 : 139-143. Ref.: https://pubmed.ncbi.nlm.nih.gov/12100197/ Doi : https://doi.org/10.1046/j.1365-2133.2002.04724.x




















