Indexing & Abstracting
Full Text
Case ReportDOI Number : 10.36811/ojor.2019.110003Article Views : 1998Article Downloads : 30
A case with Chiari malformation 2 diagnosed with vertigo
Zeynep Özözen Ayas1*and Dilcan Kotan2
1Eskisehir City Hospital, Department of Neurology, Eskisehir, Turkey
2Sakarya University Training and Research Hospital, Department of Neurology, Sakarya, Turkey
*Corresponding author: Zeynep Özözen Ayas, Eskisehir City Hospital, Department of Neurology, Eskisehir, St. 71 Evler , Av. Çavdarlar, 26080, Odunpazari/Eskisehir Turkey, Tel: 05059039605; Email: zozozen@hotmail.com
Article Information
Aritcle Type: Case Report
Citation: Zeynep Özözen Ayas, Dilcan Kotan. 2019. A case with Chiari malformation 2 diagnosed with vertigo. Open J Otolaryngol Rhinol. 1: 13-14.
Copyright:This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2019; Zeynep Özözen Ayas
Publication history:
Received date: 31 January, 2019Accepted date: 19 February, 2019
Published date: 21 February, 2019
Introduction
Chiari malformations (CM) are a congenital anomally which posterior fossa structures are displaced from foroman magnum to the upper cervical spinal canal at different degrees [1]. (1) If there is accompanied by spinal dysraphism, it is defined as type 2. Symptoms occurs as a results of pressure on the cerebellum like as vertigo, ataxia, vision problems, headache. In some cases, medical therapy can be used to manage symptoms. Surgery is only treatment for decrease compression or stop progression. This malformation is frequently accompanied by syringomyelia, cystic spaces occur vertically in the spinal cord. In this article, a case with CM type 2, syringomyelia and multilacuner infarction with vertigo was discussed.
Case Report
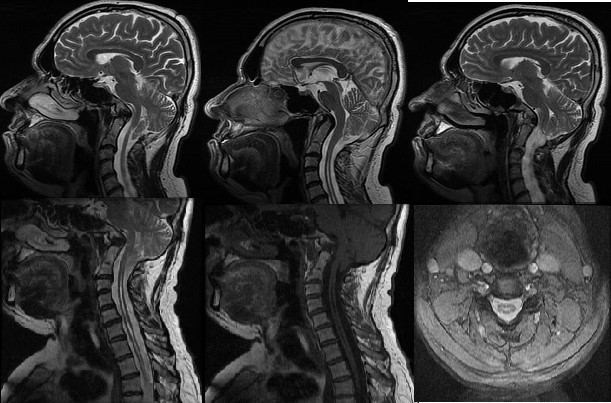
A 49-year-old male patient was admitted to hospital had vertigo for last 6 months. His symptom could be positional and lasting for hours. He noted that sometimes his vertigo distrup the patients’s daily life activity like as bend over. There was no nause and vomiting, hearing loss, and tinnitus. Also the patient had moderate headache for 3 years. Headache was localized nape of the neck and had no spread. There was no trigger and accompanying factor. Headache was not treat with analgesic medical theraphy. In his past medical history, he had head trauma history at the age of 7. Also, he was diagnosed with hypertension for 2 years. When he was treated with 2 antihypertensive theraphy with ramipril 5mg and amlodipine 10mg, he was normotensive. His neurological examination and laboratory tests were normal. Dix-Hallpike maneuver was negative. His audiogram and hearing test were normal. Cranial MRI revealed that multilacuner infarcts in periventriculer area and cervical syrinx cavity in cervical area with sagittal section. (figure 1) Cervical MRI was performed and long-segment syringomyelinosis (up to T2 vertebra) was observed in the spinal canal. (figure1) The patient was diagnosed with CM type 2. Surgical treatment was not adviced and followed with symtomatic theraphy.
Discussion
CM type 2 is thought to be due to defective occlusion and open neural tube [2]. The malformation is characterised by a displacement of brainstem, fourth ventricle and cerebellum through the foramen magnum. It is usually accompanied by corpus callosum anomalies. Asymmetric dilatation of lateral ventricles, auaduct stenoz or atresia, larger occipital horns than the frontal may be seen. Our patient had no cranial anomally except cerebellar herniation. Common symptoms of CM type 2 are upper cervical canal symptoms, brainstem, and cerebellar symptoms. Nape pain, scoliosis and tethered cord syndrome are important findings in adults [3]. The patient had non-specific symptoms like as vertigo and headache. These symptoms may also be seen in hypertensive headache, but he was normotensive with medical theraphy. His neurological examination was normal, so symptoms can be incidentally.The treatment of CM 2 varies according to symptoms and comorbid diseases. Shunt and decompressive surgery are important in cases with hydrocephalus and brainstem compression symptoms. No surgical treatment was needed in our patient. Syringomyelinosis is most seen in the lower cervical region, but may ocur in the all spinal cord. Atrophic spinal cord and relative large central canal are present. Syringomyelinosis have different symptoms and progressive clinical course. Pain, paresis, paresthesia, hydrocephalus and brainstem findings can be seen. Patients benefit from surgical approach [4].Syringomyelinosis was detected as long segment involvement on T2 veretebra on his MRI. Lacuner infarcts occurs as a result of hypoperfusion or ischemia of perforating arteries, basal ganglions, white matter of capsular interna and pons localized lesions. Silent lacuner infarcts are often seen in hypertensive patients and result of lypohyalinosis. Collagen accumulation in muscle cells deteriorates wall elasticity [5]. Similarly, our patient had hypertension. His brain MRI showed multilacuner infarcts. We emphasized te importance of the identifying the etiology with MRI, when patients present with common symptoms in neurology practice like as vertigo and headache which is localized, persistant and not treat with analgesic theraphy.
Figure 1: Cerebral CT-scan showing cerebral venous infarction.
References
- Chiari H. 1891. U?ber Vera?nderungen des kleinhirns infolge von hydrocephalie des grosshirns. Dtsch Med Wochenschr. 17:1172-1175. [Ref.]
- McLone DG, Knepper PA. 1989. The cause of of chiari 2 malformation: A unified theory. Pediatr Neuroscience.15: 1-12. [Ref.]
- Stevenson K. 20004. Chiari type II malformation: Past, present, and future. Neurosurg Focus. 16: 1-7. [Ref.]
- Jiang L, Xia C, Zhu WG, et al. 2019. Correlation between syrinx resolution after posterior fossa dekompression and cervical sagittal profile change in adolescents with Chiari malformation and syringomyelia. Zhonghua Yi Xue Za Zhi. 15: 183-187. [Ref.]
- Wardlaw JM. 2005. What causes lacunar stroke? J Neurol Neurosurg Psychiatry. 76 :617-619. [Ref.]




















