Indexing & Abstracting
Full Text
Case ReportDOI Number : 10.36811/ojgor.2020.110012Article Views : 30Article Downloads : 26
Management of placenta percreta. A case report
DIOUF A1,2,3*, Thiam O1, Ndour K3, Gueye M2,3, Ndiaye MD3, Niang D1, Sow DB1, Sarr CT1, Mbodj A3, Moreau JC3, Mbaye M2 and Konaté I1
1Regional Hospital Center of Saint-Louis, BP 401, Dakar, Senegal
2Philippe Maguilen SENGHOR health center, BP: 29026 or 8951 Aéroport Yoff, Dakar, Senegal
3Gynecological and Obstetric Clinic, EPS Aristide Le Dantec, BP 3001, Dakar, Senegal
*Corresponding Author: Dr Aliou DIOUF, Regional Hospital Center of Saint-Louis, BP 401, Tel: 002216412302; Email: alioudiouf69@yahoo.com
Article Information
Aritcle Type: Case Report
Citation: DIOUF A, Thiam O, Ndour K, et al. 2020. Management of placenta percreta. A case report. O J Gyencol Obset Res. 2: 01-04.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2020; DIOUF A
Publication history:
Received date: 06 January, 2020Accepted date: 09 January, 2020
Published date: 13 January, 2020
Introduction
The placenta accreta designates an abnormality of the placental insertion characterized, on the anatomopathological level, by an absence of deciduous deciduous between the placenta and the myometrium. This insertion anomaly may interest all or only part of the placenta. We distinguish within this terminology the terms of
- placenta accreta when the placenta is simply attached to the
Myometrium.
- placenta increta when the placenta invades the myometrium.
- placenta percreta when the placenta enters the serosa
uterine, or even the neighboring organs (bladder, peritoneum, etc.) [1]. Placentas accretas are a high-risk situation for severe postpartum hemorrhage and its inherent complications such as disseminated intravascular coagulation, hemostasis hysterectomy, surgical wounds to the ureters, bladder, multiple organ failure, or even maternal death, particularly in the case of placenta percreta [2,3]. Risk factors for placenta percreta include a history of cesarean, uterine curettage or manual removal of placenta, presence of placenta previa, endometriosis, high parity and advanced maternal age [4]. We report the case of a 30-year-old woman, IIGIIP, who had a previous cesarean section during her first pregnancy and who had a placenta percreta and who underwent hysterectomy without cystectomy and without ligation of the hypogastric arteries.
Observation
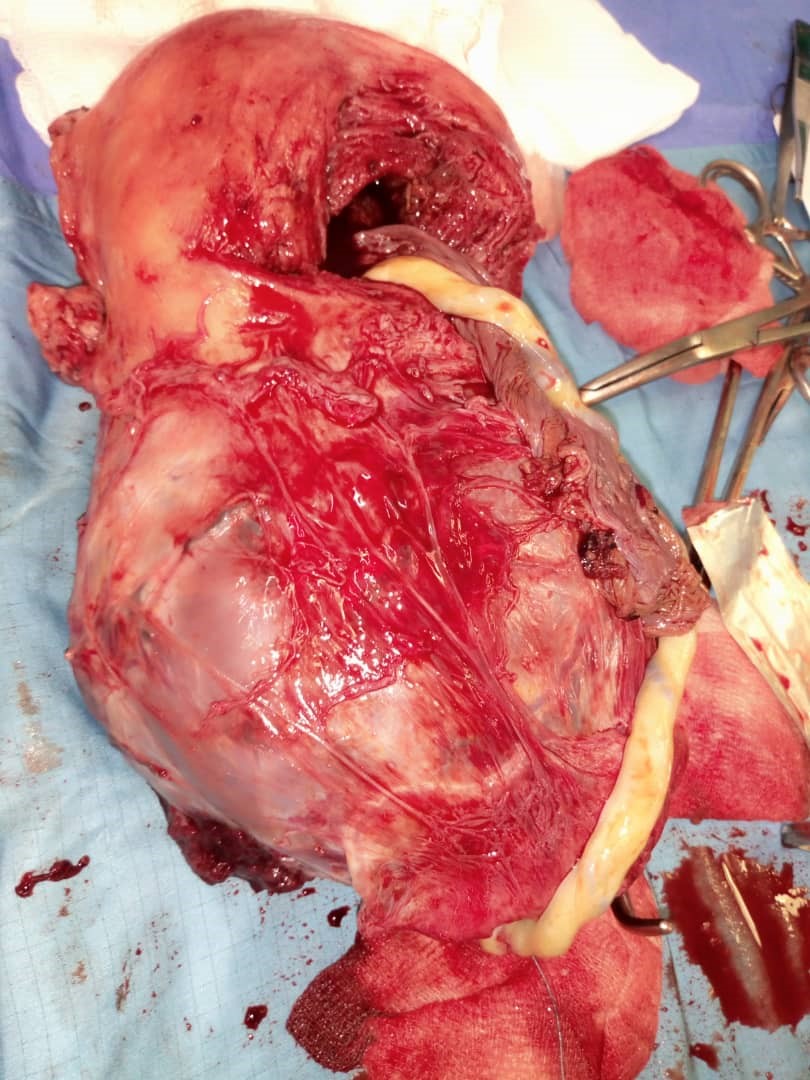
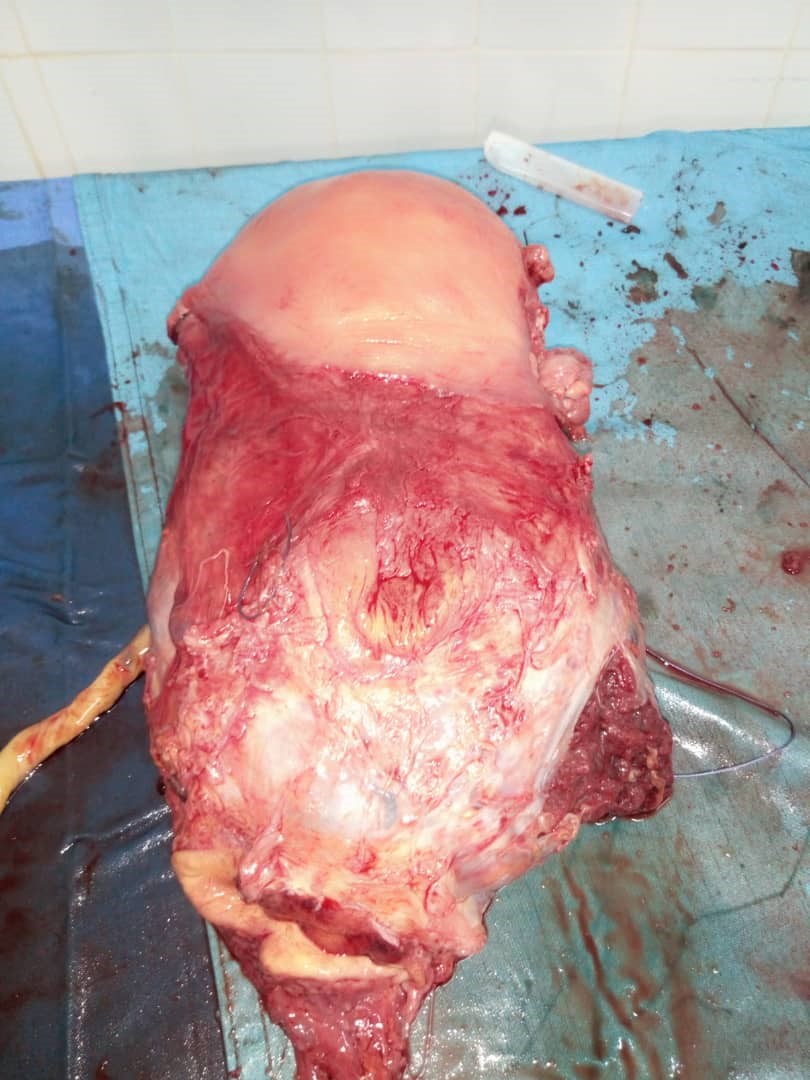
We report the case of a patient, 2nd gesture, 2nd parent, 30 years old, with a history of cesarean section 2 years ago received in our structure for the management of bleeding on a pregnancy of 31SA + 2 days. At 28 weeks of gestation, the ultrasound finds a marginal placenta previa. The patient was admitted to the ward for bleeding episodes twice at 28 and 30 weeks, but ultrasound did not reveal the placenta percreta. On admission, she complained of repeated vaginal bleeding but her general condition was preserved; the general condition was good, the normal-colored mucous membranes, the conscience clear. The obstetrical examination found a uterus with a long longitudinal axis, a uterine height of 27 cm, a palpated head in suprapubic and the seat at the level of the uterine fundus, the sounds of the fetal heart present and calculated at 140 beats per minute; on vaginal contact, the cervix was posterior, softened, semi-long with an internal opening barely open and admitting the pulp of the finger, and red blood at the fingertip. The pelvis was normal. Thus, it was a parturient, IIGIIP with one cesarean section in her history, in which the diagnosis of a marginal placenta previa was made on a non-term pregnancy. She received antenatal corticosteroid therapy and a preoperative workup for a semi-emergency cesarean. The Caesarean section performed using the Misgaw-Ladakh technique with transverse incision and extraction required a longitudinal fundic corporal hysterotomy. The placenta alone formed the usual lower segment area extending on the posterior surface of the bladder and subperitoneally, surrounding the uterus up to the two uterosacral ligaments. We performed a hysterectomy without cystectomy or ligation of the hypogastric arteries. Preoperative antibiotic therapy was administered and immediate postoperative follow-up was simple with no genital bleeding or hematuria. The patient was transferred to the intensive care unit and received an iso-group iso-rhesus blood transfusion with 4 pockets of pellet and 2 pockets of fresh frozen plasma. A pelvic control ultrasound did not show any sign of peritoneal effusion that would favor persistent bleeding. An anatomo-pathological examination of the operating room confirmed that it was indeed a percreta placenta.
Discussion
The placenta percreta is the rarest form of placental abnormalities representing 5% to 7% of all placenta accreta [5,6]. Well-known traditional risk factors for placenta percreta are a history of cesarean or uterine surgery, placenta previa, manual removal of the placenta, dilation and curettage, multiparity and advanced maternal age [5]. Our patient had well identified risk factors such as a previous cesarean and placenta preavia; her age being intermediate and she was pauciparous. However, in recent studies, IVF pregnancy is newly recognized as an independent risk factor for accelerated placenta [7,8]. Uterine rupture due to placenta percreta is very rare, occurring in 1 in 5000 pregnancies, and it occurs mainly later in the second and third trimester. Its occurrence during the first trimester is rarely described [9,10]. Our patient did not experience a uterine rupture during pregnancy but rather endless episodes of bleeding that motivated a cesarean for placenta previa. The main clinical features of uterine rupture often include signs of shock, severe abdominal and pelvic pain associated with vaginal bleeding [11]. In front of a placenta accreta, a hysterectomy associated with a cystectomy is often performed, sometimes associated with ligation of the hypogastric arteries. Chauveaud-Lambling described a management of a percreta placenta extending on the posterior face of the bladder and in subperitoneal surrounding the uterus until the two uterosacral ligaments, bulging in the cul-de-sac of Douglas or a conservative treatment was carried out with a placenta left in place. Ligation of the hypogastric arteries and round ligaments was performed in conjunction with an in situ injection of Methotrexate [12]. In our patient, a radical treatment using the electrosurgical unit was done with a satisfactory hemostasis; reason why the hypogastric arteries were not ligated. Conservative management in the event of placenta accreta is very advantageous in order to preserve the subsequent fertility of patients [13]. In our case, and perhaps in all cases of placenta percreta, for the sake of avoiding catasclismic hemorrhage, conservative treatment could not have been done even if the patient was pauciparous with two living children. In our African societies, although multiparity is strongly anchored in mentalities and this can often make the surgeon doubt, the life of the patient and the child must remain at the center of care. A similar case of placenta percreta invading the bladder was reported by Jaffe R in the American Journal of Obstetrics and Gynecology [14] with failure of conservative treatment and resumption at 7 weeks by hysterectomy, partial cystectomy and ureteral reimplantation. Ligation of the hypogastric arteries was also performed.
Another case was reported in Obstetrics and Gynecology by Legros RS in 1994 [15] for which the development was more favorable. The placenta percreta had been diagnosed at the time of the attempt of manual delivery after natural delivery; it had been left in place. MRI confirmed the total invasion of the myometrium and the patient was treated with weekly doses of Methotrexate (610 mg total dose). The ultrasound inversion of the placenta was very slow (several months) compared to the rapid drop in the blood level of βHCG. Eight months after delivery, a hysteroscopy was performed to remove the residues and two years later, the patient delivered again by natural means without abnormal delivery.

Conclusion
At present, it is quite difficult to suggest a standard course of action for the placenta percreta. The majority of publications on this subject are clinical cases. If a conservative treatment is better indicated in front of a woman wanting a pregnancy, it is important to know how to assess the clinical situation of the patient and the risk of cataclysmic hemorrhage to preserve her vital prognosis.
References
1. Oyelese Y, Smulian JC. Placenta previa, et al. 2006. Obstet Gynecol. 107: 927-41.
2. O’Brien JM, Barton JR, Donaldson ES. 1996. The management of placenta percreta: conservative and operative strategies. Am J Obstet Gynecol. 175: 1632-1637. Ref.: https://bit.ly/2utMmhC
3. Hudon L, Belfort MA, Broome DR. 1998. Diagnosis and management of placenta percreta: conservative and operative strategies. Am J Obstet Gynecol. 53: 509-517. Ref.: https://bit.ly/37JX5CU
4. Morken NH, Henriksen H. 2001. Placenta percreta-two cases and review of the literature. Eur J Obstet Gynecol Reprod Biol. 100: 112-115. Ref.: https://bit.ly/39TMlUz
5. Miller DA, Chollet JA, Goodwin TM. 1997. Clinical risk factors for placenta previa-placenta accreta. Am J Obstet Gynecol. 177: 210-214. Ref.: https://bit.ly/2uvjllJ
6. Timor-Tritsch IE, Monteagudo A. 2012. Unforeseen consequences of the increasing rate of cesarean deliveries: early placenta accreta and cesarean scar pregnancy. A review. Am J Obstet Gynecol. 207: 14-29. Ref.: https://bit.ly/37DuSh4
7. Fitzpatrick KE, Sellers S, Spark P, et al. 2012. Incidence and risk factors for placenta accreta/increta/ percreta in the UK: a national case-control study. PLoS One. 7: 52893. Ref.: https://bit.ly/2QycXT5
8. Esh-Broder E, Ariel I, Abas-Bashir N, et al. 2011. Placenta accreta is associated with IVF pregnancies: a retrospective chart review. BJOG. 118: 1084-1089. Ref.: https://bit.ly/36LdPcE
9. Gardeil F, Daly S, Turner MJ. 1994. Uterine rupture in pregnancy reviewed. Eur J Obstet Gynecol Reprod Biol. 56: 107-110. Ref.: https://bit.ly/2s9FHZe
10. Dabulis SA, McGuirk TD.2007. An unusual case of hemoperitoneum: uterine rupture at 9 weeks gestational age. J Emerg Med. 33: 285-287. Ref.: https://bit.ly/2utPSbO
11. Jang DG, Lee GS, Yoon JH, et al. 2011. Placenta percreta-induced uterine rupture diagnosed by laparoscopy in the first trimester. Int Jmed Sci. 8: 424-427. Ref.: https://bit.ly/35A84NQ
12. Chauveaud-Lambling A, Antonetti-N’Diaye E, de Rudnicki S, et al. 2005. Prise en charge des placentas percreta. J Gynecol Obstet Biol Reprod. 34 : 346-350. Ref.: https://bit.ly/2QyeI2D
13. Morken NH, Henriksen H. 2001. Placenta percreta-two cases and review of the literature. Eur J Obstet Gynecol Reprod Biol. 100: 112-115. Ref.: https://bit.ly/2N7m7E3
14. Jaffe R, DuNeshter B, Sherer DM, et al. 1994. Failure of methotrexate treatment for term placenta percreta. Am J Obstet Gynecol. 171: 558-559. Ref.: https://bit.ly/2FuVrcf
15. Legro RS, Price FV, Hill LM, et al. 1994. Nonsurgical management of placenta percreta: a case report. Obstet Gynecol. 83: 847-849. Ref.: https://bit.ly/39T0Ckm




















