Indexing & Abstracting
Full Text
Research ArticleDOI Number : 10.36811/ojgor.2019.110001Article Views : 3560Article Downloads : 38
Gestational weight gain and pregnancy outcome in women with excessive pre-pregnancy body mass index
Magdalena Smyka, Katarzyna Kosinska-Kaczynska*, Damian Warzecha and Miroslaw Wielgos
Department of Obstetrics and Gynecology, Medical University of Warsaw, Warsaw, Poland
*Corresponding author: Katarzyna Kosinska-Kaczynska Ph.D. MD, Department of Obstetrics and Gynecology, Medical University of Warsaw, Pl.Starynkiewicza 1/3, 02-015 Warsaw, Poland, Tel.: +48 22 5830 301; Fax: +48 22 5830 302; Email: kkaczynska@wum.edu.pl
Article Information
Aritcle Type: Research Article
Citation: Magdalena S, Katarzyna K, Damian W, et al. 2019. Gestational weight gain and pregnancy outcome in women with excessive pre-pregnancy body mass index. O J Gyencol Obset Res. 1: 01-07.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2019; Magdalena Smyka
Publication history:
Received date: 08 December, 2018Accepted date: 14 December, 2018
Published date: 02 January, 2019
Abstract
Aim: To evaluate the effects of gestational weight gain on perinatal outcomes in woman with excessive pre-gravid body mass index.
Material and Methods: The study group consisted of 197 overweight or obese women who delivered full-term newborns at the 1st Department of Obstetrics and Gynecology, Medical University of Warsaw. Group A included 89 (45.2%) women with inadequate or adequate weight gain. Group B included 108 patients (54.8%) with excessive weight gain during pregnancy.
Results: No significant differences in the occurrence of gestational diabetes, hypertension or intrahepatic cholestasis between the analyzed groups were observed. Excessive weight gain was positively correlated with the incidence of cesarean delivery (67.6% vs 32.4%, p=0.009), newborns’ birthweight (3627g±519 vs 3406g±521, p=0.009) and the risk of low for gestational age infants (26.9% vs 12.4%, p=0.01). The highest risk of low for gestational age new born was related to gestational weight gain of about 15 kg. Appropriate preconception counselling for overweight and obese women may reduce the risk of low for gestational age infants.
Keywords: Pre-pregnancy excessive weight; Gestational weight gain; Pregnancy outcomes; Birthweight; Large for gestational age
Introduction
Excessive weight is one of the main factors affecting general health and leading to reduction in daily activity. Nowadays, overweight and obesity have reached the epidemic level in both developed and developing countries. According to the World Health Organization the incidence of an overweight has increased trice in the last two decades. These days there are 1,6 billion overweight people and over 500 millions obese ones around the world [1]. Among pregnant women 55 % are normal weight,7% underweight and 38% obese [2]. The relation between overweight or obesity and diseases such as atherosclerosis,hypertension, heart diseases, diabetes, metabolic syndrome and musculoskeletal system disorders is well known. A relation between excessive body mass index and pregnancy complications, like gestational diabetes (GDM), pregnancy hypertension (PH) or preeclampsia (PE) is well established [3]. During delivery obese women have greater risk of injuries, cesarean section, shoulder dystocia or wound’s infections [4]. Excessive mother’s weight is a risk factor of large for gestational age infants [5]. Obese pregnant women are less likely to have a spontaneous onset of labour, so induction of labour is more common in obese pregnant woman than in normal weight ones [6]. The Institute of Medicine (IOM) recommends a gestational weight gain of 12.5-18.0 kg (28-40 Ib) for underweight woman, 11.5-16 kg (25-35 lb) for women with normal weight, 7.0-11.5 kg (15-25 lb) for overweight women, and 5.0- 9.0 kg (11-20 lb) for obese women [7]. The recommendations were developed on the basis of observational studies and the is still a need for them to be verified. The aim of this study was to evaluate the effect of gestational weight gain on perinatal outcome in women with excessive prepregnancy body mass index (BMI), who gave birth at the 1st Department of Obstetrics and Gynecology, Medical University of Warsaw.
Materials and Methods
All women in singleton pregnancies with pre-pregnancy BMI above 25 kg/m2, who gave birth ≥ 36 weeks of gestation at the 1st Department of Obstetrics and Gynecology of Warsaw Medical University in 2016 and 2017 have been subjected to retrospective analysis. The exclusion criteria were: incomplete medical data, unverified by first trimester ultrasound scan gestational age, delivery before completing 36 weeks of gestation and multiple pregnancy.
Pre-gravid weight was defined as weight before conception or <10 weeks of gestation. The patients were asked to provide their pre-gravid weight. It was verified by comparing to the weight measured by medical staff during the first trimester of pregnancy and provided in the patient’s medical records. The weight at delivery was measured with light clothing and shoes off. Height was reported by the patients themselves and verified by medical staff.BMI was calculated by dividing the body mass by the square of the body height. Normal weight was defined as BMI 18.5- 24.9, underweight as BMI less than 18.5,overweight as 25.0-29.9, and obesity as BMI 30 and greater.
The main study group was divided into two subgroups according to gestational weight gain. The first subgroup included women with adequate or inadequate weight gain during pregnancy and the second one was composed of women with excessive weight gain according to OIM recommendations [7]. In order to avoid bias related to a different weight gain in cases of preterm delivery, as weight gain is related to the duration of pregnancy, only women delivering beyond 36 gestational weeks were included in the study. The study outcomes included: occurrence of GDH, PH, PE and intrahepatic cholestasis of pregnancy (ICP), cesarean delivery, blood loss during delivery, small for gestational age (SGA), adequate for gestational age (AGA) and large or gestational age (LGA) newborns. GDM diagnosis was based on the results of the fasting 75 g oral glucose tolerance test (OGTT) performed during 24-28 gestational week in every patient. One or more elevated level was sufficient for a diagnosis of GDM: fasting plasma glucose ≥5.1 mmol/l (92 mg/dl), 1-hour plasma glucose ≥10.0 mmol/l (180 mg/dl) or 2-hour plasma glucose ≥8.5 mmol/l (153 mg/dl). PH was defined as a systolic blood pressure ≥140mmHg and/or diastolic blood pressure ≥90 mmHg in at least two measurements and diagnosed after 20 weeks of gestation. PE diagnosis is defined as PH with proteinuria (>300 mg of protein in a 24-hour urine sample) or without proteinuria but with one of the adverse organ’s conditions: evidence of kidney dysfunction (oliguria, elevated creatinine levels >1.1 mg/dl), impaired liver function (noted by liver function tests), thrombocytopenia (platelet count <100.000/microliter), pulmonary edema or cerebral or visual disturbances. ICP diagnosis was based on pruritus, elevated serum aminotransferases and bile acid levels with onset in the second or third trimester of pregnancy, and spontaneous relief of signs and symptoms within two to three weeks after delivery. AGA defined infants with birth weight between the 10th and 90th percentiles for the gestational age. Infants weighing below 10th percentiles for gestational age are defined as SGA, and the ones weighting above 90th percentiles for the gestational age are defined as LGA. Preterm delivery was defining as a labor before completing 37 weeks of gestation. Variables were described as mean (±standard deviation), median or percentage. The Mann-Whitney test (for continuous variables) and the Fischer’s exact test (for categorical values) were used for the statistical analysis. P-values <0.05 were considered significant. A relationship between gestational weight gain as continuous variable and neonatal birthweight was examined. Data were analysed using Statistica version 13.1.
Results
Among the 206 women studied, 197 (95.6%) met the inclusion criteria.108 (55.3%) of them were overweight and 89 (44.7%) were obese. Group A included 89 patients (45.2%): 41 (46%) women with inadequate weight gain and 48 (54%) with adequate weight gain. Group B included patients with excessive weight gain during pregnancy (108 women, 54.8%). Basic characteristics of the study groups are presented in Table 1.
| Table 1: Basic characteristics of the study groups | |||
|---|---|---|---|
| Group A n=89 | Group B n=108 | ||
| Mean ± SD *n (%) | Mean±SD *n (%) | p | |
| Age | 31.9±3.7 | 32.9±6.1 | 0.7 |
| BMI | 34.78±3.91 | 27.41±1.24 | <0.001 |
| Weight gain (kg) | 9.07±6.5 | 12.87±6.01 | <0.001 |
| Week of delivery | 38.12±1.64 | 38.96±1.3 | <0.001 |
| Parity * primiparous multiparous | 39 (43.8%) 50 (56.2%) | 44 (40.7%) 64 (59.3%) | 0.6 |
| BMI - body mass index | |||
| Table 2: Pregnancy outcomes of women from group A and B. | ||||
|---|---|---|---|---|
| Study group n=197 | Group A n=89 | Group B n=108 | ||
| n (%) *mean±SD | n (%) *mean±SD | n (%)*mean±SD | p | |
| GDM | 34 | 16 (18 %) | 18 (16.7%) | 0.8 |
| GH | 29 | 11 (12.4%) | 18 (16.7%) | 0.4 |
| PE | 4 | 2 (2.2%) | 2 (1.9%) | 1 |
| ICP | 3 | 3 (3.4%) | 0 (0%) | 0.09 |
| Caesarean delivery | 116 | 43 (48.3%) | 73 (67.6%) | 0.009 |
| Blood loss* | 526±208 | 476±206 | 524±205 | 0.09 |
| Birthweight* | 3602±512 | 3406±521 | 3627±519 | 0.003 |
| SGA | 9 | 5 (5.6%) | 4 (3.7%) | 0.7 |
| LGA | 40 | 11 (12.4%) | 29 (26.9%) | 0.01 |
| GDM - gestational diabetes mellitus; GH - pregnancy hypertension; PE - preeclampsia; ICP - intrahepatic cholestasis of pregnancy; SGA - small for gestational age; LGA - large for gestational age | ||||
Pregnancy outcomes of women from group A and B are presented in Table 2. Women with excessive weight gain had significantly more often cesarean delivery (67.6% vs 32.4%, p=0.009) and delivered newborns with higher birthweight (3627g±519 vs 3406g±521, p=0.003). Excessive weight gain was related to higher risk of having an LGA newborn, while no relationship with having an SGA infant was observed.
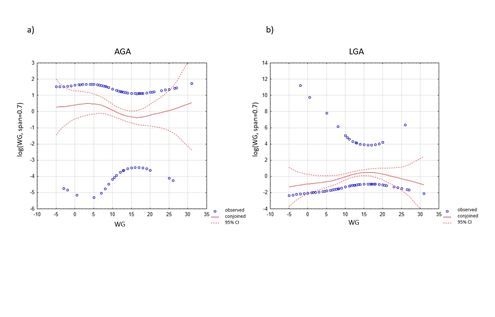
Linear association between neonatal birthweight and maternal gestational weight gain was assessed using generalized additive models and is presented in Figure 1. A non-linear relation was observed between maternal weight gain and the prevalence of AGA and LGA infants. Weight gain up to 10 kg was associated with increased prevalence of AGA newborns, while between 10 and 25 kg increased the risk of having LGA infant. The highest risk of delivering LGA newborn was related to gestational weight gain of about 15 kg.
Figure 1: Linear association between neonatal birthweight and maternal gestational weight gain.
Discussion
Our study confirmed that excessive weight gain during pregnancy among women with increased pre-gravid BMI is a risk factor of cesarean birth and delivering an LGA newborn. The relation between excessive weight gain and the risk of operative delivery is well established in overall population [8]. Similar finding were published in women with excessive BMI. Kiel at el. conducted a cohort study of 120,251 women and found that gestational weight gain below 15 lb (6.75 kg) was associated with lower risk of caesarean delivery [9].
Several studies confirm the higher incidence of operative delivery in women with excessive GWG. Research on Swedish pregnant women showed that intrapregnancy weight gain above the recommended by IOM levels increased the risk of emergency cesarean section in women with normal weight, overweight or obesity [10]. Excessive weight gain during pregnancy and obesity both decreased the rates of vaginal birth after cesarean one [11].
Women whose GWG is above the recommended ranges may also experience various adverse maternal outcomes, such as gestational diabetes mellitus, gestational hypertension or preeclampsia, as also other long-term consequences such as increased risk for type 2 diabetes and cardiovascular disease [7]. The abnormal BMI of women in the first trimester of pregnancy is associated with the risk of adverse perinatal outcome. Obese pregnant women are more likely to have a higher risk of preeclampsia, need of induction of labor, cesarean section, preterm delivery and LGA than the women with a normal pre-gravid BMI [12]. Flick et al. evaluated pregnancy outcomes among 20,823 obese women with excessive weight gain during pregnancy. His analysis demonstrated a greater frequency of cesarean section and LGA, but also gestational diabetes mellitus, preterm delivery and very low for gestational age [13]. Studies evaluating GWG across different classes of obesity, found insufficient weight gain or even weight loss during pregnancy associated with a decreased risk of preeclampsia, postpartum hemorrhage, instrumental, and cesarean section, and postpartum weight retention [14].
Unique in our study is the analysis of relation not only between newborn birth weight and gestational weight gain below or above recommended ranges, but also weight gain as a continuous variable. It allows to investigate the impact of maternal GWG on the prevalence of AGA infants. We found that weight gain of about 15 kg in mothers with excessive BMI is related to the highest risk of delivering LGA infants. Comparing to Kiel et al. research, the minimal risk of occurrence specific pregnancy outcomes like LGA, caesarean delivery or preeclampsia corresponded to gaining 4.5-15.5 kg (10-25 pounds) and 0-4.1 kg (0-9 pounds) for obesity class I (BMI of 30-34.9), and obesity classes II and III, respectively (BMI of 35-39.9 and BMI of 40 or greater respectively) [9]. According to IOM recommended gain weight of 5.0-9.0 kg (11-20 lb) for women with pre-pregnancy BMI more than 30, IOM do not differentiate between class I, class II, and class III obesity. Given the limited data by class, the IOM recommended weight gain of 5-9.0 kg (11-20 lb) is given for all obese women. The committee concluded that low gain or weight loss during pregnancy is not recommended for obese women because of the potential for irreversible effects on child neurologic development [7]. The risks for SGA and preterm births increased with decreasing gestational weight gain in all women [15].
The limitation of the study is a small study group from a single academic centre. Only women delivering above 36 weeks of gestation were included in the study, leaving a group of preterm deliveries out of analysis. Deliveries below 36 weeks were excluded in order to avoid bias related to a difference in weight gain in different durations of pregnancies. However, the analyzed period of deliveries above 36 weeks may still have a significant impact on gestational weight gain.
Another recommendation for weight gain during pregnancy were proposed by Bracero and Byrne [16]. The analysis of 20,971 pregnant women who deliver between 1987 and 1993 at a single institution in New York City showed that for overweight or obese women a gain of 26-30 pounds (11-13 kg) was associated with optimal outcome. According to DeVader the ideal gestational weight gain for population of normal weight women was 11.4-15.5 kg (25-34 pounds) [17]. Finally, Norh et al. analysis over 60 000 pregnant women indicates that greater weight gains (more than 16 kg) and high pre-gravid maternal BMI decreased the risk of growth restriction and increased the risk of the infant's being born large-for-gestational-age or with a low Apgar score. Generally, low GWG was advantageous for the mother, but it increased the risk of having a small baby, particularly for underweight women [18].
Conclusions
Excessive GWG affects the course of pregnancy and it is correlated with perinatal outcomes. It seems crucial to pay attention to reaching normal weight in pre-pregnancy period and gaining recommended weight according to pre-gravid BMI.
References
- World Health Organization., 2013. Obesity and overweight. Fact Sheets No 311. [Ref.]
- Goldstein RF, Abell SK, Ranasinha S, et al., 2017. Association of Gestational Weight Gain with Maternal and Infant Outcomes A Systematic Review and Meta-analysis. JAMA, 317: 2207-2225. [Ref.]
- Gaillard R, Durmus B, Hofman A, et al. 2013. Risk Factors and Outcomes of Maternal Obesity and Excessive Weight Gain During Pregnancy. Obesity. 21: 1046-55. [Ref.]
- Miko?ajek-Bedner W, Marcinkiewicz O, Zapa?owska M, et al. 2010. Effect of obesity on pregnancy, delivery and birth status of a newborn baby. Neonatologia i Ginekologia. 3: 201-214. [Ref.]
- Hajduk M, 2012. The influence of body mass on female fertility. Endokrynologia, Oty?o?? I Zaburzenia Przemiany Materii. 8: 93-97. [Ref.]
- Schrauwers C, Dekker GJ, 2009. Maternal and perinatal outcome in obese pregnant patients. J Matern Fetal Neonatal Med. 22: 218-226. [Ref.]
- Institute of Medicine. 2009. Weight Gain During Pregnancy: Re-examining the Guidelines. Washington: DC, The National Academies Press. [Ref.]
- Lynes C, McLain AC, Yeung EH, et al. 2017. Interpregnancy weight change and adverse maternal outcomes: a retrospective cohort study. Ann Epidemiol. 27: 632-637. [Ref.]
- Kiel DW, Dodson EA, Artal R, et al. 2007. Gestational weight gain and pregnancy outcomes in obese women: how much is enough? Obstet Gynecol. 110: 752-758. [Ref.]
- Nilses C, Persson M, Lindkvist M, et al. 2017. High weight gain during pregnancy increases the risk for emergency caesarean section-Population-based data from the Swedish Maternal Health Care Register 2011-2012. Sexual & Reproductive Healthcare. 11: 47-52. [Ref.]
- Juhasz G, Gyamfi C, Gyamfi P, et al. 2005. Effect of Body Mass Index and Excessive Weight Gain on Success of Vaginal Birth After Cesarean Delivery. Obstetrics & Gynecology. 106: 741-746. [Ref.]
- Yazdani S, Yosofniyapasha Y, Nasab BH, et al. 2012. Effect of maternal body mass index on pregnancy outcome and newborn weight. MC Research Notes. 5: 34. [Ref.]
- Flick AA, Brookfield KF, de la Torre L, Tet al. 2010. Excessive Weight Gain among Obese Women and Pregnancy Outcomes. Am J Perinatol. 27: 333-338. [Ref.]
- Moehlecke M, Costenaro F, Reichelt A, et al. 2016. Low Gestational Weight Gain in Obese Women and Pregnancy Outcomes. AJP Rep. 6: 77-82. [Ref.]
- Rasmussen KM, Abrams B, Bodnar LM, et al. 2010. Recommendations for weight gain during pregnancy in the context of the obesity epidemic. Obstet Gynecol. 116: 1191-1195. [Ref.]
- Bracero LA, Byrne DW. 1998. Optimal maternal weight gain during singleton pregnancy. Gynecologic and Obstetric Investigation. 46: 9-16. [Ref.]
- DeVader SR, Neeley HL, Myles TD, et al. 2007. Evaluation of gestational weight gain guidelines for women with normal prepregnancy body mass index. Obstetrics and Gynecology. 110: 745-751. [Ref.]
- Nohr EA, Vaeth M, Baker JL, et al. 2008. Combined associations of prepregnancy body mass index and gestational weight gain with the outcome of pregnancy. Am J ClinNutr. 87: 1750-1759. [Ref.]




















