Indexing & Abstracting
Full Text
Research ArticleDOI Number : 10.36811/ojdoh.2022.110008Article Views : 0Article Downloads : 2
Radiological assessment of Nasopalatine Canal and Incisive Foramen Morphology Using Cone Beam Computed Tomography- A descriptive study
Manisha Saxena* and Dr. Shilpi Srivastava BDS
*Corresponding Author: Manisha Saxena, India; Email: drmanisha.saxena@yahoo.com
Article Information
Aritcle Type: Research Article
Citation: Manisha Saxena. 2022. Radiological assessment of Nasopalatine Canal and Incisive Foramen Morphology Using Cone Beam Computed Tomography- A descriptive study. Open J Dent Oral Health. 4: 11-23.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2022; Manisha Saxena
Publication history:
Received date: 02 December, 2022Accepted date: 20 December, 2022
Published date: 22 December, 2022
Abstract
The aim of this study was to analyse the three dimensional anatomical and morphometric dimensions of nasopalatine canal (NPC) in the sagittal, axial and coronal plane directions using cone beam computed tomography (CBCT) and to evaluate the effect of age, gender and maxillary dental status on NPC and buccal bone thickness (BBT) of anterior maxilla.
Objective: To evaluate the shape, diameter and length of NPC, shape and diameter of Incisive foramen and width of buccal bone anterior to NPC in relation to age, gender and dental status.
Methods: One hundred and ten CBCT scans of patients with ages ranging from 18 to 65 years were analyzed for the study. The measurements of NPC were obtained from CBCT scans.
Results: The mean labio-palatal SF diameter ranges from 3.09±1.47 (0.9 mm– 8.7mm). The mean IF diameter of all the subjects in our sample group was 3.47±1.03 mm (1.5mm–6.2 mm). As the age of person increases the diameter if IF also increases in our study. The mean NPC length in our study was 11.48±2.69 mm (4.0mm–19.5 mm). Mean NPC length in males was 12.58 mm±2.25mm (5.1mm–21.10 mm) while it was 10.34±2.65 mm (4.0–19.5 mm) in females. The mean Buccal bone thickness at IF level (BBT1) measurement was 6.08±1.58 mm (2.3mm–9.5 mm), the buccal bone thickness at SF level (BBT2) measurement was 8.36±2.50 mm (3.8–14.6 mm). The most common shapes of NPC were cylindrical in sagittal plane. The round shape of IF was seen in axial plane. Mesio-distal diameter of IF in male was 3.86±1.11 and in female 3.81±1.20 mm. NPC shape in coronal plane showed Type 1 as the most common type.
Conclusions: The study showed that CBCT scans and their analysis help the clinician to make a better radiographic diagnosis and clinical application while using surgical procedures, such as implant placement and osteotomies for orthodontic or prosthetic purpose.
Introduction
Nasopalatine canal (NPC) is funnel shaped opening in the bone of the oral hard palate opens through the incisive foramen in the oral cavity, and into the nasal cavity as the foramina of Stenson. The location of the foramen is also variable and it can be seen going from the apical portion of central incisors up to the adjacent alveolar crest [1]. From fourth to tenth intrauterine week series of changes takes place to separate the oral cavity from nasal cavity by palato-genesis with the formation of the primary and secondary palates.By the sixth embryonic week, the primary palate will be formed by the fusion of the medial nasal processes. The definitive structures arising from the primary palate are the nasal septum, the pre-maxillary bone, the central incisors, and the upper lip. Secondary palate forms from the maxillary processes, arising from the first pharyngeal pouch, produce vertical mesenchymal tissue outgrowths called palatal shelves. They continue to grow horizontally and unite in midline. Collectively, the fusion of these palatal shelves results in the formation of the secondary palate. The complete fusion of the primary and secondary palates occurs at the 12th embryonic week [2]. Thus, communication between the mouth and nasal cavity persists and marks the position of the incisive fossa. Microscopically, the duct is usually lined with a ciliated columnar epithelium from the nasal floor to the palatal opening, where the lining is replaced with transitional and then squamous cell epithelium [3]. Regarding theory of development Radlanski et al [4]. conducted study on seven human embryos, at weeks seven to twentyfour, demonstrated that during embryogenesis, the incisive canal was derived from the primary palate within the pre-maxillary bone.
Structures present in nasopalatine canal
Neurovascular structures traversing this canal include the nasopalatine nerve providing sensory input to the pterygopalatine ganglion, from the mucosa of the hard palate and gingiva around the incisors up to the canine teeth and a vascular anastomosis between the posterior septal branch of the sphenopalatine artery and the greater palatine artery. Beauty of the face is enhanced by natural teeth. Any lost teeth need to be replaced. Earlier RPD and FPD were used but now a days implants have emerged as new treatment modality. Complications and anatomic limitations were reported during implant placement in maxillary incisor region due to close proximity of NPC. Implant contact with the neural tissue may lead to sensory dysfunction and osseointegration failure which could affect the success of implants in the aesthetically demanding anterior region [6]. The buccal bone plate thickness anterior to the incisive fossa from a clinical standpoint is of interest. CBCT studies have demonstrated that maxillary tooth loss markedly reduces buccal bone plate thickness. Therefore, we can understand in a way that buccal bone thickness is positively co-related with maxillary tooth loss and canal length is negatively related [5].
Radiologic evaluations of incisive canal anatomy
Craniofacial radiography is essential for the assessment of gross pathology or anatomy interrogation for the planning of craniofacial surgery or restorative dental procedures. Imaging modalities of the maxillofacial region include X-rays with periapical or panoramic views, CT, and magnetic resonance imaging (MRI). Of these, CBCT is the best way to evaluate the incisive canal giving better highresolution images, eliminating image superimposition, offering less radiation exposure, and providing better analysis of bone quality. CBCT is a recent technology. Imaging is accomplished by using a rotating gantry to which an x-ray source and detector are fixed. A divergent pyramidal- or coneshaped source of ionizing radiation is directed through the middle of the area of interest onto an area x-ray detector on the opposite side. The x-ray source and detector rotate around a rotation fulcrum fixed within the centre of the region of interest. During the rotation, multiple (from 150 to more than 600) sequential planar projection images of the field of view (FOV) are acquired in a complete, or sometimes partial, arc. This procedure varies from a traditional medical CT, which uses a fanshaped x-ray beam in a helical progression to acquire individual image slices of the FOV and then stacks the slices to obtain a 3D representation. Each slice requires a separate scan and separate 2D reconstruction [5].
Materials and Methodology
The study was prepared using 110 CBCT scans, which were taken from October 2019 to August 2020. The subjects were between the ages of 18-65 years, and their scans were taken for various routine investigations or treatment. The scans were acquired using the Kodak 9300 CS unit (Carestream Health Inc., Rochester, New York) machine and were processed on a computer using the Kodak dental imaging software 3D module (Version 2.4.10, Carestream Health Inc., 2007). The exposure parameters were set at 90 kVp, 12 mA, and voxel size of 300-500.The study has been approved by IRB and Ethical clearance certificate is attached. (RDCH/Ethical/2020/0551A) The study followed specific inclusion criteria. Good diagnostic-quality CBCT scans of patients aged 18 -65 years were selected with 53 males and 51 females. The inclusion criteria were patients with periodontal diseases, partially and completely edentulous for implant planning were included. Patients with severe atrophy, residual roots, cleft palate, jaw fractures, a pathologic lesion in the premaxillary region, receiving orthodontic treatment or orthodontic surgery, embedded teeth were excluded from the study. Also, nondiagnostic CBCT scans and scans with any artifacts and faulty images were excluded. The participants were asked to remove all metal objects in the vicinity of oral and maxillofacial region and were asked to wear a lead apron with thyroid collar. The patient position is accurate the mid-sagittal plane was adjusted using laser beam for a vertical alignment and the horizontal plane laser beam for a Frank fort plane alignment. The tube voltage ranged from 68-90kvp, tube current was 4mA and an exposure time of 11.30sec was used. Tube voltage was altered depending upon the physique of patient and presence of metallic structures such as crowns, implants etc. this will result in exposure which ranged from 697- 1585 m Gy cm2. The patients were divided into 3 groups as 18-33 years, 34 -49 years and 50 – 65 years. The gender of the individuals was recorded. In addition, individuals were classified and recorded in three groups according to their dental status: Group 1: individuals with only one maxillary central incisor; Group 2: individuals with missing both central incisors; Group 3: individuals with both maxillary central incisors present. The parameters described in table 1 was studied.
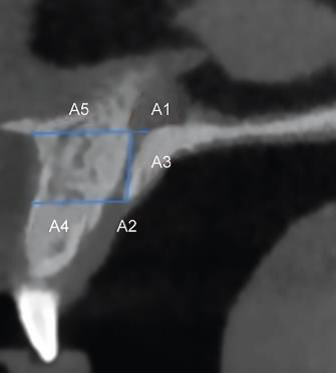
Figure 1: Description and explanation of parameters
|
Table 1: Description of parameters. |
|
|
Parameter |
Description |
|
SAGGITAL PLANE 1. Labio-palatal diameter of the canal at the nasal fossa level (A1) 2. Labio- palatal diameter of the canal at the Incisive fossa. (A2) 3. Length of Canal (A3) 4. Width of the buccal bone at IF (A4) 5. Width of buccal bone at SF (A5) 6. Shape of canal AXIAL PLANE 7. Medio-lateral diameter of IF 8. Shape of Incisive Foramen CORONAL PLANE 9. Type of canal |
The inner diameter measured at the level of the nasal fossa. The inner diameter measured at the level of the hard palate. Measured between the floor of the nasal fossa and the level of the hard palate along the long axis of the canal. Buccal Bone thickness measured in sagittal view at hard palate level. Buccal bone thickness at nasal level. Cylindrical, Spindle, Hour-glass, banana The inner diameter measured at the level of the hard palate. Heart shaped, lobulated, round, oval. Type1, Type 2, Type 3. |
Analyses of morphometric dimensions and variations of NPC
The anteroposterior diameters or labio-palatal diameter of the Stenson foramen (SF) or Incisive foramen (IF), and the length of the NPC were measured in millimetres using the reformatted sagittal CBCT images according to Bornstein et al [7]. The labio-palatal diameter of Stenson foramen A1, Labio-palatal diameter of Incisive foramen A2, length of canal A3, buccal bone width at SF A4 and buccal bone width at IF A5, shape of canal was observed in sagittal plane. The medio-lateral diameter of IF and shape of IF was noted in axial plane. The type of canal as single, double or bifurcated at SF was observed in coronal plane. These parameters are depicted in Figure 1-3. The length of the NPC was measured by the line drawn from the midpoint of SF to the midpoint of IF. The shapes of the canal were examined in sagittal sections and classified into four groups based on the classification of Mardinger et al [8], classified the NPCs in four groups (hourglass, funnel, banana, cylinder) in the sagittal sections.

Figure 2: The classification of NPC based on sagittal sections of CBCT images, A: cylindrical B: banana C: hourglass D: funnel

Figure 3: Measurement of mesio-distal diameter of Incisive foremen in axial section.
Parameters in Axial plane
The mesiodistal diameter was assessed in axial plane as shown in Figure 3. The Incisive foramen shape (round, oval, heart-shaped and lobular) was determined using the axial section as mentioned in Salemi et al study. [9]
Parameters in Coronal plane
The anatomic variants of the canal were differentiated into three groups (A) a single canal; (B) two parallel canals; (C) variations of the Y-type of canal with one oral/palatal opening (¼incisive foramen) and two or more nasal openings (¼foramina of Stenson). This classification is according to Bornstein et al [7] as seen in Figure 4.

Figure 4: Anatomic Classification of NPC morphology: A single canal (Type A), Two separate canals (Type B) and Y shape canals (Type C)
Statistical analysis
The collected data was entered in excel sheet to prepare master chart and was subjected for a statistical analysis. All statistical analyses were performed using the IBM SPSS Statistics 26 (SPSS Company, Illinois, USA) programme. Descriptive statistical evaluations were calculated for all measurements (mean, standard deviation, minimum and maximum values, etc.). Continuous variables are summarized as mean and standard deviation while categorical/ numerical data as percentages.
Unpaired “T test”, one way “ANNOVA test” were used for analysis of continuous variables whereas “CHI-SQUARE test” were used for categorical/ numerical values. Differences in measurements between genders were compared using independent t-test. Differences of parameters in patients of varied age and dental status groups were analyzed using analysis of variance (ANOVA). The results were evaluated at 95% confidence interval; significance level was assumed at p < 0.05. A p value <0.05 was considered to be statistically significant and a p value <0.001 is considered to be highly statistically significant.
Results
Total sample size taken for the study was n=104 in which 53 were males (50.9%) and 51were females (49.1%). The statistical study was divided into three age groups, 18-33years, 34-49 years and 50-65 years with mean age of 50.6 years.
Morphometric evaluation of NPC in sagittal plane
The mean labio-palatal SF diameter ranges from 3.09±1.47 (0.9 mm– 8.7mm). Mean SF diameter in males was 3.083±1.34 while in female mean was 3.098±1.612. The correlation of SF was not statistically significant with the gender, age and dental status.
• The mean IF diameter of all the subjects in our sample group was 3.47 ± 1.03 mm (1.5mm–6.2 mm). As the age of person increases the diameter of IF also increases in our study. It is not statistically significant with gender and dental status but IF diameter is increasing with age and is statistically significant (p < 0.01) • The mean NPC length in our study was 11.48 ± 2.69 mm (4.0mm– 19.5 mm). Mean NPC length in males was 12.58 mm ±2.25mm (5.1mm–21.10 mm) while it was 10.34 ±2.65 mm (4.0–19.5 mm) in females. There was a statistically highly significant difference between males and females in terms of canal length (p < 0.001). Males have relatively large craniocaudal dimensions. • When the influence of age on the canal length was assessed, it was observed to be decreasing with age. Younger individuals are found to have significantly greater length of incisive canal when compared to older individuals. (p = 0.55)
The NPC diminution including the length and the diameter of oral opening (A2 and A3) were significantly greater among men.
Buccal bone palate thicknesses at the front of oral opening of the canal (A4) of men were also significantly greater than that in women.
In our study, the mean Buccal bone thickness at IF level (BBT1) measurement was 6.08 ± 1.58 mm (2.3mm–9.5 mm), the buccal bone thickness at SF level (BBT2) measurement was 8.36 ± 2.50 mm (3.8–14.6 mm). (Table2). In males, the mean BBT1 measurement was 6.33 ±1.69 mm while it was 5.81 ±1.43 mm in females. The BBT1 measurements showed statistically significant differences according to dental status (p < 0.01).
The mean BBT2 measurement in males was 8.27 ±2.82 mm while it was 8.44 ±2.14 mm in females. In both genders, BBT1 and BBT2 measurements are not statistically significant. BT1 is statistically significant with age (p < 0.03). Buccal bone thickness is decreasing with age as seen in table 2. • The effect of dental status is related with buccal bone thickness. The values of BBT1 is showing statistically highly significant relation (p = .000) and BBT2 is statistically significant (p < .05) relation. (Table 2). It means that with loss of teeth buccal bone thickness decreases.
|
Table 2: The distribution of individuals according to gender, age groups and dental status. |
|||||||
|
Gender |
Age-groups |
Dental status groups |
Total |
||||
|
|
1 |
2 |
3 |
1 |
2 |
3 |
|
|
Male |
22 |
10 |
21 |
12 |
6 |
35 |
53 |
|
Female |
18 |
12 |
21 |
4 |
7 |
40 |
51 |
|
1 (CI missing) 2 (Both CI absent) 3 (Both present) |
|||||||
Shape of NPC in sagittal plane
• Of the 104 individuals, regarding NPC shape in sagittal plane 8 (7.71%) hourglass, 58 (55.80%) cylinders, 28 (26.9%) funnel, 10 (9.6%) bananas. While the most common shapes of NPC were cylindrical in females (29 individuals, 56.9%) and males (29 individuals, 54.7%). The gender had no statistical influence on NPC shapes (p > 0.05).
NPC patterns were given by gender, age group and dental status. When the canal form was evaluated according to age, the individuals in all age group cylindrical shape was more prevalent than funnel, hourglass and banana and least common was hour glass shape of NPC shapes. NPC formations did not show a statistically significant difference according to age groups (p > 0.05). There was a statistically significant difference in the shape of the canal compared to the dental status (p = 0.003) (Table 3,4).

Figure 5: Graphical distribution of NPC shape in population.
|
Table 3: - The mean values of nasopalatine canal dimensions according to the general, gender, age group and dental status. |
|||||
|
|
A1 (SF dia) |
A2 (IF dia) |
A3 (NPC Length) |
A4(BB1) |
A5(BB2) |
|
Gender |
3.083+1.34 |
3.616+1.09 |
12.58+2.25 |
6.337+1.69 |
8.279+2.82 |
|
Male 53 |
|||||
|
Female 51 |
3.098+1.612 |
3.335+0.96 |
10.34+2.65 |
5.819+1.43 |
8.449+2.14 |
|
p- value |
0.959 |
0.167 |
0.000 |
0.096 |
0.732 |
|
Test applied |
t test |
|
|
|
|
|
Age-groups |
2.942+1.25 |
3.252+1.07 |
11.772+2.40 |
6.595+1.52 |
8.055+2.22 |
|
1. 40 |
|||||
|
2. 22 |
2.981+1.36 |
3.218+0.84 |
11.622+2.37 |
5.854+.962 |
8.445+2.56 |
|
3. 42 |
3.288+1.72 |
3.830+1.01 |
11.145+3.10 |
5.716+1.79 |
8.611+2.74 |
|
p-valve |
0.534 |
0.016 |
0.558 |
0.031 |
0.598 |
|
Test applied |
Oneway ANOVA |
|
|
|
|
|
Dental status |
2.80+1.64 |
3.26+1.09 |
11.40+1.45 |
5.90+1.13 |
7.037+2.47 |
|
1. 16 |
|||||
|
2. 13 |
3.53+2.12 |
3.68+0.89 |
12.31+3.99 |
4.41+1.81 |
7.75+3.02 |
|
3. 75 |
3.08 +1.32 |
3.48+1.05 |
11.28+2.54 |
6.38+1.48 |
8.778+2.32 |
|
p-value |
0.435 |
0.578 |
0.449 |
0.000 |
0.025 |
|
Test applied |
Oneway ANOVA |
|
|
|
|
Morphometric evaluation of Incisive foramen (IF) Shape and Mesio-distal width in axial plane.
• The study of axial plane showed four types of shape of IF. The round shape of IF is common in males (n=25) and females (n=26). Lobulated shape of IF was least common as shown in Figure 5,6. The shape of IF in axial plane is not significant statistically in context to gender, age and dental status.
• Mesio-distal diameter of IF in male was 3.86 ±1.11 and in female 3.81±1.20 and are not significant statistically.MD diameter is greater in males in comparison to female. However, mesio-diatal diameter of IF increases with age and is statistically highly significant. (p=.003). Dental status of patient is not having any influence on of medio- lateral diameter IF.

Figure 6: Graphical representation of IF in axial plane according to gender.
|
Table 4: The distributions of mesio-distal diameter of IF (incisive foramen) in axial plane according to gender, age and dental status. |
|||||||||||
|
Mesio-distal diameter of IF |
Gender |
Age-group |
Dental status |
||||||||
|
M F p |
1 2 3 p |
1 2 3 p |
|||||||||
|
3.86 |
3.81 |
0.83 |
3.39 |
3.89 |
4.23 |
0.003 |
3.41 |
4.30 |
3.86 |
0.130 |
|
Morphometric evaluation of Type of NPC in coronal plane.
• Type 1 was the most prevalent type of NPC among the study cases and Type 2 was the least frequent one (71% versus 11%) (Figure 7).

Figure 7: Distribution of type if NPC in coronal plane in respect to gender.
Discussion
Maxillary anterior teeth play an important role in the development of esthetics of an individual. These teeth are more vulnerable to get fractured. With the advent of implants in dentistry, the replacement of missing maxillary anterior teeth has become easy. In recent years, CBCT imaging system has become popular in the evaluation of anatomic structures, such as the IF, NPC, mandibular canal, and mental foramen. CBCT is less costly with lower radiation dose compared to CT, while providing valuable images.
Our study consisted of 104 individuals of which 53 were males and 51 females. The present study showed the most predominant shape of the canal was cylindrical shaped (56%) followed by funnel shaped (26 %), banana-like (10%) and hour-glass shaped (8%) which was consistent with Safi et al [10] Guncu et al [11] Kajan et al [12] and Soumya et al [13] and Tozum et al. [14] In contrast to these studies Jayachandran et al [6] and Rai A et al [15] scans and found funnel shape was the commonly observed shape in 51% of cases followed by cylindrical shape in 17%. The current study showed mean NPC length was 11.48±2.69 mm. The males have 12.58±2.25mm while it was 10.34 ±2.65 mm in females. Males showed significantly more length as compared with females. The reason could be due to normal anatomic variation. According to the statistical findings, age and dental status showed no relationship with the canal length, but the difference in canal length between men and women was highly statistically significant (p<0.001). These findings are consistent with previous studies Song et al and Safi et al [10] and Kajan et al [12] Mishra et al [17] and Bornstein et al [7] reported in their study that the length of NPC decreases as the age advances. Panda et al [18] and Etoz et al [19] in their study stated that age does not influence the length of the canal. In our study length of canal is decreasing with age but not significant statistically.
The mean labio-palatal dimension of SF opening was registered as 3.09 ± 1.47 mm (0.9 – 8.7 mm) in our study. The diameter of SF in male was 3.083 ± 1.34 mm and in female 3.098 ± 1.612 mm. Age, gender relation and dental status was not statistically significant related to SF diameter. The mean labio-palatal dimension of IF in our study was 3.47 ± 1.03 mm (1.5–6.2 mm). It means there is increase in diameter from NPC canal on going from nasal cavity to oral cavity. The labio-palatal diameter of IF in males was 3.616±1.09 and in females 3.335±0.96. The mesio-distal diameter of IF was 3.86 ± 1.0 in males and 3.81 ± 0.9 in females. Mraiwa et al [21] Bornstein et al [7] (4.4–4.6 mm) and Güncü et al [11] reported that male had significantly larger mean canal diameter as compared to female. The authors found that gender difference was only true for the labiopalatal width, but not applicable to the mesio-diatal width.
Our study results are consistent with Bornstein et al. and Liang et al [20] who also concluded that the diameter of the canal in males was greater than that detected in females. Gender wise no statistically significant difference was seen in mesio-diatal dimension of IF; however, the mean diameter was greater in males. Panda et al, Rao et al [24] Khojastepour et al [22] and Gopal and Kapoor also reported similar significant differences. Since IF diameter is generally less than 6 mm, in cases in which this dimension exceeds 10 mm, pathologic circumstance may be considered. The current study concluded that buccal bone thickness at incisive foramen A4 was 6.08 ± 1.58 mm and buccal bone thickness at Stenson foramen A5 was 8.36 ± 2.50 mm showing an increase in bone thickness as we go higher towards Stenson foramen, contributing a tapering presentation superio-inferiorly. The result of present study correlates with that published by various researchers such as Panda M et al, Bronstein et al and Acar and Kamburo?lu [23] in their study found that buccal bone plate is affected by gender. Males were known to have higher values for buccal bone thickness. Such a finding indicates that female patients need more precautions during surgical procedures. In our study gender is not significantly associated with width of buccal cortical plate.
In our study the advancing age shows thinning of buccal cortical plate at level of incisive foramen A4 and was statistically significant (p= .03) In Al-Amery et al. also concluded in his study that age affects significantly the average anterior maxillary bone thickness, whereby it was noted to be thicker in young patients e.g 8.54 mm in 15-25 years, but reduced 24% to 6.49mm when compared to subjects above 55 years ANOVA; P < 0.001). In our study the width of the buccal bone wall gradually increased from cases with missing central incisors, to cases with one missing central incisor, to cases with both central incisors present it was in line with Bonstein et al. The ongoing study showed most common shape of incisive foramen on axial view of CBCT images was round (52.5%), followed by heart (35%) oval (7.5%), and lobular (5.0%). Kim et al [5] and Wani et al [25] also found round shape of IF to be most common shape. The last parameter of our study is type of NPC in coronal plane. The current study showed single canal as the most commonly seen canal 71.1%, Y shaped canal being the second common 18.3% and two parallel separate canal was least common 10.6%. Similar results were obtained in previous studies.
Conclusion
CBCT is now a well-accepted diagnostic tool for care of dental patients. CBCT is capable of providing accurate submillimetre resolution images in formats allowing 3-D visualization of the complexity of the maxillofacial region. All the current generation of the CBCT units are less bulky, the patient either sits or stand upright during the scan, better stabilization devices for the head and chin, using smaller, flat panels silicone detector with better image quality, variable KV, option for voxel size, FOV dimensions, scan timer and more powerful software application for the care of dental patients. Therefore, CBCT scans comprehensively evaluate the anatomical landmarks and their possible variations in the maxillofacial region should be considered to avoid postoperative surgical complications. In preoperative implant planning, for bone harvesting or bone grafting procedures, CBCT cross sectional images provides more information on anatomical landmarks.
References
1. Dler Abdurrahman Mohammed. 2016. Anatomical Variation in the Dimension of Nasopalatine Canal on Cone Beam Computed Tomography CBCT Images among Sulaimani Population. Acta Medica International. 3: 2.
2. Sasha Lake, Joe Iwanaga, Shogu Kikuta, et al. 2018. The Incisive Canal: A Comprehensive Review. 10: e3069. Ref.: https://pubmed.ncbi.nlm.nih.gov/30280065/ DOI: https://doi.org/10.7759/cureus.3069
3. Moacyr Tadeu. 2009. Unilateral patent nasopalatine duct: a case report and review of the literature. American Journal of Otolaryngology–Head and Neck Medicine and Surgery. 30: 137-140. Ref.: https://pubmed.ncbi.nlm.nih.gov/19239956/ DOI: https://doi.org/10.1016/j.amjoto.2008.02.015
4. Radlanski RJ, Emmerich S, Renz H. 2004. Prenatal morphogenesis of the human incisive canal. Anatomy and Embryology. 208: 265-271. Ref.: https://pubmed.ncbi.nlm.nih.gov/15293047/ DOI: https://doi.org/10.1007/s00429-004- 0389-y
5. Kim GT, Hwang EH, Lee SR. 2004. A study of incisive canal using a cone beam computed tomography. Korean J Oral Maxillo-dac Radiol. 34: 7-12.
6. Sadakashram Jayachandran, Sangeetha Ramamoorthy. 2019. CBCT evaluation of morphological characteristics of Nasopalatine canal and its related structure- A hospital based retrospective study. JIDA - Journal of Indian Dental Association. 13: 4.
7. Bornstein MM, Balsiger R, Sendi P, et al. 2011. Morphology of the nasopalatine canal and dental implant surgery: a radiographic analysis of 100 consecutive patients using limited cone-beam computed tomography. Clin Oral Impl Res. 22: 295. Ref.: https://pubmed.ncbi.nlm.nih.gov/21039896/ DOI: https://doi.org/10.1111/j.1600- 0501.2010.02010.x
8. O Mardinger, N Namani-Sadan, G Chaushu, et al. 2008. “Morphologic changes of the nasopalatine canal related to dental implantation: a radiologic study in different degrees of absorbed maxillae,” Journal of Periodontology. 79: 1659–1662. Ref.: https://pubmed.ncbi.nlm.nih.gov/18771366/ DOI: https://doi.org/10.1902/jop.2008.080043
9. Fateme Salemi Fazele Atarbashi Moghadam. 2016. Three-dimensional Assessment of the Nasopalatine Canal and the Surrounding Bone Using Cone-beam Computed Tomography.J Periodontal Implant Dent. 8: 1-7.
10. Yaser Safi, Mahkameh Moshfeghi. 2017. Assessment of Nasopalatine Canal Anatomic Variations Using Cone Beam Computed Tomography in a Group of Iranian Population. Iran J Radiol. 14: e37028.
11. GNG ¨unc¨u, YD Yildirim, HG Yilmaz, et al. 2013. Is there a gender difference in anatomic features of incisive canal and maxillary environmental bone? Clinical Oral Implants Research. 24: 1023-1026. Ref.: https://pubmed.ncbi.nlm.nih.gov/22587805/ DOI: https://doi.org/10.1111/j.1600- 0501.2012.02493.x
12. ZD Kajan, J Kia, S Motevasseli, et al. 2015. Evaluation of the nasopalatine canal with cone-beam computed tomography in an Iranian population. Dental Research Journal. 12: 14-19. Ref.: https://pubmed.ncbi.nlm.nih.gov/25709669/ DOI: https://doi.org/10.4103/1735- 3327.150289
13. Penala Soumya, Pradeep Koppolu, Krishnajaneya Reddy Pathakota, et al. 2019. Maxillary Incisive Canal Characteristics: A Radiographic Study Using Cone Beam Computerized Tomography. Hindawi Radiology Research and Practice. 5. Ref.: https://pubmed.ncbi.nlm.nih.gov/31032120/ DOI: https://doi.org/10.1155/2019/6151253
14. TFT ¨oz¨um, GNG ¨unc¨u, YD Yildirim, et al. 2012. Evaluation of maxillary incisive canal characteristics related to dental implant treatment with computerized tomography: a clinical multicenter study. Journal of Periodontology. 83: 337-343. Ref.: https://pubmed.ncbi.nlm.nih.gov/21910596/ DOI: https://doi.org/10.1902/jop.2011.110326
15. Arpita Rai Thakur, Krishna Burde, Kruthika Guttal, et al. 2013. Anatomy and morphology of the nasopalatine canal using cone-beam computed tomography. Imaging Science in Dentistry. 43: 273- 281. Ref.: https://pubmed.ncbi.nlm.nih.gov/24380067/ DOI: https://doi.org/10.5624/isd.2013.43.4.273
16. Mishra R, Thimmarasa VB, Jaju PP, et al. 2017. Influence of gender and age on nasopalatine canal: A cone-beam computed tomography study. J Dent Implant. 7: 15-19.
17. Mousumi Panda, Thatapudi Shankar. 2018. Cone beam computerized tomography evaluation of incisive canal and anterior maxillary bone thickness for placement of immediate implants. J Indian Prosthodont Soc. 18: 356-363. Ref.: https://pubmed.ncbi.nlm.nih.gov/30449964/ DOI: https://doi.org/10.4103/jips.jips_167_18
18. M Etoz, Y Sisman. 2014. Evaluation of the nasopalatine canal and variations with cone-beam computed tomography. Surgical and Radiologic Anatomy. 36: 805-812. Ref.: https://pubmed.ncbi.nlm.nih.gov/24488202/ DOI: https://doi.org/10.1007/s00276-014- 1259-9
19. Liang X, Jacobs R, Martens W, et al. 2009. Macro- and micro-anatomical, histological and computed tomography scan characterization of the nasopalatine canal. J Clin Periodontol. 36: 598-603. Ref.: https://pubmed.ncbi.nlm.nih.gov/19538333/ DOI: https://doi.org/10.1111/j.1600- 051x.2009.01429.x
20. Mraiwa N, Jacobs R, Van Cleynenbreugel J, et al. 2004. The nasopalatine canal revisitedusing 2D and 3D CT imaging. Dentomaxillofac Radiol. 33: 396-402. Ref.: https://pubmed.ncbi.nlm.nih.gov/15665234/ DOI: https://doi.org/10.1259/dmfr/53801969
21. Leila Khojastepour, Abdolaziz Haghnegahdar. 2017. Morphology and Dimensions of Nasopalatine Canal: a Radiographic Analysis Using Cone Beam Computed Tomography. J Dent Shiraz Univ Med Sci. 18: 244-250. Ref.: https://pubmed.ncbi.nlm.nih.gov/29201966/
22. Acar B, Kamburo?lu K. 2015. Morphological and volumetric evaluation of the nasopalatinal canal in a Turkish population using cone-beam computed tomography. Surg Radiol Anat. 37: 259- 265. Ref.: https://pubmed.ncbi.nlm.nih.gov/25038838/ DOI: https://doi.org/10.1007/s00276-014- 1348-9
23. Jaligama B Rao, Pramod Tatuskar. 2018. Radiographic Assessment of Anatomy of Nasopalatine Canal for Dental Implant Placement: A Cone Beam Computed Tomographic Study. The Journal of Contemporary Dental Practice. 19: 301- 305. Ref.: https://pubmed.ncbi.nlm.nih.gov/29603703/
24. Wani B A, Altaf Hussain Chalkoo. 2018. Morphometric analysis of nasopalatine canal using cone beam computed tomography. Indian journal of research. 7: 1991-2250.
25. Sekerci AE, Buyuk SK, Cantekin K. 2014. Cone-beam computed tomographic analysis of the morphological characterization of the nasopalatine canal in a pediatric population. Surg Radiol Anat. 36: 925-932. Ref.: https://pubmed.ncbi.nlm.nih.gov/24590491/ DOI: https://doi.org/10.1007/s00276-014- 1271-0




















