Indexing & Abstracting
Full Text
Short CommunicationDOI Number : 10.36811/jcshd.2020.110016Article Views : 14Article Downloads : 15
Brucella tricuspid endocarditis: Case report
Lakehal Redha*, Bendjaballah Soumaya, Khaled Khacha, Aziza Baya, and Brahami Abdelmallek
Department of Heart Surgery, EHS Dr Djaghri Mokhtar, Constantine, Algeria, Faculty of Medicine Constantine 03, Constantine, Algeria
*Corresponding Author: Lakehal Redha, Department of Heart Surgery, EHS Dr Djaghri Mokhtar, Constantine, Algeria, Email: lakehal.redha@gmail.com
Article Information
Aritcle Type: Short Communication
Citation: Lakehal Redha, Bendjaballah Soumaya, Khaled Khacha, et al. 2020. Brucella tricuspid endocarditis: Case report. J Cardiovasc Surg Heart Dis. 2: 06-11.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2020; Lakehal Redha
Publication history:
Received date: 21 February, 2020Accepted date: 03 March, 2020
Published date: 05 March, 2020
Abstract
Objectives: Brucella tricuspid endocarditis is a very rare. The diagnostic is made by serology and echocardiography (TTE). This new report case is an opportunity for us to make a reminder of this little-known entity among cardiologists and heart surgeon.
Methods: We report the case of 15-year-old children who present persisant fever and dyspnea. The physical exam found asystolic murmur, chest X-ray showed cardiomegaly, TTE demonstrated vegetations in chordate, papillary muscle, infundibulum, and left pulmonary artery with tricuspid insufficiency III, pulmonary angiography: proximal emboli of left pulmonary artery, positives blood culture: Brucella meltiness and serology positive. Excision of tricuspid and pulmonary vegetations and tricuspid repair under cardiopulmonary bypass.
Results: The immediate postoperative course was simple.
Conclusion: Brucella endocarditis is an uncommon, but serious complication of brucellosis. The tricuspid valve is rarely affected cardiac valve. Due to characteristics of the infection, medical therapy alone is not sufficient in treating the disease and best results are obtained with surgery combination. We describe a case of Brucella endocarditis involving the tricuspid valve suspected in front of the clinical data and the results of serology, confirmed by the culture of the native valves. In association with the medical treatment, management valve surgery lead to a favourable medium-term evolution.
Keywords: Brucella endocarditis; Tricuspid; Cardiopulmonary bypass
Introduction
Brucellosis is a multi-systemic zoonotic infection which is common in the Middle East, Central Asia, the Mediterranean basin and Central America [1,2]. Although brucella endocarditis is an uncommon complication, it remains the main cause of brucellosis-related mortality. Brucella tricuspid endocarditis is very rare [3]. Brucellosis affects more than 500,000 people worldwide each year [3,4]. It is the most frequent zoonosis. Brucella infection may involve any organ or tissue in the body. Organ involvement can be assigned as focal or complication. Endocarditis is the most common presentation of cardiovascular involvement, which is reported in less than 2% of patients with brucellosis. The diagnostic is made by serology and echocardiography (TTE). [5,6] Currently with medical treatment and the progress of cardiac surgery prognosis is favorable and the healing is possible [7]. This new report case is an opportunity for us to make a reminder of this little-known entity among cardiologists and heart surgeon who was successfully treated by medical and surgical therapy.
Methods
We report the case of 15-year-old children who present persist fever and dyspnea. His past medical history was positive for an episode of treated brucellosis.
The Physical examination: He complained of fever, malaise, arthralgia, anorexia and weight loss. The physical examination showed a found systolic murmur. with tachycardy and altered general status, skin pallor.
Chest X-ray: Showed mild cardiomegaly with blunting of right costophrenic angle and pulmonary parenchymal infiltration.
Electrocardiogramme: Showed a sinus tachycardia.
Echocardiography: Demonstrated vegetations (Figures 1,2) in chordate, papillary muscle, infundibulum, and right pulmonary artery with tricuspid insufficiency III grade and dysfunction systolic left ventricle function: Ejection fracytion: 46% with severy tricuspid regurgitation;
-SAPP: 50 mm hg.
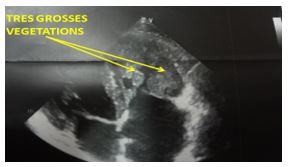
Figure 1: Echocardiography showing very large and oscillating tricuspid vegetations.
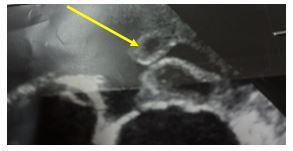
Figure 2: Echocardiography showing very large and oscillating tricuspid vegetations.
Angiochest CT: Showed proximal emboli of right pulmonary artery.
Biology
• Laboratory blood tests showed erythrocyte sedimentation rate 64 mm/h, C-reactive protein: 61 mg/mL, hemoglobin: 96 g/L, serum iron levels 3.4 mmol/L, platelets: 77 - 109/L, and serum creatinine: 110 mmol/L.
• Blood culture : Positives Brucella melitensis.
• Serology: Positive.
Surgery: The patient was opened under cardiopulmonary bypass by sternotomy approach. The per operative exploration showed multiples vegetations in tricuspid valve, right atrium, right ventricle, right pulmonary artery and mycotic aneurysm of the tricuspid ring (Figures 3-9). The gesture was excision of tricuspid and pulmonary vegetations and tricuspid repair with pericardial patch under cardiopulmonary bypass (Figures 10-12).

Figure 3: Opening view showing very large tricuspid vegetations.

Figure 4: Opening view showing very large tricuspid vegetations.
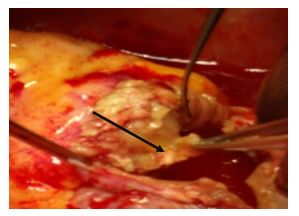
Figure 5: Opening view showing a debridement and excision of the infected tissue.

Figure 6: Opening view showing a debridement and excision of the infected tissue.
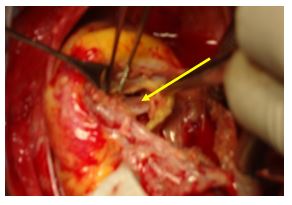
Figure 7: Opening view showing a debridement and excision of the infected tissue.
Figure 8: Opening view showing a debridement of the ventricular side of the tricuspid valve.

Figure 9: Opening view showing detachment of the anterior valve.
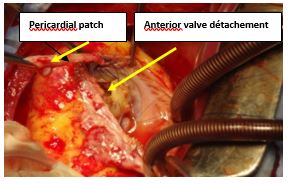
Figure 10: Opening view showing tricuspid repair with pericardial patch.
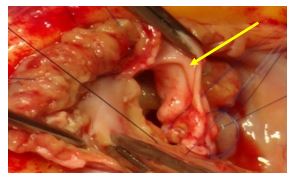
Figure 11: Opening view showing tricuspid repair with pericardial patch.
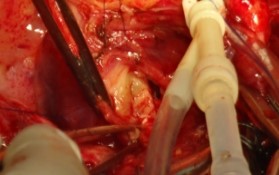
Figure 12: Opening view showing tricuspid repair with pericardial patch.
Results
• Aortic clamping: 72mn, duration of CPB: 90mn.
• The immediate postoperative course was simple.
• Stay in intensive care unit: 48 hours.
• Intubation procedure: 16 hours.
• Post-operative stay: 7 days.
• Ejection fraction: 65%.
Histopathologic examination: revealed the signs of infective endocarditis, and cultures from the valve were positive. Antibiotic treatment was continued four weeks after the operation with three antibiotics.
He was treated with doxycycline 200 mg/day PO, plus ciprofloxacin and gentamicin 5 mg/kg/day intramuscularly for 14 days. Subsequently he received the same dose of doxycycline for several additional months. After 4 weeks of antibiotic and symptomatic therapy, the patient’s condition was significantly improved, he was not febrile any more, and the laboratory tests were much better and normal echocardiography (Figures 13-15). In June 2016, 18 months after the operation, the patient felt well, completely recovered and without any signs of infection.
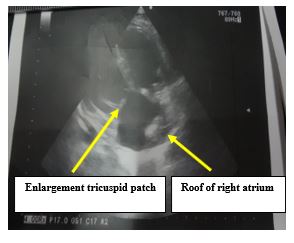
Figure 13: Postoperative echocardiography.

Figure 14: Postoperative echocardiography 01st day.

Figure 15: Postoperative echocardiography 10th day showing EF: 46%, SAPP: 32mm hg and tricuspid regurgitation I-II.
Comments
Our patient had a unique presentation namely Brucella tricuspid. Brucellosis is a systemic disease mainly affecting the musculoskeletal system (01). Cardiovascular complications, including endocarditis, are rare but usually fatal. The tricuspid valve is rarely involved (02). This includes both the native and prosthetic valves. Overall, early diagnosis and prompt medical and surgical interventions are essential for patients' survival since endocarditis continues to be the principal cause of mortality in the course of the disease. The diagnosis of brucellosis was based on combination of epidemiological, clinical data and positive serologic reactions [3,4]. Echocardiography and color Doppler mapping have become the most popular non-invasive, cost effective and easy-to-do procedure of choice for detection of the complications associated. These include: vegetation, tricuspid insuffiency, pulmonary embolism. The treatment of human brucellosis continues to pose a problem [5-7]. The best therapeutic approach to Brucella endocarditis involves a combination of medical and surgical treatment [4-7]. It is reported in literature that only these two treatments together successfully eradicate infection as Brucella can produce very destructive lesions when it is nested in the valvular endocardium. Antibiotic treatment alone is considered ineffective by most authors although there are sporadic cases successfully treated with only medical therapy (05). This is attributed to the intracellular localization of Brucella, the site that is relatively inaccessible to antibiotics. Even if symptoms improved and subsided with antibiotics, surgery would be still necessary because of the embolic potential of residual vegetation or to relieve valvular obstruction. Literature has reported confronting theories regarding the proper timing of surgical procedure of the affected valve in patients with diagnosed Brucella endocarditis [5-6]. Although some authors implicate the necessity of surgical treatment as early as possible even during the antimicrobial therapy, others suggest that it is better to postpone the surgical valve replacement after the antimicrobial treatment. The duration of antimicrobial therapy after valve replacement remains a bit disputable. Treatment periods that have been reported by different authors vary from 2-13 months [3-5]. The decision to discontinue antimicrobial therapy could be determined on patient-to-patient basis, after a thorough clinical observation and evidence of negative Ig A antibodies, normal CRP, and reduction of Wright seroreaction titers below 1/64. A patient also must be symptom-free. In our case, the patient was administered 01 year-postoperative antimicrobial treatment in order to eradicate Brucella. Justification for such postulation was confirmed in our case where patient was Brucella- free, symptom-free and without cardiac complication safter 30 months of a follow-up period.
Conclusion
Brucella endocarditis is an uncommon, but serious complication of brucellosis. The tricuspid valve is rarely affected cardiac valve. Due to characteristics of the infection, medical therapy alone is not sufficient in treating the disease and best results are obtained with surgery combination. We describe a case of Brucella endocarditis involving the tricuspid valve suspected in front of the clinical data and the results of serology, confirmed by the culture of the native valves. In association with the medical treatment, management valve surgery leads to a favorable medium-term evolution.
References
1. CLERC JL, ZECH F, THYS JP. 1990. Brucella endocarditis: the role of combined medical and surgical treatment. Rev Infect Dis. 12: 740-744. Ref.: https://www.ncbi.nlm.nih.gov/pubmed/2237111
2. LEDRU S, PAULET M, PAILLARD A, et al. Endocardite Brucella melitensis. 1992. 22: 500-I. Ref.: https://bit.ly/2vzJ11d
3. Endocardite brucellienne par un accident vasculaire cerebral Rev Mtd Interne. 2003. 24 Suppl 1.
4. Pappas G, Akritidis N, Bosilkovski M, et al. 2005. 352 : 2325-2326. Ref.: https://bit.ly/2PI3OGT
5. Shiono M, Hata M, Sezai A, et al. réopération pour anévrisme de l' aorte ascendante, coronaire ostiale anévrisme et CABROL de brevet tour après une opération de Bentall pour aortite syndrome. J. Circ 2005; 69: 861-864.
6. al-Kasab S, al-Faqih MR, al-Yousef S, et al. 1988. Brucella endocardite infectieuse. La thérapie combinée avec succès médical et chirurgical. J Thorac Cardiovasc Surg. 95 : 862-867.
7. Dhand A, Ross JJ. 2007. Implantable infection défibrillateur due à Brucella melitensis: rapport de cas et revue de la brucellose des dispositifs cardiaques . Clin Infect Dis. 44 : 37-39.




















