Indexing & Abstracting
Full Text
Research ArticleDOI Number : 10.36811/jcshd.2019.110014Article Views : 18Article Downloads : 39
Right Ventricle Recovery after ST Segment Elevation Myocardial Infarction Treated by Primary PCI as Assessed by 2D Speckle Tracking Echocardiography
Walid Sallam, MD, AmalM.Ayoub, MD, Mona I. AboulSoud, MD, Mohamed Ismail, MD, Mostafa A.Elnozahi, MD and Mohamed E. Zahran, MD*
Department of Cardiology, Faculty of Medicine, Ain Shams University, Cairo, Egypt
*Corresponding Author: Mohamed E. Zahran, MD, Department of Cardiology, Faculty of Medicine, Ain Shams University, Cairo, Egypt, Email: zahrancardiology@yahoo.com
DOI: 10.36811/jcshd.2019.110014
Article Information
Aritcle Type: Research Article
Citation: Walid Sallam, AmalM.Ayoub, Mona I. AboulSoud, et al. 2019. Right Ventricle Recovery after ST Segment Elevation Myocardial Infarction Treated by Primary PCI as Assessed by 2D Speckle Tracking Echocardiography. J Cardiovasc Surg Heart Dis. 1: 83-89.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2019; Walid Sallam
Publication history:
Received date: 25 October, 2019Accepted date: 07 November, 2019
Published date: 09 November, 2019
Abstract
Background: The right ventricle (RV) shows good long-term recovery in STEMI patients treated by primary PCI (PPCI), but, in the short term, RV involvement has a worse prognosis. Acute cardiogenic shock due to acute RV failure is equal in mortality to that due to acute left ventricular failure. The assessment of RV structure and function by echocardiography improved by advances including tissue doppler, strain, and three-dimensional (3D) imaging techniques.
Methods: In PPCI treated patients, the early recovery of the RV was studied using 2D speckle tracking Echocardiography.
Results: The study enrolled 120 patients, 40 anterior STEMI patients, 40 inferior STEMI patients and 40 adult healthy controls. All patients presented to Ainshams University hospitals cath. lab for PPCI as per guidelines. We excluded patients with known history of any disease affecting the RV. 102 males (85%) and 18 females (15%) were studied. The mean age of the anterior group was (53 ± 9 years) and of the inferior group was (54 ± 10 years). Full transthoracic echocardiography (TTE) examination including assessment of the RV systolic function by fractional area change (FAC), tricuspid annulus plane systolic excursion (TAPSE), Systolic TV annular velocity (S’) and RV free wall longitudinal strain. All echocardiographic measures were repeated after 3-6 months. Nine patients died during the follow up period. 54 (67.5%) patients had an impaired left evntricular ejection fraction (LVEEF) in the baseline study which significantly improved in the follow up (39.4%), (p value 0.001). A significant deterioration of the diastolic function was detected, (p value 0.002). A significant reduction of the Left atrial volume index (LAVI) was detected (p value 0.006). Also, a significant improvement of the RV FAC (p value 0.01) and TAPSE (p value 0.047). There was a significant deterioration of the apical RV free wall strain (P value 0.018).
Conclusions: Right ventricular systolic function may be normal after acute STEMI treated by PPCI, but with 2D strain echocardiography, subclinical RV systolic dysfunction can be detected. So, it’s recommended to assess the global & segmental RV functions after acute MI with the conventional parameters as well as by 2D speckle tracking derived strain.
Keywords: Acute MI; TTE; FAC; TAPSE S’; RV free wall GLS
Introduction
Right Ventricular dysfunction has been associated with high morbidity and mortality in patients with variable heart diseases [1,2]. The assessment of right ventricular (RV) structure and function by echocardiography improved by advances including Tissue doppler, strain, and three-dimensional (3D) imaging techniques [3]. Conventional determination of RV function by 2-dimensional (2D) is often qualitative. Doppler methods of tricuspid inflow and pulmonary artery flow velocities are influenced by changes in preload and afterload thus, may not provide accurate information for clinical decision making. Tissue doppler and strain imaging are useful in the assessment of regional RV systolic and diastolic functions. Recent advances in echocardiographic imaging of the right ventricle include Doppler tissue imaging (DTI), strain imaging (SI), and volumetric 3-dimensional (3D) imaging, which can be used for additional information beyond standard 2D measurements [4]. The RV shows good longterm recovery after acute MI but, in the short term, RV involvement has a worse prognosis. Acute RV shock has an equally high mortality to left ventricular (LV) shock [5]. This study was conducted to detect RV dysfunction after acute MI.
Methods
The study was conducted in the period from September 2014 to May 2016 including 120 individuals who were recruited from Ain Shams University hospital. Eighty patients were from the Coronary Care Unit (CCU) presenting with acute ST elevation myocardial infarction & the other 40 patients were recruited from the outpatient clinic as control cases. We excluded any patient with previously diagnosed diseases affecting the right ventricular function, previous MI, PCI or CABG. All patients were subjected to thorough history taking with particular stress on age, cardiovascular risk factors, pain to door & door to balloon time. Then full clinical examination was done stressing on the signs of RV failure e.g. congested neck veins & LL oedema. All the patients underwent successful reperfusion by primary PCI as per guidelines recommendations [5]. Twelve-lead surface ECG, and standard trans-thoracic twodimensional echocardiography including LV EF by Simpson’s method, LV & RV Diastolic function, RV systolic function assessment by measurement of RV FAC, TAPSE, S’ and RV free wall global longitudinal strain. All these measures were repeated after 3-6 months. The study was done after approval of ethical board of Ain Shams University and an informed written consent was taken from each participant in the study.
Statistical Analysis
Data were collected, revised, coded and entered to the Statistical Package for Social Science (IBM SPSS). Qualitative data were presented as number and percentages while quantitative data were presented as mean, standard deviations and ranges. The comparison between two groups with qualitative data was done by using Chi-square test and/or Fisher exact test (used instead of Chisquare test when the expected count in any cell was found less than 5). The comparison between two independent groups of quantitative data with parametric distribution was done by using Independent t-test. Spearman correlation coefficients were used to assess the relation between two quantitative parameters in the same group. The confidence interval was set to 95% and the margin of error accepted was set to 5%. So, the p-value was considered significant as the following: P>0.05: Non significant, P<0.05: Significant and P<0.001: Highly significant.
Results
The study enrolled 120 patients, 40 control, 40 patients presented with anterior STEMI & 40 patients presented with inferior STEMI patients. Nine patients died during the follow up, so they were excluded from the follow up. 18 (15%) females & 102 (85%) males were studied. In the anterior group, 7 (17.5%) females & 33 (82.5%) males & in the inferior group 5 (12.5%) & 35 (87.5%) were included. The mean age of the anterior group was 53 ± 9 years & inferior group was 54 ± 10 years. Twenty-eight patients (70%) in the anterior group were smokers and also 28 patients (70%) in the inferior group were smokers. Six patients (15%) were ex-smokers in the anterior & 3 patients (7.5%) in the inferior group. Twenty patients in the anterior group were diabetic (50%) and 16 in the inferior group (40%). Thirty two patients were hypertensive: 15 (37.5%) in the anterior & 17 (42.5%) in the inferior group. Dyslipidemia was detected in 26 patients (65%) in Anterior Group and 29 patients (72.5%) in Inferior group. Positive family history of premature coronary artery disease was found in 4 patients (10%) in the anterior group and 9 patients (22.5%) in the inferior group.
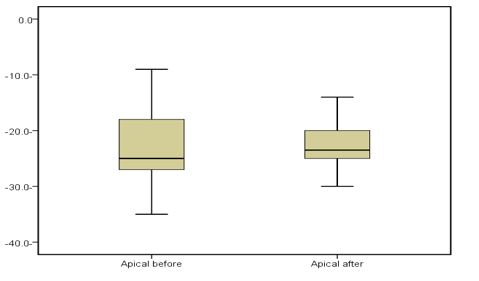
In the Anterior Group: The systolic and diastolic blood pressure ranged from 90 to 180 mmHg and from 60 to 100 mmHg respectively with mean and SD of 127.13±22.47 and 79.75±11.71 respectively. The heart rates ranged from 50 to 120 bpm with mean and SD of 87.25±15.61. The neck veins were congested in 13 patients (32.5%). The Pain to Door (PTD) time ranged from 0.5 to 13 hours with median 4 hours & the Door to Balloon (DTB) time ranged from 0.25 to 3 hours with mean & standard deviation 0.93±0.54.In the Inferior Group: The systolic and diastolic blood pressure ranged from 90 to 160 mmHg and from 60 to 100 mmHg respectively with mean and SD of 111.75±16.78 and 71±7.78 respectively. The heart rates ranged from 40 to 100 bpm with mean and SD of 74.45±11.73. The neck veins were congested in 13 patients (32.5%). The Pain to Door (PTD) time ranged from 0.5 to 36 hours with median 3 hours & the Door to Balloon (DTB) time ranged from 0.5 to 2 hours with mean & standard deviation 0.93±0.54.The systolic & diastolic blood pressures as well as the heart rate showed high statistically significant difference in the anterior group and the inferior group with P-value 0.001, 0.000 & 0.000 respectively. 54 (67.5%) patients had an impaired EF in the baseline study which significantly improved in the follow up (39.4%). P value 0. 001.A highly significant deterioration of the diastolic function was detected (P value 0.002). A highly significant reduction of the LAVI was detected (P value 0.006). Also, a significant improvement of the RV FAC & TAPSE.There was a significant deterioration of the apical RV free wall strain (P value 0.018).
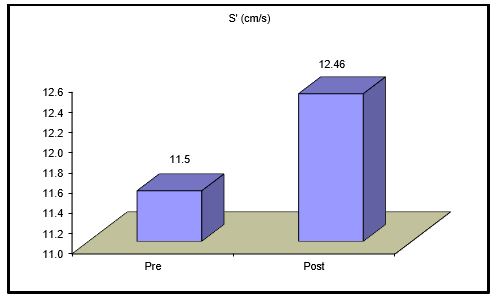
Comparison between the mean S’ in the inferior group in the baseline (Pre) & follow up (Post) echocardiographic examination.
|
|
All patients |
Test value |
P-value |
Sig. |
||
|
Baseline |
Follow-up |
|||||
|
EF |
Normal |
26 (32.5%) |
43 (60.6%) |
11.938* |
0.001 |
HS |
|
Impaired |
54 (67.5%) |
28 (39.4%) |
||||
|
LV diastolic dysfunction |
No |
24 (30.0%) |
5 (7.0%) |
14.36* |
0.002 |
HS |
|
I |
50 (62.5%) |
62 (87.3%) |
||||
|
II |
5 (6.2%) |
4 (5.6%) |
||||
|
III |
1 (1.2%) |
0 (0.0%) |
||||
|
TV inflow |
No |
49 (61.2%) |
54 (76.1%) |
4.317* |
0.115 |
NS |
|
Reversed |
30 (37.5%) |
17 (23.9%) |
||||
|
Pseudonormal |
1 (1.2%) |
0 (0.0%) |
||||
|
LA volume index |
Normal |
68 (85.0%) |
67 (94.4%) |
10.174* |
0.006 |
HS |
|
Increased |
12 (15%) |
4 (5.6%) |
||||
|
RV FAC |
Normal |
63 (78.8%) |
69 (97.2%) |
11.62* |
0.001 |
HS |
|
Decreased |
17 (21.2%) |
2 (2.8%) |
||||
|
TAPSE |
Normal |
71 (88.8%) |
69 (97.2%) |
3.961* |
0.047 |
S |
|
Reduced |
9 (11.2%) |
2 (2.8%) |
||||
|
S' |
Normal |
71 (88.8%) |
67 (94.4%) |
1.508* |
0.219 |
NS |
|
Reduced |
9 (11.2%) |
4 (5.6%) |
||||
|
Apical |
Median (IQR) |
-24.5 (-29 – -16) |
-24 (-26 – -19) |
-2.365? |
0.018 |
S |
|
Range |
-43 – 12 |
-33 – 10 |
||||
|
Mid |
Median (IQR) |
-25 (-29 – -15.5) |
-23 (-28 – -20) |
-1.350? |
0.177 |
NS |
|
Range |
-43 – -6 |
-32 – -6 |
||||
|
Basal |
Median (IQR) |
-23 (-29 – -16.5) |
-24 (-30 – -18) |
-0.050? |
0.960 |
NS |
|
Range |
-42 – 3 |
-35 – 4 |
||||
|
Global |
Median (IQR) |
-24 (-29 – -15) |
-23 (-28 – -20) |
-1.202? |
0.229 |
NS |
|
Range |
-42 – -8 |
-32 – -4 |
||||
|
RVSP (mmHg) |
Normal |
77 (96.2%) |
65 (91.5%) |
1.483* |
0.223 |
NS |
|
Elevated |
3 (3.8%) |
6 (8.5%) |
||||
Discussion
The purpose of the current study was to assess the RV systolic functions after successful reperfusion of patients presented with acute STEMI: early within 48 hours & follow up after 3-6 months. Assessment was done using conventional echocardiographic methods of RV assessment & the novel technique, strain imaging derived by 2D-speckle tracking echocardiography. Our study included 120 individuals divided into three groups: 40 patients presented with inferior STEMI, 40 patients presented with anterior STEMI & 40 control individuals, age & sex matched with the previous two groups. Nine patients died during follow-up and therefore did not have the follow-up. In the baseline echocardiographic study: the mean EF in the was 49.13 ± 10.43%, the mean LAVI was 28.26 ± 5.82 ml/m2, the mean RV FAC was 43.95 ± 9.72, the mean TAPSE was 18.84 ± 3.24 mm, the mean S’ was 12.34 ± 2.35 cm/s & the median global longitudinal strain (GLS) of the RV fee wall was -24 (IQR -29 - -15).The longitudinal strain of the apical segment of the RV free wall in the anterior group was found to have a high statistically significant impairment in comparison to the control group (P=0.001) although all conventional methods failed to detect significant impairment of the RV functions in most of the patients which is concordant with a previous study as well [6].
In a previous study [7]. 95 patients with acute STEMI (48 with inferior & 47 with anterior STEMI) were enrolled & primary PCI was the reperfusion strategy. Right ECG leads ST segment elevation was present in 12 patients (12.6%) & this was concordant with our study. Echocardiography was done 24 hours after reperfusion & at 6 months follow up. The mean RV free wall GLS was -25.6 ± 6.1 which discordantly better than the GLS of our patients. Comparing the anterior group of Huttin et al [7]. with the anterior group in our study at baseline echocardiography, the mean EF was 47.7 ± 8.8%, RV FAC was 45.2 ± 8.9%, TAPSE was 21.8 ± 5.2 mm & S’ was 12.6 ± 2.7 cm/s. All these parameters are concordant with our study in the anterior group. The mean RV free wall GLS was -28.2 ± 5.5 which is discordantly better than that of our study in the anterior group (-25.5).
As regard the inferior group of Huttin et al [7]. At baseline study, the mean EF was 51.7 ± 8.7%, RVFAC was 37.5 ± 10.2 mm, S’ was 12.7 ± 2.4 cm/s & the RV free wall GLS was -22.6 ± 6.0. These results were concordant with our study in the inferior group. The mean TAPSE was 22.0 ± 4.8 mm which is discordantly higher than the TAPSE in our study in the inferior group (17.95 ± 3.13).The follow up echocardiography of our study in the anterior group in comparison to their baseline study revealed highly significant improvement of the EF, non-significant change in the RV conventional parameters & in the RV free wall GLS, but in comparison to the control group, a highly significantimpairment of the apical, mid & global longitudinal strain was surprisingly detected. The improvement in EF & non-significant change in other conventional parameters & GLS of the RV were concordant with Huttin et al except for the TAPSE which significantly improved among his anterior MI group discordant with our study which revealed no significant change.
Conclusion
Right ventricular systolic function may be normal after acute STEMI, but with 2D strain echocardiography, subclinical RV systolic dysfunction can be detected. So, it’s recommended to assess the global & segmental RV functions after acute MI with the conventional parameters & by global longitudinal strain.
Limitations
The gold standard for assessment of the RV function is the MRI, but it wasn’t feasible to be used in our study due to technical & cost issues.
References
1. Antoni ML, Scherptong RW, Atary JZ, et al. 2010. Prognostic value of right ventricular function in patients after acute myocardial infarction treated with primary percutaneous coronary intervention. 3: 264-271. Ref.: https://bit.ly/2qj0lVw
2. Matthews JC, Dardas TF, Dorsch MP, et al. 2008. Right-sided heart failure: diagnosis and treatment strategies. 10: 329-341. Ref.: https://bit.ly/2CfGqt2
3. Hutyra M, Skála T, Horák D, et al. 2015. Echocardiographic assessment of global longitudinal right ventricular function in patients with an acute inferior ST elevation myocardial infarction and proximal right coronary artery occlusion. 31: 497-507. Ref.: https://bit.ly/33iu9Aa
4. Horton KD, Meece RW, Hill JC. 2009. Assessment of the Right Ventricle by Echocardiography: A Primer for Cardiac Sonographers. 22: 776-792. Ref.: https://bit.ly/34wzJ1X
5. Bax JJ, Baumgartner H, Ceconi C, et al. 2012. ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). 33: 2569-2619. Ref.: https://bit.ly/34suRej
6. Kakouros N, Cokkinos DV. 2010. Right ventricular myocardial infarction: pathophysiology, diagnosis, and management. 86: 719-728. Ref.: https://bit.ly/2NCyWWq
7. Huttin O, Lemarié JDi, Meglio M, et al. 2015. Assessment of right ventricular functional recovery after acute myocardial infarction by 2D speckle-tracking echocardiography. Int J Cardiovasc Imaging. 31: 537-545. Ref.: https://bit.ly/33hiW2T




















