Indexing & Abstracting
Full Text
Case ReportDOI Number : 10.36811/jcri.2022.110032Article Views : 0Article Downloads : 1
Tricuspid endocarditis on electrical stimulation probes complicated by septic shock: A case report
Redha Lakehal*, Soumaya Bendjaballah, Baya aziza, Abdelrahman Babouri and Abdelmalek Bouzid
Department of Heart Surgery, Ehs Dr Djaghri Mokhtar, Constantine, Algeria
*Corresponding Author: Redha Lakehal, Department of Heart Surgery, Ehs Dr Djaghri Mokhtar, Constantine, Algeria; Email: lakehal.redha@gmail.com
Article Information
Aritcle Type: Case Report
Citation: Redha Lakehal, Soumaya Bendjaballah, Baya aziza, et al. 2022. Tricuspid endocarditis on electrical stimulation probes complicated by septic shock: A case report. J Case Rept Img. 4: 20-25.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2022; Redha Lakehal
Publication history:
Received date: 05 April, 2022Accepted date: 19 April, 2022
Published date: 26 April, 2022
Abstract
Introduction: The infection of pacemakers seriously compromises the prognosis of patients carrying these foreign materials. It most often affects the intracardiac probes, but also the valves, in nearly half of the cases. It concerns 1% of patients. The average age is over 60; fever, prolonged or intermittent, is present in 90% of patients; signs of infection of the box compartment are reported in 45% of cases; pulmonary manifestations are noted in 20-40% of cases. Adenoids are detected in 90% of cases in echocardiography. Staphylococci are responsible for 80% of infections. Antibiotic treatment comprising a bactericidal dual therapy implemented after bacteriological samples within a period that takes into account the mode of presentation of the infection, the terrain and the degree of certainty of the diagnosis. All equipment should be removed systematically whenever possible. Antibiotic prophylaxis is recommended at the time of placement of the endovascular material, and probably also during each manipulation. The aim of this work is to report a case of tricuspid endocarditis on stimulation probe complicated by septic shock.
Methods: We report the observation of a 32-year-old patient with a history of complete AVB fitted for 6 years transferred from the intensive care unit after stabilization of septic shock secondary to tricuspid infective endocarditis. Echocardiography: Dilatation of the right cavities, leakage massive tricuspid, images of vegetations in a string on stimulation probes, EF: 50% with relaxation disorder, SAPP: 55 mm Hg, dry pericardium and right pleural effusion. Thoracic CT angiography: No signs of pulmonary embolism left postero-basal pneumopathy, moderately abundant right pleural effusion with adjacent atelectasis. Operative exploration: Presence of two stimulation probes: one right auricular, the other right ventricular bearer of multiple vegetation in a string. The gesture: Removal of the two probes carrying with it the vegetations sent to bacteriology under assistance then tricuspid plasty and verification of the trunk of the pulmonary artery and its two branches, which are free after aortic clamping, and finally removal of the case sent to the bacteriology.
Results: The postoperative follow-up was simple.
Conclusion: Serious affection. Diagnosis and treatment require multidisciplinary care. Strict compliance with antibiotic prophylaxis during pacemaker’s placement should reduce the incidence of this infection, whose morbidity and mortality are high.
Keywords: Tricuspid Endocarditis; Stimulation Probe; Septic Shock; Vegetation; CPB
Introduction
The infection of pacemakers seriously compromises the prognosis of patients carrying these foreign materials. It most often affects the intracardiac probes, but also the valves, in nearly half of the cases. It concerns 1% of patients. Fever, prolonged or intermittent, is present in 90% of patients; signs of infection of the box compartment are reported in 45% of cases; pulmonary manifestations are noted in 20-40% of cases. Vegetations are detected in 90% of cases in echocardiography. Staphylococci are responsible for 80% of infections. The antibiotic treatment comprising a bactericidal dual therapy is implemented after bacteriological samples within a period that takes into account the mode of presentation of the infection, the terrain and the degree of certainty of the diagnosis. All hardware should be removed systematically whenever possible. Antibiotic prophylaxis is recommended at the time of placement of the endocavitary material and probably also during each manipulation. The aim of this work is to report a case of tricuspid endocarditis on stimulation probes complicated by septic shock.
Observation
We report the case of a 32-year-old patient with a history of complete atrioventricular block (AVB) fitted for 6 years transferred from the intensive care unit after stabilization of septic shock secondary to tricuspid infective endocarditis under Dobutrex and Noradrenaline with double probabilistic antibiotic therapy. Functionally, the patient was intubated ventilated with altered general condition. Echocardiography showed dilation of the right cavities, massive tricuspid leak, images of vegetations in a chain on stimulation probes, EF: 50% with relaxation disorders, SAPP: 55 mmHG, and right pleural effusion (Figures 1,2).

Figure 1: Echocardiographic image of vegetations on stimulation probes.

Figure 2: Echocardiographic image of the ventricular pacing lead.
Thoracic CT angiography showed no signs of pulmonary embolism, presence of left postero-basal pneumopathy, right pleural effusion of moderate abundance with atelectasis opposite. Biologically, CRP was 212 mg/l and blood cultures were negative. The patient underwent emergency surgery under cardiopulmonary bypass. Peroperative exploration found two stimulation probes: one right atrial, the other right ventricular carrying multiple vegetations in a string. The gesture had consisted of removal of the two probes carrying with it the vegetations sent to the bacteriology under assistance (Figures 3,4) then tricuspid plasty type De Vega and verification of the trunk of the pulmonary artery and its two branches which were free after clamping aortic and finally removal of the box sent to bacteriology.
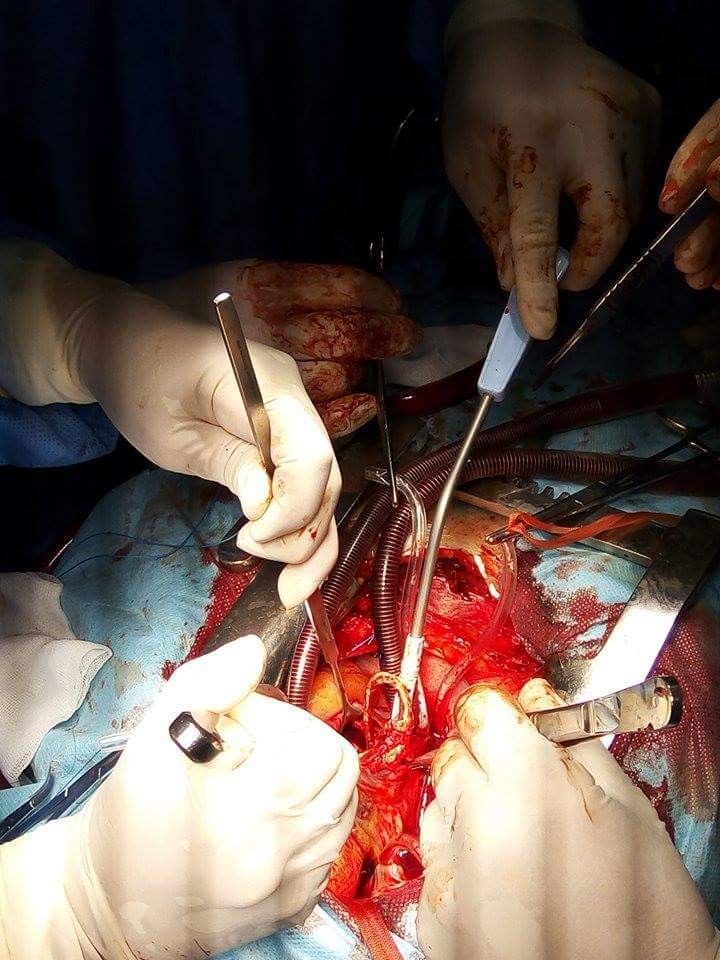
Figure 3: Intraoperative image at the opening of the right atrium.

Figure 4: Intraoperative image after removal of the stimulation probes with the vegetations.
Results
The postoperative follow-up was simple. Culture of stimulation probes was negative. The durations of CPB, aortic clamping and circulatory support were 32, 14, 10 min respectively.
Discussions
Infection after pacemaker/defibrillator implantation is a potentially serious complication. Due to the increasing number of implanted devices, the incidence of this disease has increased in parallel [1,5]. Cardiac pacemakers and implantable automatic defibrillators include probes connected to the box to deliver the necessary therapies (pacing and defibrillation) to the patient [2]. These probes are subject to many complications once implanted, some of which require their removal, such as infection on the probe (infective endocarditis on the probe) [2]. The microbiological diagnosis is based on the result of the cultures obtained at the site of the case, on the material itself and on the blood [1,4,6]. The negativity of the cultures of the stimulation probes of our patient is explained by the probabilistic antibiotic therapy before the surgical ablation. Coagulase-negative Staphylococci, and mainly Staphylococcus epidermidis, are responsible for most late infections (75%) on stimulation probes [3]. Diagnosis is based on transesophageal ultrasound, transthoracic ultrasound being less sensitive [1,4,6] as in our patient where this examination showed chaplet vegetations on the stimulation probes.
Cardiological management includes two steps associated with anti-infective treatment: extraction of all infected material with new implantation of a pacemaker [3,4,6] as is the case with our patient. Management is difficult for several reasons: difficulties in eradicating microorganisms from foreign material by antibiotic therapy alone, high embolic risk of vegetations, spontaneous or during ablation, vital necessity in some cases of an electric drive permanent heart failure, risk of open hear tsurgery in these patients, most often elderly [3,7,8]. Therapeutic choices must take into account the early or late nature of the infection, the microorganism and its sensitivity to antibiotics, the existence of associated valvular damage and remote infectious foci (pulmonary emboli, etc.), initial indications for pacemaker placement, vegetation size and terrain (possibility of cardiopulmonary bypass) [3,7,8]. The mortality of endocarditis on stimulation probes varied between 10 and 30% [9].
Conclusion
Serious affection. Diagnosis and treatment require multidisciplinary care. Strict compliance with antibiotic prophylaxis during the insertion of pacemakers should reduce the incidence of this infection, the morbidity and mortality of which are high.
References
1. Camus C. 2008. Infections graves liées aux stimulateurs cardiaques et défibrillateurs implantables. © 2008 Société de réanimation de langue franc¸aise. Publié par Elsevier Masson SAS. Tous droits réservés.
2. Vladimir M. 2013. Extraction de sondes de pacemaker et de défibrillateur : expérience du CHU de Nancy entre 2000 et 2013. Sciences du Vivant.
3. Endocardite sur sonde de pacemaker. Pacemaker infective endocarditis. l’Infectiologue - Tome XVIII - n° 2 - marsavril 2003.
4. Chua JD, Wilkoff BL, Lee I. 2000. Diagnosis and management of infections involving implantable electrophysiologic cardiac devices. Ann Intern Med. 133: 604-608. Ref.: https://pubmed.ncbi.nlm.nih.gov/11033588/ DOI: https://doi.org/10.7326/0003-4819-133- 8-200010170-00011
5. Cabell CH, Heidenreich PA, Chu VH. 2004. Increasing rates of cardiac device infections among Medicare beneficiaries: 1990-1999. Am Heart J. 147: 582-586. Ref.: https://pubmed.ncbi.nlm.nih.gov/15077071/ DOI: https://doi.org/10.1016/j.ahj.2003.06.005
6. Sohail MR, Uslan DZ, Khan AH. 2007. Management and outcome of permanent pacemaker and implantable cardioverterdefibrillator infections. J Am Coll Cardiol. 49: 1851-1859. Ref.: https://pubmed.ncbi.nlm.nih.gov/17481444/ Ref.: https://doi.org/10.1016/j.jacc.2007.01.072
7. Leprince P, Nataf P, Cacoub P. 1995. Septicemia and endocarditis related to transvenous pacing leads of pacemakers: surgical indications and results. Arch Mal Coeur. 88: 241-246. Ref.: https://pubmed.ncbi.nlm.nih.gov/7487273/
8. Carbon C, Cartier F, Etienne J. 1992. Endocardites infectieuses de l'adulte ; propositions pour l'antibiothérapie curative. Med Mal Infect. 22: 370.
9. Meune C, Arnal C, Hermand C. 2000. Les endocardites infectieuses sur sondes de pacemaker [Infective endocarditis related to pacemaker leads. A review]. Ann Med Interne (Paris). 151: 456-464.




















