Indexing & Abstracting
Full Text
Case ReportDOI Number : 10.36811/jcri.2022.110030Article Views : 0Article Downloads : 2
Surgery of a giant aneurysm of the ascending aorta, the aortic arch and the initial part of the descending aorta: A case report
Redha Lakehal*, Soumaya Bendjaballah, Baya aziza, Abdelrahman Babouri and Abdelmalek Bouzid
Department of Heart Surgery, Ehs Dr Djaghri Mokhtar, Constantine, Algeria
*Corresponding Author: Redha Lakehal, Department of Heart Surgery, Ehs Dr Djaghri Mokhtar, Constantine, Algeria; Email: lakehal.redha@gmail.com
Article Information
Aritcle Type: Case Report
Citation: Redha Lakehal, Soumaya Bendjaballah, Baya aziza, et al. 2022. Surgery of a giant aneurysm of the ascending aorta, the aortic arch and the initial part of the descending aorta: A case report. J Case Rept Img. 4: 11-16.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2022; Redha Lakehal
Publication history:
Received date: 05 April, 2022Accepted date: 19 April, 2022
Published date: 26 April, 2022
Abstract
Introduction: The replacement of the aortic arch must simultaneously address two main categories of action: the method of replacing the aorta itself and its essential branches, which are the vessels of the neck, but also the protection of the aorta. Brain during the time of exclusion from cerebral circulation. The aim of our work is to report a case of aneurysm of the ascending aorta of the arch and the initial part of the descending aorta.
Methods: We report the case of a 77-year-old patient with a history of chronic obstructive pulmonary disease and gastritis admitted for surgical treatment of an ascending aortic aneurysm encompassing the entire aortic arch and the initial part of the descending aorta. Physical examination: left supraclavicular-swelling. ECG: Regular sinus rhythm. Chest x-ray: 10 cm enlargement of the mediastinum. Echocardiography: aortic aneurysm dissecting semi-thrombosis beyond the Valsalva sinus to the 112 mm aortic arch, slightly compressing the right cavities. EF: 67%; LV: 64.7/40.3mm; SAPP: 21mmhg and no associated valve disease. Chest angioscan: large aneurysm measuring 13 cm partially thrombosed with a circulating channel measuring 09 cm from the ascending aorta extended to the arch. Intraoperative exploration: large aneurysm of the ascending aorta of the aortic arch and of the initial part of the descending aorta. Procedure: replacement of the ascending aorta of the arch and the initial part of the descending aorta with a Dacron prosthesis after resection of the pathological tissue and the thrombus with preparation of the distal anastomosis in circulatory arrest and reimplantation of supraaortic trunks.
Results: Discharge from CPB under vasoactive drugs, prolonged stay in intensive care with difficulty in extubating of patient.
Conclusion: Despite the progress of anesthesia, resuscitation, antegrade perfusion of the brain; surgery as well as myocardial protection, interventions on the arch remain complex and cumbersome. Hospital mortality is around 10%. It is multiplied by 5 in an emergency.
Keywords: Aortic arch; Aneurysm; Brain Protection; Hypothermia; Circulatory Arrest; Reimplantation of the neck vessels
Introduction
The replacement of the aortic arch must simultaneously focus on two main categories of action: the mode of replacement of the aorta itself and its essential branches, which are the vessels of the neck, but also the protection of the brain. During the time of exclusion from cerebral circulation. The aim of our work is to report a case of an aneurysm of the ascending aorta, the aortic arch and the initial part of the descending aorta treated surgically in moderate hypothermia with selective perfusion of the supraaortic trunks.
Observation
We report the case of a 77-year-old patient with chronic obstructive pulmonary disease (COPD) and a history of gastritis admitted for surgical treatment of an aneurysm of the ascending aorta encompassing the entire aortic arch and the initial part of the descending aorta. Physical examination showed left supraclavicular swelling. The ECG showed regular sinus rhythm and left ventricular hypertrophy. The chest X-ray showed an enlargement of the mediastinum by 10 cm (Figure 1).

Figure 1: Enlargement of the mediastinum on frontal chest X-ray.
Echocardiography revealed a semi-thrombosed dissecting aortic aneurysm beyond the sinus of Valsalva up to the aortic arch of 112 mm slightly compressing the right cavities. EF: 67%; LV: 64.7/40.3mm; SAPP: 21 mmHg and no associated valve disease. Thoracic CT angiography showed a large aneurysm measuring 13 cm in diameter, partially thrombosed with a circulating channel measuring 09 cm from the ascending aorta extended to the aortic arch and the initial part of the descending aorta (Figure 2).

Figure 2: Angioscannographic image of a large aneurysm of the ascending aorta and the aortic arch.
Intraoperative exploration showed a large aneurysm of the ascending aorta; of the aortic arch and the initial part of the descending aorta (Figure 03). The gesture consisted after installation of cardiopulmonary bypass (CPB) between the right femoral artery and the right atrium and establishment of moderate hypothermia at 24° C with circulatory arrest.
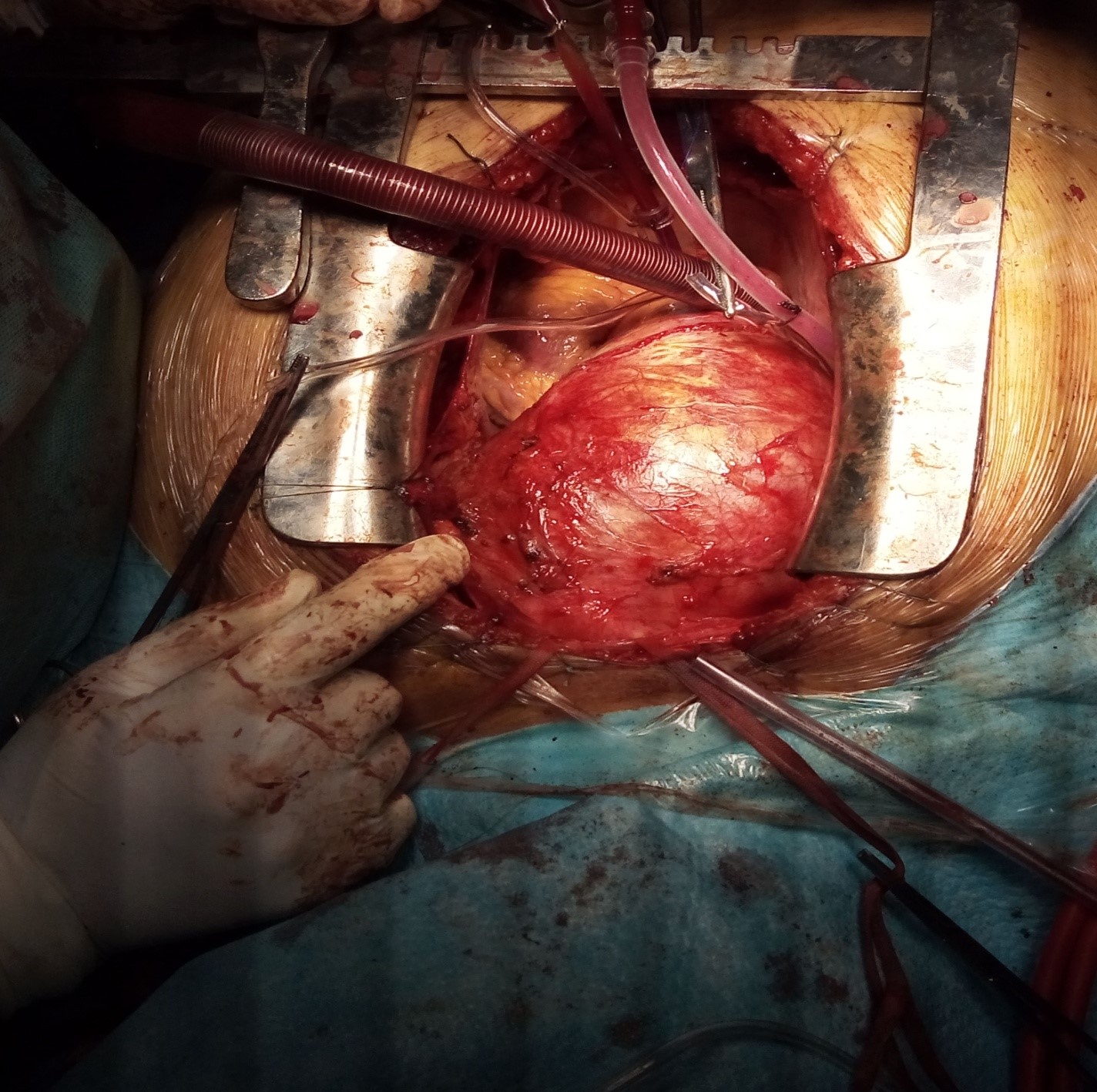
Figure 3: Intraoperative image with aneurysm of the ascending aortic aneurysm and the aortic arch.
• Selective cannulation of the brachiocephalic arterial trunk (BCAT) and left primary carotid artery (LPCA) according to the Kazui technique with placement of a Foley probe at the level of the left subclavian artery after opening of the aneurysm of the ascending aorta.
• Resection of the ascending aorta and the aortic arch sent for anatomopathological study with preservation of the aortic valve.
• Confection of the distal anastomosis in endoluminal between a first tube in Dacron N°30 and the descending aorta.
• Reimplantation of the supraaortic trunks (SAT) in a pallet at the level of the first Dacron tube.
• Clamping of the first dacron tube upstream of the BCAT after recovery of the CPB and purging of the SAT and this first dacron tube.
• Confection of the proximal anastomosis between the aorta and the second tube in dacron n°30 during the heating of the body.
• Confection of an anastomosis of the 02 prosthetic tubes in the end-to-end (Figure 4).

Figure 4: Intraoperative image final appearance after surgery.
Results
The durations of cardiopulmonary bypass, aortic clamping and circulatory support were 367, 85 and 111 min respectively. The CPB was in moderate hypothermia at 24° C with circulatory arrest lasting 105 min. The duration of mechanical ventilation was 60 days and the stay in the intensive care unit was 60 days. The immediate postoperative follow-up was favorable with complete awakening of the patient without any deficit then unfavorable linked to the complications of prolonged intubation secondary to the impossibility of extubation the patient with death on the 60th postoperative day following an oesotracheal fistula.
Discussion
An aneurysm can generally be defined as the enlargement of a blood vessel to more than 150% of the diameter expected for gender, age, and weight [4]. Although the true prevalence of thoracic aortic aneurysms is unknown, it is estimated to have an incidence of at least 5–10 per 100,000 person-years [5,7]. More than half of these aneurysms are in the ascending aorta followed in frequency by the descending thoracic aorta. Less than 10% are confined to the aortic arch [5]. Atherosclerosis along with its risk factors, connective tissue disease (eg, Marfan syndrome), and abnormalities of the aortic valve (eg, bicuspid aortic valve) are strongly associated with the development of ascending aortic aneurysms, but sporadic cases have also been reported [8-9].
The majority of thoracic aortic aneurysms are asymptomatic, and identifying a patient with them represents a true challenge to health care providers [4-5]. Thoracic aortic aneurysms are often silent [1-4]; the case of our patient was discovered during a radiological assessment motivated by the beating mass of the suprasternal hollow.
Frequently reported symptoms of thoracic aortic aneurysm include dyspnea, cough, dysphagia, hoarseness of voice, claudication, cerebrovascular events, as well as chest, abdominal, or back pain [9]. Other unusual presentations of thoracic aneurysms reported in the literature include erosion of the overlying skin and sternum, rupture into the esophagus, compression and invasion of the pulmonary artery, superior vena cava syndrome, and recurrent laryngeal and phrenic nerve palsy [10-13,14,15].
Their diagnosis usually follows a pathway in which a radiological study is being performed for a different reason, and the aneurysm is discovered coincidentally [5]. The etiology of aneurysmal formation is incompletely understood [6]. Most aortic aneurysms are caused by degenerative, infectious, or genetic conditions that weaken the aortic wall [6]. Symptomatic aortic aneurysms may manifest as chest pain, discomfort, a new cardiac murmur, or more drastically as heart failure, aortic dissection, or rupture [6]. It is estimated that 21% of patients suffering from acute aortic syndromes die before reaching the hospital [2]. To diagnose these aneurysms, the clinical history should be focused on the symptoms, risk factors, family history, and followed by detailed physical examination looking for signs of aneurysmal dilatation or its complications [9]. Aortic imaging with echocardiography, computed tomography angiography, and magnetic resonance angiography remain the cornerstone to diagnose aortic aneurysms [9]. Screening with transesophageal echocardiography is reasonable to evaluate the aorta in predisposed populations (eg, connective tissue disorders, bicuspid aortic valve, or screening first-degree relatives of patients with Thoracic aortic aneurysms).
CT or MRI confirms the diagnosis of aortic aneurysms [6]. Intervention by surgery is indicated when the size of the aneurysm reaches a threshold where the risk for developing complications according to the natural history of the disease is significant [6- 8].
The significant determinants for intervention are the size of the aneurysm, rate of expansion, and associated conditions [9]. Aneurysms are repaired when the risk of rupture exceeds the risk of repair [5]. Surgical replacement of part or all of the aortic arch requires temporary interruption of distal aortic perfusion. The combination of the three techniques: cardiopulmonary bypass, perfusion of the supra-aortic trunks and hypothermia, is currently the most reliable method. Prolonged intubation with the impossibility of extubating the patient due to age and COPD. Age, COPD, combined arch and ascending aorta surgery and the duration of ventilation are the predictive factors for mortality.
Conclusion
Thoracic aortic aneurysms are encountered frequently in the emergency department with an obscure presentation. Most of these aneurysms are incidentally discovered while doing routine imaging studies. Despite advances in anesthesia, resuscitation, anterograde brain perfusion; surgery as well as myocardial protection, interventions on the arch remain complex and cumbersome. Hospital mortality is around 10%. 5 multiply it in an emergency.
References
1. Clift PF, Cervi E. 2019. A review of thoracic aortic aneurysm disease. Echo Res Pract. 7: 1- 10. Ref.: https://pubmed.ncbi.nlm.nih.gov/32015897/ DOI: https://doi.org/10.1530/erp-19-0049
2. Saeyeldin AA, Velasquez CA, Mahmood SUB. 2019. Thoracic aortic aneurysm: unlocking the “silent killer” secrets. Gen Thorac Cardiovasc Surg. 67: 1-11. Ref.: https://pubmed.ncbi.nlm.nih.gov/29204794/ DOI: https://doi.org/10.1007/s11748-017- 0874-x
3. Elefteriades JA, Farkas EA. 2010. Thoracic aortic aneurysm clinically pertinent controversies and uncertainties. J Am Coll Cardiol. 55: 841-857. Ref.: https://pubmed.ncbi.nlm.nih.gov/20185035/ DOI: https://doi.org/10.1016/j.jacc.2009.08.084
4. Lavall D, Schäfers HJ, Böhm M. 2012. Aneurysms of the ascending aorta. Dtsch Arztebl Int. 109: 227-233. Ref.: https://pubmed.ncbi.nlm.nih.gov/22532815/ DOI: https://doi.org/10.3238/arztebl.2012.0227
5. Dudzinski DM, Isselbacher EM. 2015. Diagnosis and Management of Thoracic Aortic Disease. Curr Cardiol Rep. 17: 106. Ref.: https://pubmed.ncbi.nlm.nih.gov/26468124/ DOI: https://doi.org/10.1007/s11886-015- 0655-z
7. Mathur A, Mohan V, Ameta D. 2016. Aortic aneurysm. J Transl Int Med. 4: 35-41. Ref.: https://pubmed.ncbi.nlm.nih.gov/28191516/ DOI: https://doi.org/10.1515/jtim-2016-0008
8. Alhabdan MS, AlSehly AA. 2011. Ascending aortic aneurysm. Pediatr Cardiol. 32: 1266- 1268. Ref.: https://pubmed.ncbi.nlm.nih.gov/21894548/ DOI: https://doi.org/10.1007/s00246-011- 0103-9
9. Wang TKM, Desai MY. 2020. Thoracic aortic aneurysm: optimal surveillance and treatment. Cleve Clin J Med. 2020; 87: 557-568. Ref.: https://pubmed.ncbi.nlm.nih.gov/32868306/ DOI: https://doi.org/10.3949/ccjm.87a.19140- 1
10. Ambepitiya SG, Michiue T, Bessho Y. 2010. An unusual presentation of thoracic aortic aneurysm rupturing into the esophagus: an autopsy case report. Forensic Sci Med Pathol. 6: 121-126. Ref.: https://pubmed.ncbi.nlm.nih.gov/20087793/ DOI: https://doi.org/10.1007/s12024-009- 9137-1
11. Felix AS, Alves LA, Felipe AR. 2018. Pulmonary Artery Compression and Invasion by a Ruptured Giant Thoracic Aortic Aneurysm: a Rare Presentation. CASE. 2: 201- 206. Ref.: https://pubmed.ncbi.nlm.nih.gov/30370383/ DOI: https://doi.org/10.1016/j.case.2018.02.005
12. Sarangi PK, Hui P, Sagar HS. 2017. Combined Left Recurrent Laryngeal Nerve and Phrenic Nerve Palsy: a Rare Presentation of Thoracic Aortic Aneurysm. J Clin Diagn Res. 11: 1-2. Ref.: https://pubmed.ncbi.nlm.nih.gov/28658876/DOI: https://doi.org/10.7860/jcdr/2017/25035.9765
13. Bicer M, Yuksel A, Kan II. 2020. The Largest Reported Giant Ascending Aortic Aneurysm Presented with Superior Vena Cava Syndrome. Braz J Cardiovasc Surg. 35: 834-837. Ref.: https://pubmed.ncbi.nlm.nih.gov/33118751/ DOI: https://doi.org/10.21470/1678-9741- 2019-0151
14. Porapakkham P. 2019. Impending rupture of aortic aneurysm eroding skin and sternum: a rare condition. Asian Cardiovasc Thorac Ann. 27: 307-309. Ref.: https://pubmed.ncbi.nlm.nih.gov/30781972/ DOI: https://doi.org/10.1177/0218492319833280
15. Booher AM, Eagle KA. 2011. Diagnosis and management issues in thoracic aortic aneurysm. Am Heart J. 162: 38-46. Ref.: https://pubmed.ncbi.nlm.nih.gov/21742088/ DOI: https://doi.org/10.1016/j.ahj.2011.04.010




















