Indexing & Abstracting
Full Text
Case ReportDOI Number : 10.36811/jcri.2021.110025Article Views : 1Article Downloads : 0
A case report of Urinary bladder injury post laparoscopic appendectomy: A rare complication
Aliya Ishaq*, Moaza Hashim Albedwawi, Siddhart Sankar Das, Nisha Nahar, Husni Shalak, Zaid Abdulaziz, Yasir Amin, Atif Latif, Rasih Mustafa, Syed Javeed and Esaaf Hasan Ghazi
Department of General Surgery, Liaquat National University Hospital, Karachi, Pakistan
*Corresponding Author: Aliya Ishaq, Department of General Surgery, Liaquat National University Hospital, Karachi, Pakistan, Email: aishaq@dha.gov.ae
Article Information
Aritcle Type: Case Report
Citation: Aliya Ishaq, Moaza Hashim Albedwawi, Siddhart Sankar Das, et al. 2021. A case report of Urinary bladder injury post laparoscopic appendectomy: A rare complication. J Case Rept Img. 3: 50-56.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2021; Aliya Ishaq
Publication history:
Received date: 30 September, 2021Accepted date: 06 October, 2021
Published date: 07 October, 2021
Abstract
Urinary bladder injury is a rare complication of laparoscopic abdominal surgery. The incidence is low and usually goes unidentified with confusing presentation. We report a case of such injury during laparoscopic appendectomy that was identified on 3rd post-operative day and a small 1 cm tear was found at posterior wall of bladder which and was repaired. There was also a collection anterior to bladder which was drained separately under radiological guidance later as on table cystogram did not show any leak anterior to bladder. Patient also had covid pneumonia during stay and patients stay and recovery was prolonged. Attention must be paid to port insertion under vision especially low insertion of supra pubic port should be avoided with pre op catheterization and key to diagnosis of injury is awareness of this rare entity.
Keyword: Laparoscopic Appendectomy; Bladder Injury; Uroperitonium
Introduction
Bladder injury is a rare recognized complication of laparoscopic surgery and is reported to occur in approximately 0.02–8.5% of adult general surgery cases. Its 0.36% in laparoscopic appendectomies [1]. If bladder injury is unidentified intraoperatively can present with subsequent unclear and confusing clinical presentation. The patient may present with symptoms of intense and persistent abdominal pain due to urinary peritonitis as well as biochemical changes that introduce serious doubts and diagnostic difficulties while mimicking an acute renal failure [1-4]. Prevention of bladder injury depends on knowledge of anatomy ,emptying of urinary bladder before starting procedure ,insertion of secondary trocars under vision and insertion of supra pubic trocar well above the symphysis pubis [1]. We report a case of iatrogenic urinary bladder injury that happened during laparoscopic appendectomy for a straight forward minimally inflamed appendix for a 17 years old male patient and will discuss the measures that can be taken to minimize the risk of such injuries.
Case Report
17 years old previously healthy with no co-morbidities male patient presented to accident and emergency with 2 days h/o generalized abdominal pain shifting to RIF associated with nausea ,no vomiting ,no fever and no urinary symptoms. He never had such symptoms before. Past surgical history was insignificant as well. On examination he was stable hemodynamically with tenderness and rebound tenderness in RIF however abdomen was soft, non-tender. His base line investigations showed normal white blood count and other septic markers and urine analysis was within normal limits as well. He had and ultrasound from another hospital suggestive of appendicitis. Since history and physical examination was suggestive of appendicitis so patient was posted for laparoscopic appendectomy. He was thin and lean built patient and prior to surgery as per protocol urinary bladder was emptied. Laparoscopic appendectomy was performed and 5 mm supra umbilical port was made for camera introduction using verus needle.10 mm LIF and 5 mm supra pubic ports were made under vision .Intra operative findings were acutely inflamed appendix mainly at tip with healthy base. Appendicular mesentery was ligated using bipolar forceps and single endo lop was applied at base and appendix was taken out using endo bag. Patient was examined at the evening of surgery was stable vitally and was c/o abdominal pain, his abdomen was soft, mild tenderness was at sites of surgical dressings, otherwise he was up and about and tolerated diet and passed stool and urine. Patent was reassured and was decided to discharge him next morning.
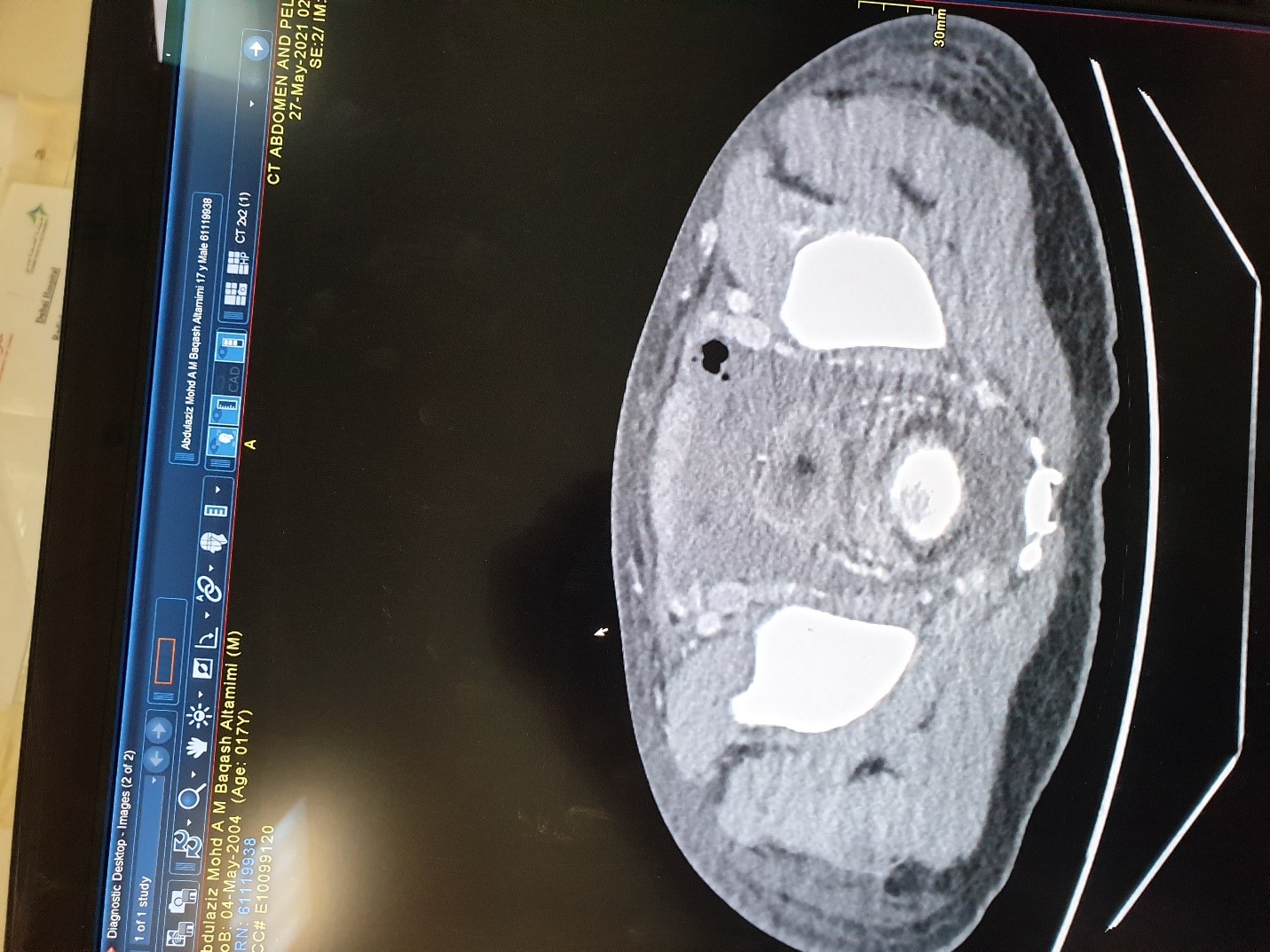
Next morning patient was still c/o mild generalized abdominal pain however hemodynamic and abdominal examination was fine ,he was tolerating diet ,passed stool and urine so pain was attributed to low threshold and young age of patient. However the decision was taken not to discharge him and analgesia was increased. On 3rd post-operative day patient was having even more pain and abdominal tenderness increased with guarding, patient was little techy cardiac. At this point of time along with base line investigations CT scan abdomen with contrast was arranged for the patient. Ct scan abdomen with contrast showed moderate ascetic fluid collection intra abdominally with thickening of small bowel and no leakage of contrast as shown in images below:
Arterial blood gases were suggestive of metabolic acidosis. Based on clinical ,radiological and laboratory findings patient was taken to operation theatre and diagnostic laparoscopy was done and intraoperatively around 1500 ml of turbid fluid was found, appendicular stump was healthy and secured ,all the bowel was run and no perforation was found ,suddenly it was noted that all wash out fluid is draining through Foley’s catheter. Methylene blue was injected through foley’s catheter and it was clamped and blue liquid seen coming through a small less than 1 cm perforation at the posterior wall of intraperitoneal part of urinary bladder. Intraoperative urology consultation was taken and laparoscopic urinary bladder tear was done using PDS 3/0 interrupted double layer.Post repair cystogram was done on table and no leak was found as shown in diagram below:
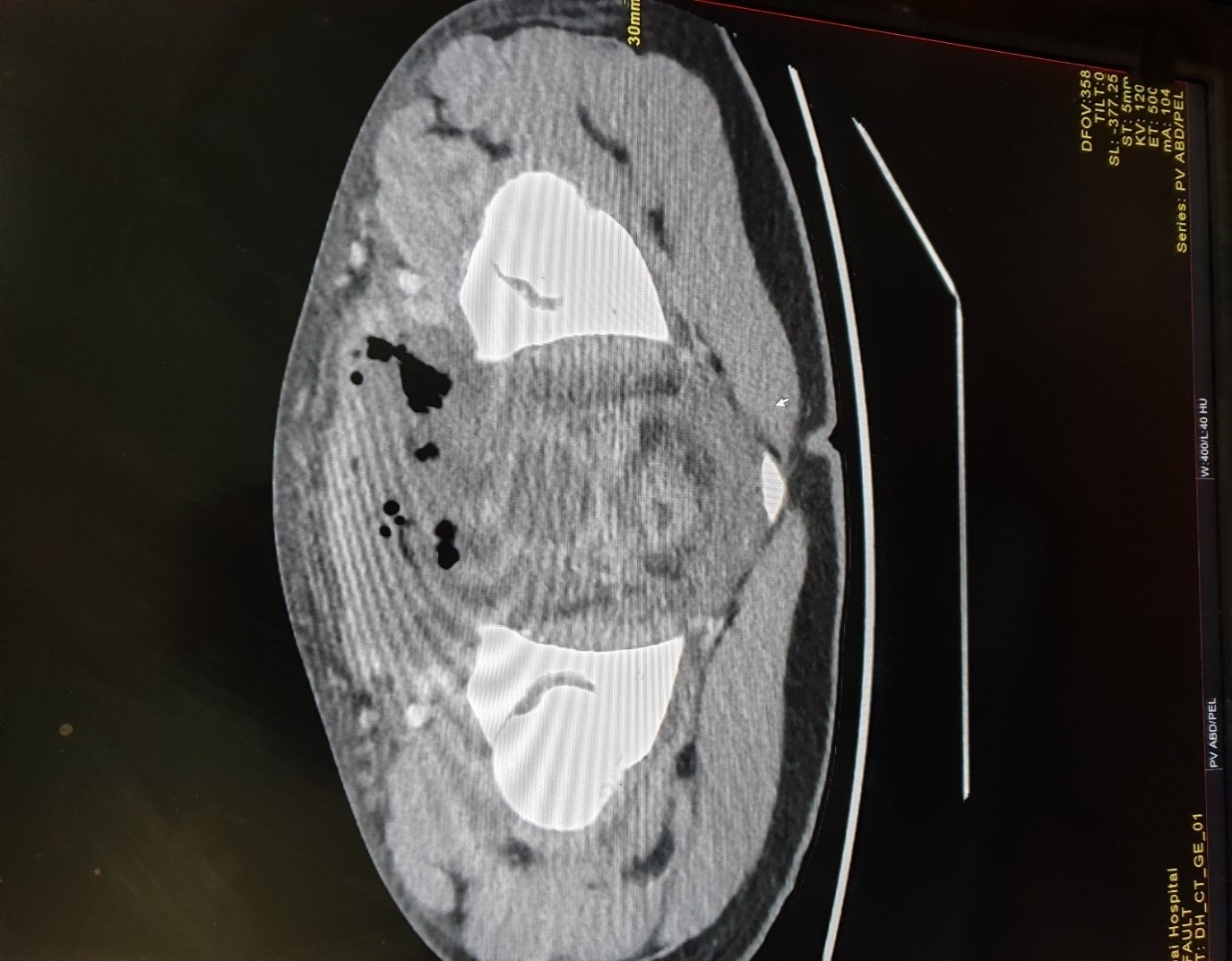
Ct scan abdomen showing air in pelvis with collection, no leakage of contrast.
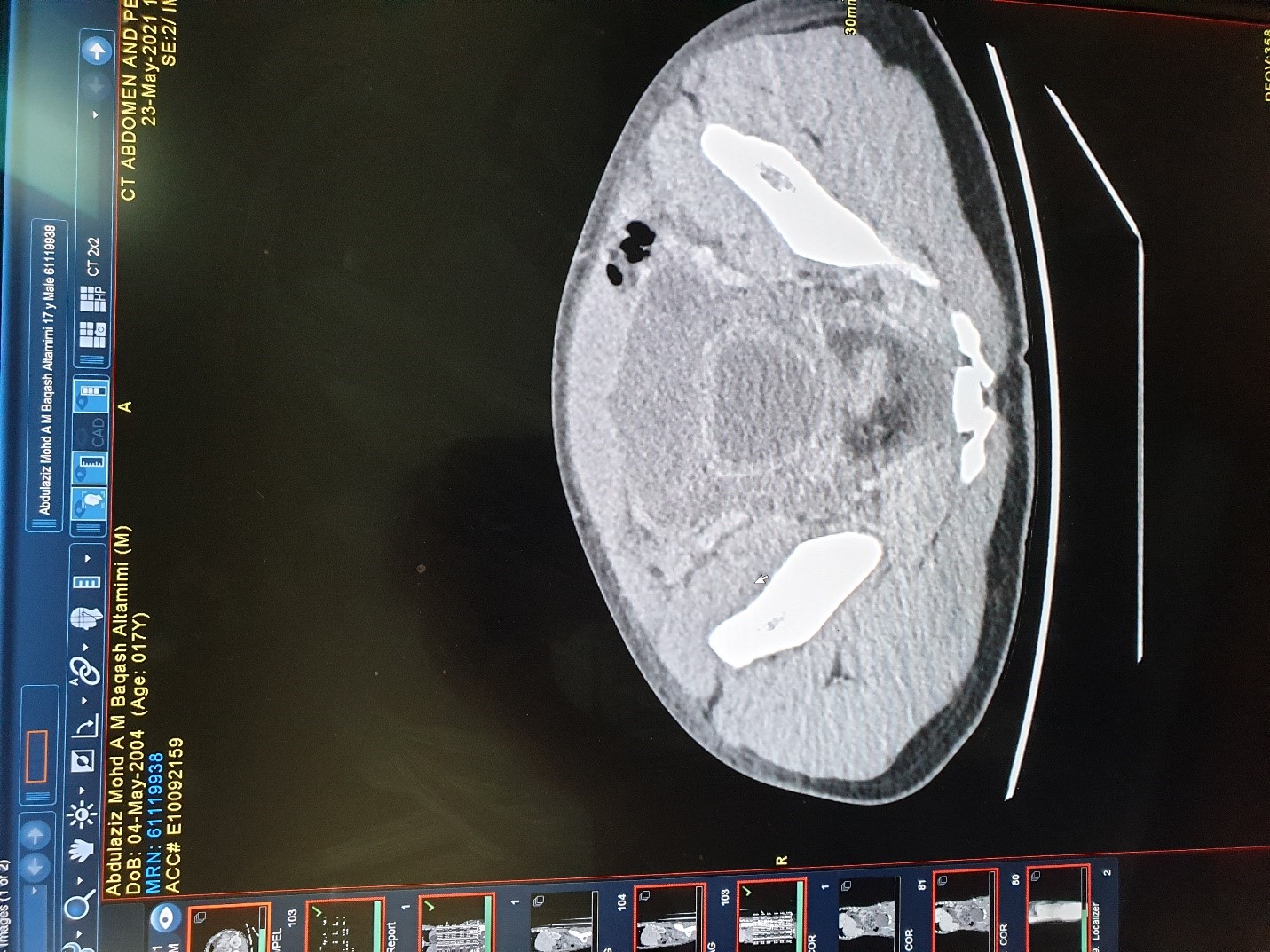
Ct scan abdomen showing air in pelvis with collection and thick-walled urinary bladder, no leakage of contrast.
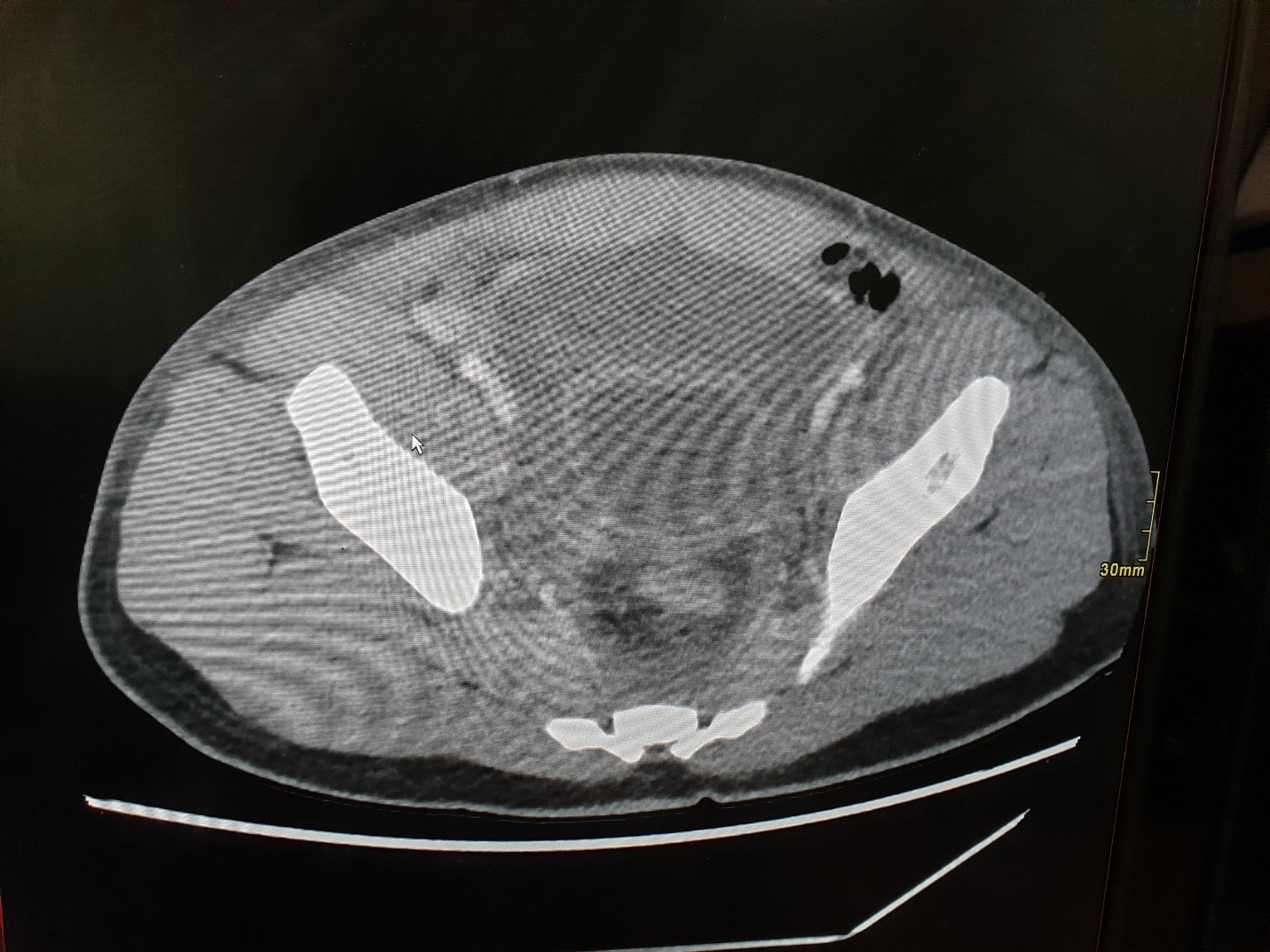
Ct scan abdomen showing air in pelvis with collection and thick walled urinary bladder, no leakage of contrast.
CRP was 423.1 mg/l
Na –127 mmol/l
Urea—79 mg/dl
Creat—2.3 mg/dl
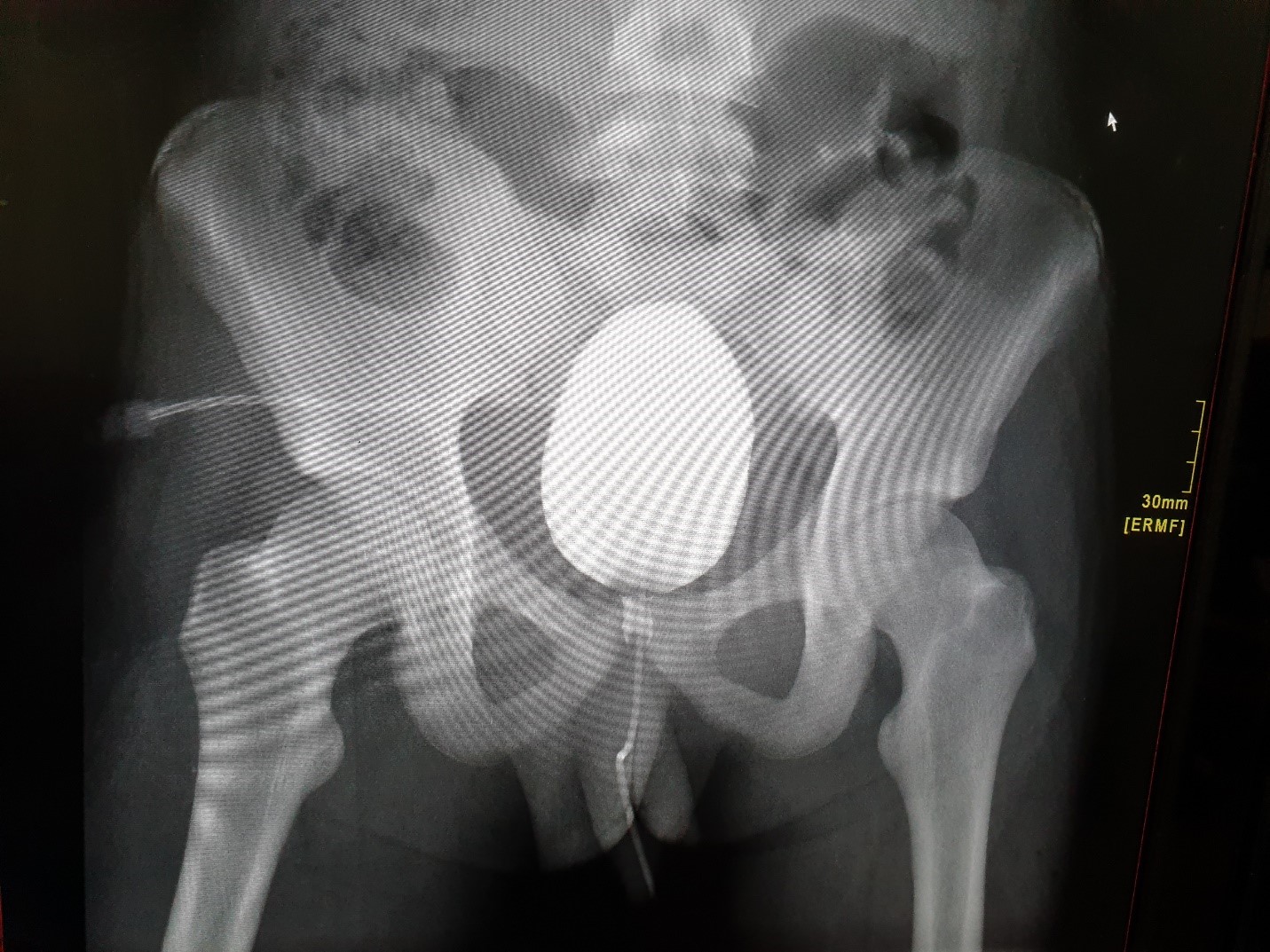
Preoperative cystogram done post repair of bladder injury showing no leak.
Thorough wash out was done with 9-10 liters of saline and pelvic drain was placed and it was decided by urology team to keep Foley’s catheter for 15 days. Patient was having persistent techy cardia and shortness of breath post operatively and was requiring high oxygen. Respiratory efforts were poor and chest x- ray was suggestive of infiltrates. His covid swab was repeated and it came positive. Patient was shifted to isolation high dependency and covid team was involved in management. Patient had slow recovery and gradually improved over a period of 4-5 days with negative covid and was shifted back to surgical ward. His drain output pelvic was still having 100-150 ml/day and cultures were taken again. He was started on antibiotic as per culture report. On 7th post-operative day of 2nd surgery patient started having discharge from supra pubic port ,culture was sent and repeat CT scan done which showed a collection around 11.8 x 3.2 cm anterior to urinary bladder as shown below;
Ct scan abdomen showing collection anterior to urinary bladder.
This collection was drained radiologically and drain was placed as well. Drain output gradually reduced over a period of one more week and both drains were taken out one by none. Patient also improved clinically and became hemodynamically stable with healthy healed wounds and no pain, on regular diet. His foley’s catheter was removed as well after 2 weeks after repeating cystogram which showed no leak and he was passing normal urine. As an analysis of our case the first port was made after identifying the rectus sheath using verus needle and all other subsequent ports were made under vision, urinary bladder was empty as well pre procedure and intraoperatively bladder was not found to be distended. No injury identified during the procedure more ever it was a simple minimally inflamed appendix and surgery took 10 minutes only. What made perforation is unclear but may be because of diathermy?? But we used bipolar only for short period of time. Another explanation was patient was thin and lean built and was only 17 years old so may be bladder was intra peritoneal but bladder fold was well identified. We don’t catheterize patient but do let them empty urinary bladder. May be routine use of pre op catheterization can be more safe. Also we did not put any drain as it was not indicated but if there would have been drain it would have picked up the perforation earlier. Our patient also had post-operative covid pneumonia that made his recovery more slow also collection anterior to bladder was drained late. Collection anterior to bladder is also raising possibility of through and through peroration involving both anterior and posterior bladder walls but that was not evident while on table cryptogram was done.
Discussion
Urinary bladder injury post laparoscopic appendectomy is a possible yet rare complication. Electrosurgical dissection is reported as the most likely cause of bladder injury followed by blunt dissection of bladder followed by trocar insertion [1]. As an analysis of our case the first port was made after identifying the rectus sheath using verus needle and all other subsequent ports were made under vision ,urinary bladder was empty as well pre procedure and intraoperatively bladder was not found to be distended. No injury identified during the procedure more ever it was a simple minimally inflamed appendix and surgery took 10 minutes only. What made perforation is unclear but may be because of diathermy?? But we used bipolar only for short period of time. Another explanation was patient was thin and lean built and was only 17 years old so may be bladder was intra peritoneal but bladder fold was well identified.
Bladder perforations are not always easy to detect intra operatively but signs of bladder perforation per operatively are presence of bloody urine, gaseous distension of urinary bladder [1]. In our case patient was not catheterized and we did not notice any bladder distension during the procedure. We don’t catheterize patient but do let them empty urinary bladder. May be routine use of pre op catheterization can be more safe. If bladder injury is missed intraoperatively then patient can present in post op period with oliguria, hematuria, abdominal distension, fever, nausea and vomiting [1]. In our case patient did not report hematuria or oliguria however the output charting was not accurately measured as patient was not catheterized and it was straight forward case and patient did not report any abnormality. In case of urinary ascites patient can present with abdominal distension and disturbance of renal biochemistry in terms of elevated urea, creatinine and hyponatremia and hyperkalemia [1,2]. Our patient had abdominal distension with raised urea creatinine as well as hyponatremia, but it was picked up on 3rd post-operative day. Our suprapubic trocar was not very well above the symphysis pubis that can be a contributing factor for bladder injury. Also we did not put any drain as it was not indicated but if there would have been drain it would have picked up the perforation earlier. Our patient also had post-operative covid pneumonia that made his recovery more slow also collection anterior to bladder was drained late. Collection anterior to bladder is also raising possibility of through and through peroration involving both anterior and posterior bladder walls but that was not evident while on table cystogram was done [5-11].
Conclusion
Although the incidence of bladder injury is low, its importance is highlighted by the large number of laparoscopies being performed. In addition to catheterization of the patient, care must be taken with the insertion of low suprapubic ports and consideration should be made regarding alternative sites. Adequate laparoscopic supervision and training in port site planning is required for surgical trainees.
Learning points
• During laparoscopic appendectomy pre-operative catheterization till the end of surgery should be practiced to keep bladder deflated.
• Cautious use of mono and bipolar.
• Post-operative unusual pain even on first post-operative day should be investigated. Post appendectomy urine output monitoring should be strict till patient is discharged.
• Low insertion of supra pubic port should be avoided or should be replaced by alternate port sides.
References
1. Levy BF, De Guara J, Wilson PD. 2012. Bladder injuries in emergency/expedited laparoscopic surgery in the abscence of previous surgery: a case series. Ann R Coll Surg Engl. 94: 118-120. Ref.: https://pubmed.ncbi.nlm.nih.gov/22507707/ DOI: https://doi.org/10.1308/003588412x13171221502149
2. Heyns CF, Rimington PD. 1987. Intraperitoneal rupture of the bladder causing the biochemical features of renal failure. Br J Urol. 60: 217-222. Ref.: https://pubmed.ncbi.nlm.nih.gov/3676665/ DOI: https://doi.org/10.1111/j.1464-410x.1987.tb05486.x
3. Vilos GA, Haebe J, Crumley TL. 2001. Serum biochemical changes after laparoscopy may be indicators of bladder injury. J Am Assoc Gynecol Laparosc. 8: 285-290. Ref.: https://pubmed.ncbi.nlm.nih.gov/11342739/ DOI: https://doi.org/10.1016/s1074-3804(05)60592-0
4. Kruger PS, Whiteside RS. 2003. Pseudo-renal failure following the delayed diagnosis of bladder perforation after diagnostic laparoscopy. Anaesth Intensive Care. 31: 211-213. Ref.: https://pubmed.ncbi.nlm.nih.gov/12712789/ DOI: https://doi.org/10.1177/0310057x0303100214
5. Kruger PS, Whiteside RS. 2003. Pseudo-renal failure following the delayed diagnosis of bladder perforation after diagnostic laparoscopy. Anaesth Intensive Care. 31: 211-213. Ref.: https://pubmed.ncbi.nlm.nih.gov/12712789/ DOI: https://doi.org/10.1177/0310057x0303100214
6. Tang KK, Wong CK, Lo SF. 2005. Is it necessary to catheterise the bladder routinely before gynaecological laparoscopic surgery? Aus NZ J Obstet Gynaecol. 45: 380-383. Ref.: https://pubmed.ncbi.nlm.nih.gov/16171472/ DOI: https://doi.org/10.1111/j.1479-828x.2005.00443.x
7. Lamaro VP, Broome JV, Vancaillie TG. 2000. Unrecognized bladder perforation during operative laparoscopy. J Am Assoc Gynecol Laparosc. 7: 417-419. Ref.: https://pubmed.ncbi.nlm.nih.gov/10924641/ DOI: https://doi.org/10.1016/s1074-3804(05)60490-2
8. Ho AM, Roth P, Cowan WD. 1996. Gaseous distension of the urinary bag indicating bladder perforation during laparoscopic pelvic procedures. Int J Gynecol Obstet. 55: 297-298. Ref.: https://pubmed.ncbi.nlm.nih.gov/9003958/ DOI: https://doi.org/10.1016/s0020-7292(97)82728-2
9. Nachshen S, Abusaid D, Nauta M. 2008. The "catheter bag" sign revisited: A simple way detecting bladder truma during operative laparoscopic procedures. Arch Gynaecol Obstet. 277: 65-66. Ref.: https://pubmed.ncbi.nlm.nih.gov/17619890/ DOI: https://doi.org/10.1007/s00404-007-0413-6
10. Tran H, Petrovsky N. 2004. A swollen abdomen. Pathology. 36: 193-195. Ref.: https://pubmed.ncbi.nlm.nih.gov/15203757/ DOI: https://doi.org/10.1080/00313020410001672055
11. Tai CK, Li SK, Hou SM. 2008. Bladder injury mimicking acute renal failure after cesarean section. Surg Laparosc Endosc Percutan Tech. 18: 301-303. Ref.: https://pubmed.ncbi.nlm.nih.gov/18574423/ DOI: https://doi.org/10.1097/sle.0b013e31816907e6




















