Indexing & Abstracting
Full Text
Research ArticleDOI Number : 10.36811/jcri.2021.110021Article Views : 40Article Downloads : 30
Anatomical location of undescended testes and comparison between their size at different anatomical locations: A cross sectional study
Aliya Ishaq* , Mariya Ishaq, Muhammad Shadab Khan, Abida Parveen, Muhammad Jamshaid Hussain Khan and Shabbir Hussain
, Mariya Ishaq, Muhammad Shadab Khan, Abida Parveen, Muhammad Jamshaid Hussain Khan and Shabbir Hussain
Department of General Surgery, Liaquat National University Hospital, Karachi, Pakistan
*Corresponding Author: Aliya Ishaq, Department of General Surgery, Liaquat National University Hospital, Karachi, Pakistan, Email: aishaq@dha.gov.ae
Article Information
Aritcle Type: Research Article
Citation: Aliya Ishaq, Mariya Ishaq, Muhammad Shadab Khan, et al. 2021. Anatomical location of undescended testes and comparison between their size at different anatomical locations: A cross sectional study. J Case Rept Img. 3: 16-26.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2021; Aliya Ishaq
Publication history:
Received date: 12 May, 2021Accepted date: 22 May, 2021
Published date: 25 May, 2021
Abstract
Introduction: Undescended testis (UDT) or cryptorchidism is a common childhood condition in which a boy is born without having one or both testes in their scrotum. It is a very frequent clinical finding in boys, with a prevalence of about 2-4%. The inguinoscrotal phase of testicular descent normally takes place in the last trimester of pregnancy. The regulation of prenatal testicular descent in humans is not fully understood, but numerous genetic and endocrinal factors are thought to have been involved. Preterm boys have been described to have a higher rate of UDT. The classification of UDT is performed according to palpable or nonpalpable testis. If the testis is located inside the normal path of descent, the testis is called ’intra-abdominal’, for those located in the abdomen is called ’intracanalicular’, for those located between the internal and external rings or ’suprascrotal’, for those located between the entrance of the scrotum and the external ring. This study was conducted to determine the frequency of anatomical location of undescended testis in pediatric patients undergoing orchidopexy as well as to compare the mean size of undescended testis at different anatomical location in pediatric patients undergoing orchidopexy as a secondary objective.
Methods: It’s a cross sectional study of 94 patients with total 110 testes as per inclusion criteria. Study was performed at pediatric surgery department of Liaquat National university hospital Karachi, Pakistan for a duration of eight months. Orchidopexy was performed under general anesthesia as a surgical day care procedure. At orchiopexy, the outcome variables i.e. location and size of the testis was noted. The size of the testis was measured in anteroposterior and mediolateral dimensions vernier caliper, graduated in mm. The size of testis was calculated by modified Lambert’s formula (0.71xlengthxwidth2). All the collected data were entered into the proforma attached at the end.
Results: Mean±SD of age was 4.29±2.19 with C.I (3.38…….4.74) years. Mean±SD of size of testis was 425.68±244.43 with C.I. (375.89……..475.47) mm. In location of testis 4 (4.2%) was located at intra-abdominal, 15 (16%) at intracanalicular and 75 (79.8%) was located at distal to superficial ring. Mean size of testis in intra-abdominal location was 276.29±145.47, intra-canalicular 367.89±196.15, distal to superficial ring was 442.27±54.08 and non-significant P-value was found i.e. (p=0.264).
Conclusion: No significant difference was found between mean size of testis and location of undescended testis. The most common location was distal to superficial ring.
Keyword: Testes; Undescended; Anatomical Location; Orchidopexy; Anatomical Location
Introduction
Undescended testis (UDT), or cryptorchidism, is the failure of one or both testes to descend to a normal scrotal position and is the most common genital anomaly in boys [1]. Although a large proportion of cases descend spontaneously to a normal position by 3 months of age, nearly 1% remain undescended and require surgery [1]. Orchiopexy is the standard intervention for congenital undescended testes (UDTs), which is recommended within the age of 6-12 months [1]. The importance of surgery for UDT is underpinned by the fact that boys with UDT have an increased risk of testicular cancer later in life. In addition, it has been shown that UDT inhibits the differentiation of primitive germ cells, starting at 4 to 12 months, which is crucial for the production of germ cells that subsequently enable spermatogenesis [1]. Delayed repositioning of an undescended testis may result in a reduction in germ cell development and low testicular volume, potentially diminishing subsequent fertility. Incomplete descent of one or both testicles from the abdominal cavity, through the inguinal canal into the scrotum (cryptorchidism) is a multifactorial etiology abnormality that affects 1-1.8% of male infants [1]. It is reported to be associated with infertility and testicular cancer [2]. However, based on several studies that show that undescended testes undergo early and progressive deterioration, the recommended age for treatment has been decreasing gradually as we have improved our understanding of spermatogenesis [1]. Cryptorchidism (undescended testis) is a common disease in pediatric urology, with an incidence of approximately 3% in term infants and 30.1% in premature babies that drops to 0.7- 0.8 % after the first year of life due to spontaneous descent [3]. Approximately 20% of undescended testes (UDT) are non-palpable on presentation, and 40–60% of non-palpable testis was found to be absent or a nubbin on exploration [1]. Despite of extensively written literature concerning undescended testis, many facts of this entity are poorly understood and the effectiveness in terms of functional outcome, has yet to be determined [1]. Mean size of undescended testis was reported by Hussain TS et al, at intra-abdominal testis (1.347±1.18), deep inguinal ring (2.41±2.52), and canalicular (1.22±1.40) and found statistically insignificant difference between the different anatomical locations [4]. Many surgeons and physicians generally assume that size of undescended testis is affected by location and age of presentation [1].
It is generally believed that in patients with intra-abdominal testis and the one who present at later age, the testicular size would be small [1]. Undescended testis is very prone to the low fertility and high rate of occurrence of neoplasm locating them at the earliest is important [1]. Studies reported anatomical location of undescended testis i.e. intraabdominal (36%) [1], deep inguinal ring (69%) [5], canalicular (27%) [5], the descent of the testes consists of the opening of a connection from the testis from abdomen to its final location in scrotum with the development of the gubernaculum, which subsequently pulls and translocates the testis down into the developing scrotum. Ultimately, the passageway closes behind the testis [5].
Rationale: This study is planned to assess the anatomical location and mean size of undescended testis in pediatric patients undergoing orchidopexy. Currently, no national data is available on the same, therefore, it is important to investigate the status of it, so that treatment of such patients should be anticipated in appropriate clinical line and appropriate diagnosis is must be made to prevent complications. Moreover, this study was helped to made strategies and formulate an appropriate management plan to reduce morbidity and complications in this already compromised group of patients.
Primary Objective: To determine the frequency of anatomical location of undescended testis in pediatric patients undergoing orchidopexy.
Secondary Objective: To compare the mean size of undescended testis at different anatomical location in pediatric patients undergoing orchidopexy.
Operational Definition
Undescended Testis: It was defined as a testis that cannot be manipulated into a stable scrotal position in its most caudal position and not palpable in the scrotum since birth assess clinically and confirmed on USG [1,2].
Anatomical Locations
Intraabdominal: Is an undescended testis located in abdominal cavity assess per operatively.
Canalicular: Is an undescended testis located between the internal and external inguinal rings assess per operatively [5-12].
Near to deep Inguinal Ring: Is an undescended testis near to deep inguinal ring assess per operatively [6-10].
Material and Methods Study Design: Descriptive Cross-Sectional Study.
Settings: Study was conducted in Peadiatric Surgery Department (including patients presenting for orchiopexy) at Liaquat National Hospital Karachi between Jan 2019 to Sep 2019.
Duration of Study: 8 months. Sample Size: By using W.H.O sample size calculator using frequency of canalicular (27%), Confidence level (95%), Margin of error (d) = 9% then the estimated sample size was n=94.
Sample technique: Non-Probability Consecutive Sampling.
Sample Selection:
Inclusion Criteria
• Male children
• Children between age group1 to 13 years
• Patients with undescended testis (as mention in operational definition) but normal looking genitalia who presented for surgery in day care OT.
Exclusion Criteria
• Ectopic and retractile testes (assess clinically).
• Abnormal looking genitalia (disorders of sexual differentiation) or those presenting with pen scrotal hypospadias
• Children who presented with torsion (assess through USG)
• History of previously operated testis.
Data Collection Procedure
This study was conducted after approval of synopsis from CPSP9 college of physicians and surgeons of Pakistan) and Ethical review committee of Liaquat National Hospital. All the patients who fulfill the inclusion criteria were included in the study. A written informed consent was taken from parents/guardians of each children before enrolling them into study. Patient clinical history and examination was done by principle investigator before going to the operation theater on operative day. Detailed history and clinical examination of children was taken by the principle investigator. Physical examination was performed, and findings recorded regarding the side, whether it was palpable or not, its location, either inguinal or pubic. Orchidopexy was performed under general anesthesia as a surgical day care procedure (was admitted and discharged on same day of surgery) by principle investigator under the supervision of consultant Pediatric Surgeon with>5-year experience in pediatric surgery. At orchiopexy, the outcome variables i.e. location and size of the testis was noted. The size of the testis was measured in anteroposterior and Medio lateral dimensions using Vernier caliper, graduated in mm. The size of testis was calculated by modified Lambert’s formula (0.71xlengthxwidth2). Effect modifiers / confounders variables and bias was controlled by strictly following the inclusion and exclusion criteria. All the collected information was entered into the predesigned Performa.
Data Analysis
Data was analyzed by using SPSS version 21. Mean and standard deviation were computed for quantitative variable i.e. age and size of testis. Frequency and percentage were calculated for side and location of the testis i.e. (intraabdominal, intracanalicular, distal to superficial ring). ANOVA was applied to compare the mean size of the undescended testis at different anatomical location i.e. (intraabdominal, intracanalicular, distal to superficial ring consider P ≤ 0.05 as significant. Effect modifiers were controlled through stratification of age and side of testis to see the impact of these on outcome variables by using chi- square test and ANOVA consider P≤0.05 as significant.
Results
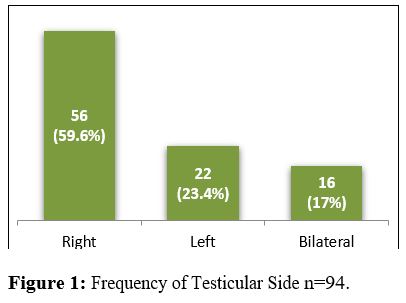
In this study total number of patients were 94 and total number of testis were 110 included to assess the anatomical location and mean size of undescended testis in patients undergoing orchidopexy , in distribution right sided testis were 56 , left sided testis were 22 and bilateral testis were 16 and the results were analyzed as Mean±SD of age of 94 patients were 4.277±2.510 with C.I (3.76…….4.791 ) years as shown in Table 1. Mean±SD of size of testis of 94 patients were 440.94±273.11 with C.I. (385.00…….496.88) mm as shown in Table 2. Stratification of age group with size of testis Table 3. Stratification of side of testis with size of testis Table 4. Descriptive statistics of age Table 5. Descriptive statistics of size of testis Table 6. In distribution for side of testis 56 (59.6%) was found in right side, 22 (23.4%) was in left side and bilateral side was noted at 16 (17%) patients as shown in figure 1. In frequency for testicular side with total number of testis (total left and total right including B/L) figure 2.
In frequency for location of testis 6 (5.5 %) was located at intraabdominal, 21 (9.1%) at intracanalicular and 83 (75.5%) testis was located at distal to superficial ring as shown in figure 3. In comparison between mean size of testis and anatomical location non-significant difference was noted and p-value was found to be (P=0.370) as shown in table 7. Stratification of age and side of testis was done with respect to location and size of the testis from [Table 8-11].
|
Table 1: Descriptive statistics of age n=94. |
||||
|
Descriptive |
Statistic |
Std. Error |
||
|
|
Mean |
4.277 |
0.259 |
|
|
|
95% Confidence Interval for Mean |
Lower Bound |
3.762 |
|
|
|
Upper Bound |
4.791 |
|
|
|
|
5% Trimmed Mean |
4.077 |
|
|
|
|
Median |
3.5 |
|
|
|
|
Variance |
6.304 |
|
|
|
Age |
Std. Deviation |
2.5109 |
|
|
|
[In Years] |
Minimum |
1 |
|
|
|
|
Maximum |
13 |
|
|
|
|
Range |
12 |
|
|
|
|
Interquartile Range |
2.5 |
|
|
|
|
Skewness |
1.356 |
0.249 |
|
|
|
Kurtosis |
1.841 |
0.493 |
|
|
Table 2: Descriptive statistics for size of testis n=94. |
||||
|
Descriptive |
Statistic |
Std. Error |
||
|
|
Mean |
440.9482 |
28.16974 |
|
|
|
95% Confidence Interval for Mean |
Lower Bound |
385.0087 |
|
|
|
Upper Bound |
496.8877 |
|
|
|
|
5% Trimmed Mean |
412.6612 |
|
|
|
|
Median |
382.69 |
|
|
|
|
Variance |
74592.19 |
|
|
|
|
Std. Deviation |
273.1157 |
|
|
|
|
Minimum |
79.52 |
|
|
|
|
Maximum |
1635.13 |
|
|
|
Size of Testis |
Range |
1555.61 |
|
|
|
[In mm] |
Interquartile Range |
242.62 |
|
|
|
|
Skewness |
2.067 |
0.249 |
|
|
|
Kurtosis |
5.747 |
0.493 |
|
|
Table 3: Stratification of age group with size of testis n=94. |
|||
|
Outcomes |
Age [In Years] |
||
|
1-5 (n=74) |
>5 (n=20) |
||
|
Size of Testis |
Mean |
422.66 |
508.58 |
|
[In mm] |
±SD |
251.03 |
341.85 |
|
|
P-Value |
0.214 |
|
|
Applied independent t-test |
|||
|
Table 4: Stratification of side of testis with size of testis n=94. |
||||
|
Outcomes |
Testicular Side |
|||
|
Right (n=56) |
Left (n=22) |
Bilateral (n=16) |
||
|
Size of Testis |
Mean |
401.23 |
360.53 |
690.49 |
|
[In mm] |
±SD |
229.76 |
128.35 |
405.09 |
|
|
P-VALUE |
9.777 |
||
|
Applied ANOVA |
||||
|
Table 5: Descriptive statistics of age n=110. |
||||
|
Descriptive |
Statistic |
Std. Error |
||
|
|
Mean |
4.341 |
0.2576 |
|
|
|
95% Confidence Interval for Mean |
Lower Bound |
3.83 |
|
|
|
Upper Bound |
4.851 |
|
|
|
|
5% Trimmed Mean |
4.129 |
|
|
|
|
Median |
3.5 |
|
|
|
|
Variance |
7.298 |
|
|
|
Age |
Std. Deviation |
2.7015 |
|
|
|
[In Years] |
Minimum |
1 |
|
|
|
|
Maximum |
13 |
|
|
|
|
Range |
12 |
|
|
|
|
Interquartile Range |
2.5 |
|
|
|
|
Skewness |
1.321 |
0.23 |
|
|
|
Kurtosis |
1.449 |
0.457 |
|
|
Table 6: Descriptive statistics for size of testis n=110. |
||||
|
Descriptive |
Statistic |
Std. Error |
||
|
|
Mean |
477.246 |
29.2369 |
|
|
|
95% Confidence Interval for Mean |
Lower Bound |
419.2994 |
|
|
|
Upper Bound |
535.1926 |
|
|
|
|
5% Trimmed Mean |
442.6985 |
|
|
|
|
Median |
383.045 |
|
|
|
|
Variance |
94027.72 |
|
|
|
|
Std. Deviation |
306.6394 |
|
|
|
|
Minimum |
79.52 |
|
|
|
|
Maximum |
1635.13 |
|
|
|
Size of Testis |
Range |
1555.61 |
|
|
|
[In mm] |
Interquartile Range |
254.36 |
|
|
|
|
Skewness |
1.978 |
0.23 |
|
|
|
Kurtosis |
4.63 |
0.457 |
|
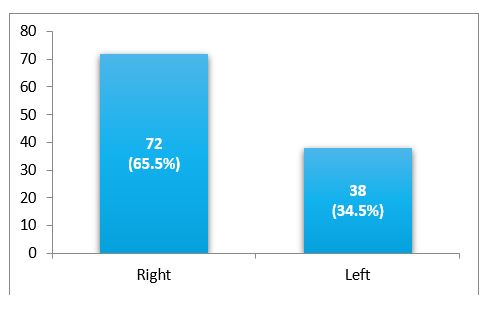
Figure 2: Frequency of Testicular Side n=110.
|
Table 7: Comparison of mean size of undescended testis n=110. |
||||
|
Outcomes |
Location of Testis |
|||
|
Intra-Abdominal (n=6) |
Intra-Canalicular (n=21) |
Distal To Superficial Ring (n=83) |
||
|
Size of Testis |
Mean |
307.17 |
473.04 |
490.6 |
|
[In mm] |
±SD |
±148.69 |
±235.11 |
±328.41 |
|
|
P-value |
0.37 |
||
|
Applied ANOVA. |
||||
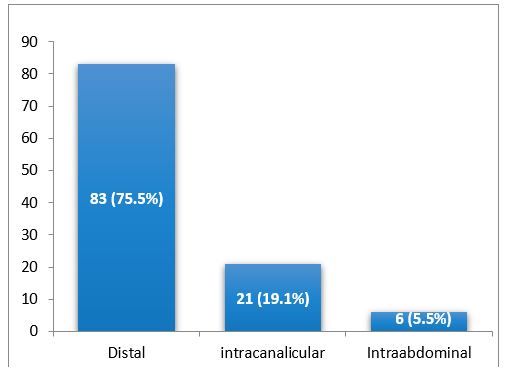
Figure 3: Frequency for anatomical location of undescended testis n=110.
|
Table 8: Stratification of age group with size of testis n=110. |
|||
|
Outcomes |
Age [in Years] |
||
|
1-5 (n=85) |
>5 (n=25) |
||
|
SIZE OF TESTIS |
Mean |
447.84 |
577.2 |
|
[In mm] |
±SD |
274.58 |
386.88 |
|
|
P-VALUE |
0.129 |
|
|
Applied independent t-test |
|||
|
Table 9: Stratification of age group with location of testis n=110. |
|||
|
|
Age [In Years] |
P-value |
|
|
1-5 (n=85) |
>5 (n=25) |
||
|
Intra-Abdominal |
1(1.2%) |
5(20%) |
|
|
Intra-Canalicular |
17(20%) |
4 (19%) |
0.005 |
|
Distal to Superficial Ring |
67 (78.8%) |
16 (19.3%) |
|
|
Applied chi square test. |
|||
|
Table 10: Stratification of side of testis with size of testis n=110. |
|||
|
Outcomes |
Testitcular side |
||
|
Right (n=72) |
Left (n=38) |
||
|
Size of Testis |
Mean |
465.51 |
499.46 |
|
[In mm] |
±SD |
300.36 |
321.1 |
|
|
P-value |
0.583 |
|
|
Applied independent t-test |
|||
|
Table 11: Stratification of side of testis with position of testis n=110. |
|||
|
Location of Testis |
Testitucar Side |
P-value |
|
|
Right |
Left |
|
|
|
Intra-Abdominal |
4 (66.7%) |
2 (5.3%) |
|
|
Intra-Canalicular |
14 (19.4%) |
7 (18.4%) |
|
|
Distal to Superficial Ring |
54 (75%) |
29 (76.3%) |
1 |
|
Applied chi square test. |
|||
Discussion
Undescended testis is one of the most common congenital urological anomalies in children. Although many advances have taken place in the management of patients with undescended testis, yet anatomical and descriptive features of cryptorchidism at physical examination lacks standardization. UDT not only cause psychological trauma to parents but also to child with advancing age. To avoid this and some of the deleterious effects of UDT like impaired fertility and malignancy in UDT, timely diagnosis and surgical treatment of UDT is essential [11,12]. Whenever a child presented to paediatric surgeon with any congenital anomaly it is very important to check his gonads also for UDT because different anomalies are associated with UDT as it was obvious from our study and other studies given below. In our study the common age of patient was 39 months. In this study from clinical standpoint we observed the location of testis as follows (4.2%) were at intraabdominal, (16%) at intracanalicular and (79.8%) at distal to superficial ring. Our result was supported by Kolon TF [7], and Schneck FX [1].
We also observed in our study that 49 (52%) was found in right side, 27 (29%) was in left side and 18 (19%) was found at bilateral side. Our result was supported by Bianchi A148 and Taqvi et al. [1]. Dcruz AJ3 and Favorito LA et al. [1]. From location standpoint we observe in our study that intracanalicular was the commonest site for both palpable and nonpalpable testes. Inguinal canal was a common site of location on local assessment, on u/s, and per-operatively. Taqi et al [13,14] proved approximately same results in their study on 107 Undescended testis, out of 107 testes 68 testes were located in the inguinal canal in our study out of 100 testes 70 (70%) were in the inguinal canal. Our result was also supported by Kolon TF [8], Dogra VS Showing location of UDT in inguinal canal 68% and 72% respectively. In our study non-significant difference was noted and p-value was noted between mean size of testis and anatomical location. Our results are comparable with other national and international studies. Kogan S et al [2] and Schneck FX et al [3] were of views that the most common ectopic location is within the superficial inguinal pouch between scarpa’s fascia and external oblique fascia. Our study supported these views as we found four palpable (4/59, 6.8%) ectopic located testis and all were within superficial inguinal pouch. Mesrobian H.Q.O et al [2] documented same result in their study carried out on 86 cryptorchid testis that there were10% cryptorchid testes and all were in the superficial inguinal pouch. Favorito LA et al [2] states that absent testis has an incidence of 3- 5%, Taqvi SRH et al [14] during their study on 107 testes revealed three absent testes. Mesrobian H.Q.O et al [2] found 13 vanished testes, we think that this increase in number of absent testis as compare to our study is due to a large sample size of 86 cases consisting of only impalpable testes and absent testes are more common in impalpable variety of UDT.
Taqvi SRH et al. [14], documented 12 prescrotal (pubic) testis which is very close to our result. Kolon TF5 in his article showed the results of Kleintach et al who compiled results on 14,548 testes from several studies and declared 24% testes prescrotal in lacation. In our opinion increase number of prescrotal testes as compare to our study is due to a very large sample size and culture variation as in our culture still many people shy or ignore their genital problem. In our study along with locations of UDT we also stress upon documenting different congenital anomalies associated with UDT. The most common congenital anomaly associated with cryptorchidism is persistent processus vaginalis 90% (Schneck FX23 et al) leading to indirect inguinal hernia and hydrocele. Baker RJ et al states that approximately 85% of UDT have an adjacent inguinal hernia sac. Tanagho EA et al [2] documented 95% patent processes vaginalis during surgery for orchidopexy. In literature clear cut association exist between cryptorchidism and hypospadias. In one study occurrence of hypospadias is up to 9% (Baskin LS et al). In another study conducted on 280 cryptorchid patient’s hypospadias was present in 13 (4.6%) and 8 of 13 were found to have intersex problem . In our study we came across seven patients of hypospadias (7%) so this figure is again same or very close to what described in literature. In the study of Kelalis pp [15-18] 8 out 13 were of intersex problem, and as we mentioned above that the intersex patients were in our exclusion criterion so remaining five cases of hypospadias were very close to our result of 7 hypospadias cases.
Literature also reveals that there are some other congenital anomalies associated with cryptorchidism. These include ARA 4% [Baskin et al, Myelomeningocele, 6 patients were cryptorchid in 23 (26%) patients of myelomeningocele (Kelalis et at). Micro penis 1 in 48 UDT cases (thong et al). According to Atwell et al some 3-9% patient admitted for orchidopexy have major renal anomalies. Kelalis et al revised the compiled results of Kleinteich et al (17.4%), Felton (13%), Grossman and Pirie (12%) about abnormalities of urinary tract. Our study almost confirmed the above as results as follow.
We found 6 (6%) cases of ARA, 2 (2%) cases of myelomeningocele in which one patient also had hydrocephalus. The cause of difference between our study and that of Baskin et al regarding number of cases having myelomeningocele with cryptorchidism is that they looked for cryptorchidism in serial cases of myelomeningocele while our data is reverse. In our study 81% of patients presented to us in age of 4 to 5 years which is too late for development of the degenerative changes in testis to occur. We think that factors responsible this delay are inadequate and as well as inadequately integrated health care system, lack of parents education and socioeconomic problems. We suggest a need for further education of physicians in primary health care services as well as parents.
Conclusion
It is to be concluded that there is no significant difference was noted between mean size and location of undescended testis and the most common location was distal to superficial ring. Future prospective, there is a need to conduct randomized studies using large sample size with multiple study centers in Pakistan are needed to confirm the findings of the present study.
References
1. Kamisawa H, Kojima Y, Hayashi Y. 2008. Evaluation of preoperative testicular volume in Japanese children with unilateral cryptorchidism. Int Urol Nephrol. 40: 977-981. Ref.: https://pubmed.ncbi.nlm.nih.gov/18459063/ DOI: https://doi.org/10.1007/s11255-008-9385-0
2. Kehoe JE, Christman MS. 2017. To ‘Pex or Not to ‘Pex: What to Do for the Contralateral Testis When a Nubbin Is Discovered. Cur Urol Rep. 18: 9.
3. Hussain TS, Akhtar J, Batool T. 2006. Correlation of the size of undescended testis with its locations in vatrious age groups. J Col Phys Surg Pakistan. 16: 594-597. Ref.: https://pubmed.ncbi.nlm.nih.gov/16945233
/ 4. Canning DA. 2017. The Anatomic Findings during Operative Exploration for Non-Palpable Testes: A Prospective Evaluation. J Urol. 198: 202. Ref.: https://pubmed.ncbi.nlm.nih.gov/28618702/ DOI: https://doi.org/10.1016/j.juro.2017.04.062
5. Holland AJ, Nassar N, Schneuer FJ. 2016. Undescended testes: an update. Cur OpinPediatr. 28: 388-394. Ref.: https://pubmed.ncbi.nlm.nih.gov/27138807/ DOI: https://doi.org/10.1097/mop.0000000000000335
6. Meijer RW, Hack WW, Voort- Doedens LM. 2004. Surgical findings in acquired undescended testis. J Pediatr Surg. 39: 1242-1244. Ref.: https://pubmed.ncbi.nlm.nih.gov/15300536/ DOI: https://doi.org/10.1016/j.jpedsurg.2004.04.016
7. Srivastava S, Singh K. 2016. Anatomical correlation of undescended testes. Indian J ClinAnat Physiol. 3: 370-372.
8. Scheck FX, Bellinger MF. 2002. Abnormalities of the testis and scrotum and their surgical management. In: Walsh PC, Retik AB, Vaughan EDJr, Wein AJ, editors. Campbell’s Urology. 8th ed. Philadelphia: W.B. Saunders. 2002: 2353-2394.
9. Taqvi SRH, Akhtar J, Batool T. 2006. Correlation of the size of undescended testis with its location in various age groups. J Coll Physicians Surg Pak. 16: 594-597. Ref.: https://pubmed.ncbi.nlm.nih.gov/16945233/
10. Favorito LA, Klojda CA, Sampaio FJ. 2004. Congenital absence of the testis in human fetuses and in cryptorchid patients. Int J Urol. 11: 1110-1113. Ref.: https://pubmed.ncbi.nlm.nih.gov/15663684/ DOI: https://doi.org/10.1111/j.1442-2042.2004.00952.x
11. Dogra VS. 2004. Cryptorchidism. eMedicine. 1-6.
12. Kelalis PP, King LR, Belman AJ. 1992. Cryptorchidism. Clinical pediatric urology. 1050-1078.
13. Scheck FX, Bellinger MF. 2002. Abnormalities of the testis and scrotum and their surgical management. In: Walsh PC, Retik AB, Vaughan EDJr, Wein AJ, editors. Campbell’s Urology. 8th ed. Philadelphia: W.B. Saunders. 2353-2394.
14. Mesrobian HGO, Chassaignac JM, Laud PW. The presence or absence of an impalpable testis can be p redicted from clinical observations alone.
15. Favorito LA, Klojda CA, Sampaio FJ. 2004. Congenital absence of the testis in human fetuses and in cryptorchid patients. Int J Urol. 11: 1110-1113. Ref.: https://pubmed.ncbi.nlm.nih.gov/15663684/ DOI: https://doi.org/10.1111/j.1442-2042.2004.00952.x
16. Martini FH, Timmsons MJ. 1997. Human Anatomy. 2nd ed. New Jersey: Prentice Hall.
17. Tews DS, Goebel HH. 1997. Apoptosis-related proteins in skeletal muscle fibers of spinal muscular atrophy. J Neuropathol Exp Neurol. 56: 150-156. Ref.: https://pubmed.ncbi.nlm.nih.gov/9034368/ DOI: https://doi.org/10.1097/00005072-199702000-00005
18. Cryptorchidism. 1992. In: Kelalis PP, King LR, Belman AJ, editors. Clinical pediatric urology. 3rd ed. Philadelphia: W.B. Saunders. 1050-1078.




















