Indexing & Abstracting
Full Text
Case ReportDOI Number : 10.36811/jcri.2021.110020Article Views : 66Article Downloads : 43
Improvement in CT findings and Inflammatory Parameters during Recovery in a Covid-19 patient: A Case Report
Yasin Kilic, Hakan Usta, Ferhat Borulu and Bilgehan Erkut*
Atatürk University, Medical Faculty, Department of Cardiovascular Surgery, Erzurum, Turkey
*Corresponding Author: Bilgehan Erkut, Atatürk University Medical Faculty, Department of Cardiovascular Surgery, Erzurum, Turkey, Tel: 0090533 7451006, 0090442 3448899; Email: bilgehanerkut@yahoo.com; bilgehan.erkut@gmail.com
Article Information
Aritcle Type: Case Report
Citation: Yasin Kilic, Hakan Usta, Ferhat Borulu, et al. 2021. Unilateral pneumocephalus: A rare case. J Case Rept Img. 3: 10-15.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2021; Yasin Kilic
Publication history:
Received date: 28 April, 2021Accepted date: 01 May, 2021
Published date: 05 May, 2021
Abstract
The COVID-19 infection from China has turned into a worldwide epidemic and the early diagnosis, control and limitation of the disease plays an important role in affecting the health systems of the world countries and the prognosis related to patients. In COVID-19 patients, the first 2 weeks is usually a viral and inflammatory process. In these patients, after the deterioration in radiological and inflammatory markers occurs, the recovery period begins in the 3rd week and after. In this case report, we presented the changes in the radiological and inflammatory parameters during the recovery phase of the disease stage parameters in a 44-year-old man COVID-19 disease patient who was followed up by the cardiovascular surgery clinic due to deep venous insufficiency.
Keyword: Covid-19 Infections; Inflammatory Parameter; Lung Involvement; Recovery: Crazy-Paving Pattern
Introduction
A respiratory-associated pneumonia of unknown cause emerged in Wuhan, China, and spread throughout the world within months [1-3]. A new corona-virus SARS-COV 2 (COVID-19) agent was identified in the respiratory tract of the patients and defined as the cause This COVID-19 agent was very potent in terms of its ability to be transmitted from person to person, and thus infected thousands of people in a short time [4,5].
Due to the similarity of COVID-19 to the flu in the early stages, it is difficult to distinguish between them, especially during the winter and spring months. This condition is critical for the early diagnosis of the disease and associated with it to improve the prognosis of patients. Changes in some inflammatory and hematological parameters and computed tomography findings in COVID-19 patients can provide information about the diagnosis and severity of the disease. Combining imaging findings (bilateral ground glass opacities, crazy-paving pattern, consolidation of the peripheral lung, gradual resolution of consolidation) with clinical and laboratory findings can aid in the early diagnosis of COVID 19 [6].
In this presentation, where we would like to show whether the improvement in clinical and laboratory findings accompany the computed tomography findings during the healing process of our patient diagnosed with COVID-19 infection, and we also emphasized the importance of early diagnosis markers.
Case Report
The 44-year-old man, who was followed up in the cardiovascular surgery outpatient clinic due to deep venous insufficiency, was admitted to the hospital with the complaints of moderate fever, sneeze, nasal congestion, weakness, head and throat pain, cough, fatigue and chest-back pain after a wedding ceremony. Although his complaints resemble flu infection, the laboratory, radiological and PCR tests were requested for early diagnosis of COVID-19 infection. The results of the patient's laboratory tests are shown in (Table 1). In addition, 24 hours later, the patient's COVID-19 PCR test came as positive. After PCR (+); D-Dimer, fibrinogen and ferritin were requested to follow the thrombotic process associated with COVID-19 (Table 1). After the diagnosis of COVID-19 infection, the oxygen saturation values of the patient remained between 85% - 88%, and he was hospitalized. The telecardiography showed infiltration in the bilateral lower and sub-pleural regions of the lung (Figure 1A). On thoracic computed tomography, there was ground-glass opacity showing bilateral lung involvement (Figure 1B). In addition to oxygen therapy, the drug protocol accepted by our hospital for COVID-19 infections has been initiated. Enoxaparine, antiviral agent (favipiravir), hydroxyl-chloroquine, empirical antibacterial drug (levofloxacin) and methyl-prednisolone for lung involvement were started to be given to the patient. The patient was closely observed for any thrombotic and hyper-coagulability (for cerebral, pulmonary, vascular and cardiac thrombosis). Although neutrophil count and percentage, WBC, LDH and platelet count did not change in the second week, the increase in ferritin, fibrinogen, D-Dimer, CRP, sedimentation, serum procalcitonin levels and the decrease in lymphocyte count and percentage continued according to the first week results. At the end of the second week, oxygen saturations were within normal limits (90% - 92%), and thrombotic and infection markers also did not increase. The patient was discharged. Bilateral crazy-paving pattern and consolidation was seen in computed tomography performed before discharge (Figure 2). Despite this appearance in her lungs, the patient had no breathing problems and her clinic was stable. The PCR test performed at this time was negative. From the 3rd week to the end of the 4th week, a significant improvement was observed in all infection parameters, inflammatory markers and tests showing thrombotic tendency (Table 2).
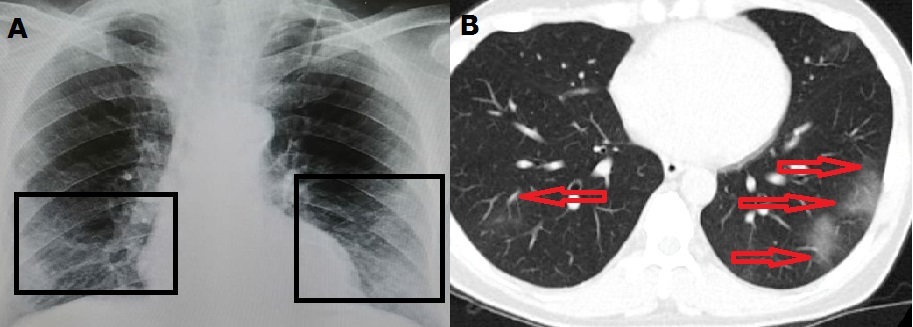
Figure 1A: Chest roentgenography shows bilateral infiltrates at the initial stage in our patient with COVID-19 infection (black frame).
Figure 1B: Chest CT findings of corona-virus disease 2019. Trans-axial images show bilaterally ground-glass opacity (day 3 from symptom onset) (red arrows).
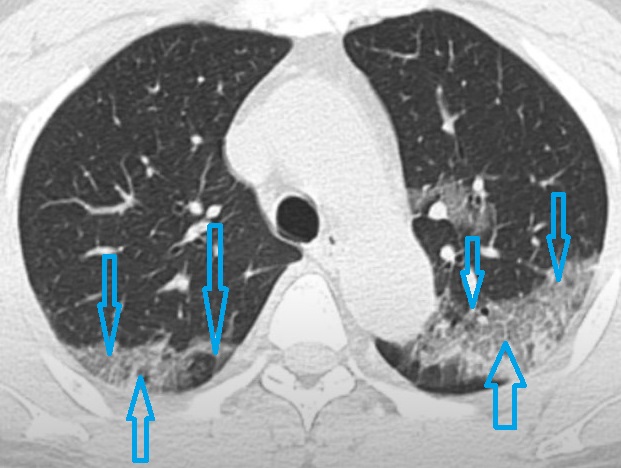
Figure 2: Scan obtained on day 15 from symptom onset shows crazy-paving pattern and consolidation (blue arrows).
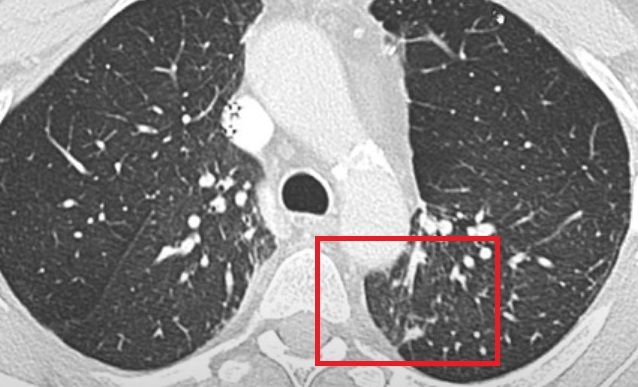
Figure 3: CT scan obtained on day 30 from symptom onset shows continued resolution of consolidation without crazy-paving pattern (Parenchymal bands) (red frame).
|
Table1: The laboratory results in the initial stage of the disease. |
|
|
Parameters |
At the beginning |
|
CRP (mg/dL) |
41 (<3,11) |
|
Sedimentation (mm/h) |
33 (0-20) |
|
Serum procalcitonin (ng/mL) |
11 (0,5-2) |
|
Neutrophil count (µ/L) |
3.87 (1,91-7,61) |
|
Neutrophil (%) |
66 (40-71) |
|
LDH (U/L) |
188 (90-250) |
|
WBC (µ/L) |
4,0.103 (3,9–10,8.103) |
|
Lymphocyte count (µL) |
0.87.103 (1,16–3,61.103) |
|
Lymphocyte (%) |
16.6 (18-47) |
|
Platelet count (µL) |
126.103 (145-345.103) |
|
ALT (10-40 (U/L) |
71 |
|
AST (15-42 (U/L) |
77 |
|
After PCR (+) Ferritin (ng/mL) Fibrinogen (mg/dL) D-Dimer (ng/mL) |
388 (23.9-336.2) 502 (245-400) 455 (0-500) |
|
Oxygen saturation (%)
|
89-93 |
|
Table 2: Changes in laboratory parameters by the end of the 4th week. |
|||
|
Parameters |
Second weeks |
Third weeks |
At the end of the 4th week |
|
CRP (mg/dL) (<3,11) |
66 |
36 |
7 |
|
Sedimentation (mm/h) (0-20) |
59 |
22 |
11 |
|
Serum procalcitonin (ng/mL) (0,5-2) |
21 |
9 |
1.7 |
|
WBC (µ/L) (3,9–10,8.103) |
4,0.103 |
4,7.103 |
5,9.103 |
|
Lymphocyte count (µL) (1,16–3,61.103) |
0.66.103 |
0,92.103 |
2,5.103 |
|
Lymphocyte (%) (18-47) |
14.1 |
23.7 |
29.1 |
|
ALT (U/L) (10-40) |
145 |
116 |
61 |
|
AST (U/L) (15-42) |
178 |
133 |
59 |
|
After PCR (+) Ferritin (ng/mL)
Fibrinogen (mg/dL) D-Dimer (ng/mL) |
466 (23.9-336.2) 567 (245-400) 501 (0-500) |
402 460 432 |
301 299 382 |
|
Oxygen saturation (%) |
90-92 |
91-94 |
95 |
The patient was followed up without being hospitalized. The oxygen values of the patient, who was called to the hospital daily, did not decrease. Except for the tomography performed on the first days and the 15th days, the patient's general condition was good and the oxygen values were normal, so the tomography was not performed until the 30th day. Computed tomography was performed again on the 30th day of the patient, who was in the recovery period, and a resolution of consolidation without crazy-paving pattern (Parenchymal bands) was determined (Figure 3). At the end of the first month, all laboratory parameters returned to normal and radiological examinations improved, so the patient was deemed recovered and was removed from follow-up.
Discussion
First emerging diagnostic criteria in COVID-19 patients; airway contact with a sick person, fever and respiratory symptoms, radiological findings, decreased white blood cell count or lymphocyte count, polymerase chain reaction positivity. After this first stage, patients are followed in terms of respiratory characteristics and thrombotic process. Laboratory and clinical findings are closely monitored. Drug treatment procedures are applied according to accepted treatment protocols. After repeating the PCR test, the patient is discharged if the following criteria are met: the patient will have a fever for more than 3 days, respiratory symptoms will improve significantly, there will be an improvement in radiological abnormalities on chest radiographs or chest CT scans, and two consecutive negative COVID-19 PCR tests will be seen. Our patient probably got the virus after a contact, spread to the respiratory tract and lungs, symptoms appeared, COVID-19 was diagnosed with the PCR test with the examinations performed, and treatment was started. Pulmonary function improved without thrombotic complications and thoracic CT showed a normal course and good prognosis.
From the recently published literature, typical radiologic images of COVID-19 demonstrated clear destruction of the pulmonary parenchyma, including interstitial inflammation and extensive consolidation, similar to the previously reported corona-virus infection. Lung involvement findings in CT follow the process from the initial stage of the disease to the recovery stage and include some findings. The most common CT findings four stages were identified from the onset of initial symptoms. The early initial stage (0-4 days); ground-glass opacities (stage I), progressive stage (5-8 days); crazy-paving pattern and consolidation (stage II), peak stage (10-13 days); consolidation was the main finding with an obviously decreased ratio of crazy-paving pattern (stage III), and absorption stage (≥14 days) gradual resolution of consolidation without crazy-paving pattern (stage IV) [2,7]. Overall, bilateral lung involvement is sub-pleural lesions and more common than central lung lesions in the lower lobes. While lung CT findings are divided according to stages, lung scoring can also be made according to the involvement rates in the lobes. Each of the five lung lobes was visually scored on a scale from 0 to 5; 0 showed no involvement and 5 showed more than 75% involvement. The total CT score was determined as the sum of lung involvement, ranging from 0 (no involvement) to 25 (maximum involvement). In the last stage, there is a significant decrease in lung scoring in CT [2,7]. In the tomography of our patient, the first 2 stage findings were seen (high CT score; 4 lobe involvement). Since the oxygen saturation of the patient did not decrease excessively and even increased after the 2nd week, we had the computed tomography performed on the 30th day at the end of the recovery period. We wanted to see the change in the lungs when the general condition of the patient improved and the oxygen saturation increased. We determined the absorption phase (resolution of consolidation without crazy-paving pattern) at the end of the first month (low CT score; 2 lobes involvement).
The important point is to be diagnosed at the earliest stage. Because the disease has put serious strains on the medical system, and in light of short and limited medical resources, it has become crucial to identify COVID-19 patients at an early stage, which will facilitate control of the outbreak and improve patients' prognosis. When evaluating early markers of the disease, it has become important to diagnose patients early with laboratory tests before CT is performed. Laboratory tests compatible with CT strengthen the diagnosis. And by following these 2 parameters, the patients are moved to the recovery period. Many parameters can be used in terms of early indicator. In particular, an increase in CRP, sediment and procalcitonin levels, fibrinogen, ferritin and D-Dimer, a decrease in lymphocyte count and percentage at an early stage of the disease are important in predicting the severity of the disease and making an early diagnosis. The improvement of these parameters during the recovery process is also important in terms of the course of COVID-19. In the latest diagnostic and treatment guidelines [5,8], changes in these parameters during the first week can be considered as an early warning of critical illness. When all these early markers are accompanied by CT findings and increasing CT score, if the oxygen saturations of the patients are also affected, it is effective in making the definitive diagnosis of COVID-19.
In conclusion, this case has shown that some laboratory parameters in the early stages of the disease can be helpful in diagnosis and may be important in monitoring the prognosis of the disease. In addition, it was observed that the improvement in the laboratory tests accompanied the recovery process in parallel with the CT findings.
References
1. WHO Novel coronavirus. China. 2020.
2. Tan W, Zhao X, Ma X, et al. 2020. Notes from the field: a novel coronavirus genome identified in a cluster of pneumonia cases - Wuhan, China 2019-2020. China CDC Weekly. 2: 61-62.
3. Xu X, Chen P, Wang J, et al. 2020. Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission. Sci China Life Sci. 63: 457-460. Ref.: https://pubmed.ncbi.nlm.nih.gov/32009228/ DOI: 10.1007/s11427-020-1637-5
4. Lu R, Zhao X, Li J, et al. 2020. Genomic characterization and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 395: 565-574. Ref.: https://pubmed.ncbi.nlm.nih.gov/32007145/ DOI: 10.1016/S0140-6736(20)30251-8
5. Li Q, Guan X, Wu P, et al. 2020. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N Engl J Med. 382: 1199-1207. Ref.: https://pubmed.ncbi.nlm.nih.gov/31995857/ DOI: 10.1056/NEJMoa2001316
6. Pan F, Ye T, Sun P, et al. 2020. Time Course of Lung Changes at Chest CT during Recovery from Coronavirus Disease 2019 (COVID-19). Radiology. 295: 715-721. Ref.: https://pubmed.ncbi.nlm.nih.gov/32053470/ DOI: 10.1148/radiol.2020200370
7. Tan C, Huang Y, Shi F, et al. 2020. C-reactive protein correlates with computed tomographic findings and predicts severe COVID-19 early. J Med Virol. 92: 856-862. Ref.: https://pubmed.ncbi.nlm.nih.gov/32281668/ DOI: 10.1002/jmv.25871
8. Ruan Q, Yang K, Wang W, et al. 2020. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 46: 846-848. Ref.: https://pubmed.ncbi.nlm.nih.gov/32125452/ DOI: 10.1007/s00134-020-05991-x




















