Indexing & Abstracting
Full Text
Case ReportDOI Number : 10.36811/jcri.2019.110005Article Views : 1491Article Downloads : 25
Dermoscopy of naevus spilus
Niema Aqil*, Sara Elloudi, Aicha Nassiri, Salim Gallouj, Hanane Baybay and Fatima Zahra Mernissi
Department of dermatology, Hassan II University Hospital Center, Fes, Morocco
*Corresponding author: Niema Aqil, department of dermatology, Hassan II University Hospital Center, Fes, Morocco, Email: niemaaqil90@gmail.com
Article Information
Aritcle Type: Case Report
Citation: Niema Aqil, Sara Elloudi, Aicha Nassiri, et al. 2019. Dermoscopy of naevus spilus. J Case Rept Img. 1: 37-39.
Copyright:This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2019; Niema Aqil
Publication history:
Received date: 20 February, 2019Accepted date: 07 April, 2019
Published date: 08 March, 2019
Abstract:
Nevus spilus defines as cafe-au-lait macule with superimposed maculopapular speckles. Although the cafe-au-lait macule often presents at birth, the darker pigmented speckles increase in number and size during a period of several years. The need for close follow-up of patients with NS is underlined by reports of several cases of cutaneous melanoma developing within such lesions. Hence the importance of recognizing its typical dermoscopic aspects.
Keywords: Nevus Spilus; Dermoscopy; Typical aspects
Introduction
Nevus spilus (NS) is clinically characterised by multiple pigmented macules or papules within a pigmented patch. It is called various names: NS, speckled lentiginous nevus, zosteriform lentiginous nevus, and spots on a spot [1]. It may be congenital or acquired. It is usually benign and usually appears in childhood. In most cases, it appears clinically as a small, isolated lesion; although in some cases occur on larger areas of the body [1]. Because of the risk of transformation into melanoma, regular skin examination with the use of dermoscopy is strongly advised [2]. Our aim was to describe dermoscopic patterns of NS in a research-based case study.
Material and Methods
We collected 10 patients with nevus spilus, and we performed a dermoscopic analysis over a period of two years in the dermatology department of the Hassan II University Hospital Center. In all cases, the diagnosis of the NS was based on clinical and dermoscopic images, with none of the patients having undergone any surgical procedures.
Results
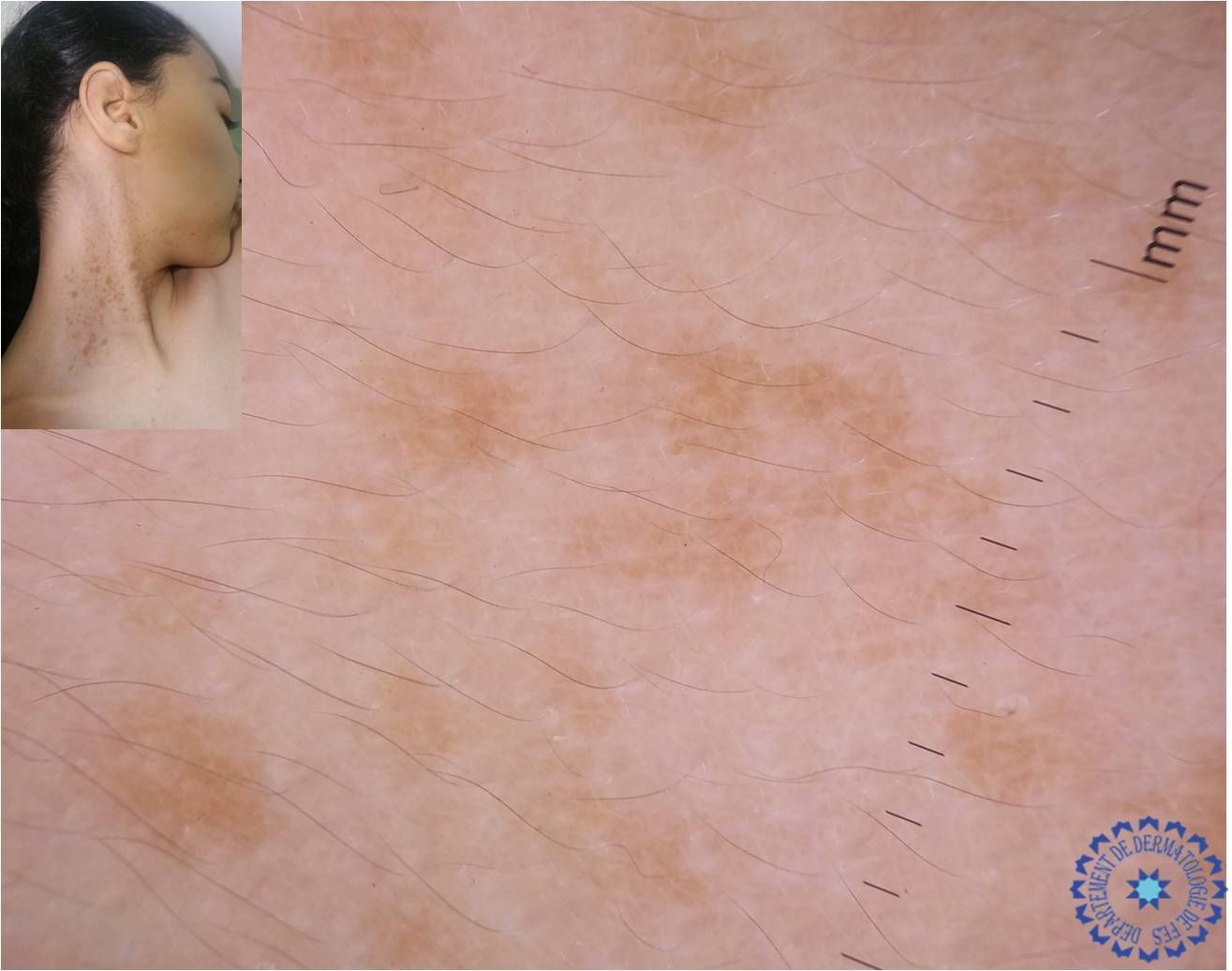
We collected 10 patients with a nevus spilus with an average age of 29 years, 8 female and 2 male, the location was in the face of a patient, the neck in a patient, the abdomen in 2 patients, the back in 3 patients, one patient's feet, and one patient's axilla, 70% of patients had these lesions from birth and 30% in adulthood. Examination with a dermoscope had objectified a homogeneous reticular pattern on a homogeneous clear pigmentation in all the patients. (Figure 1-5) Dermoscopy revealed in a single patient, a reticular pattern mixed with a dots pattern. (Figure 6) No cases of atypical NS were noted.
Figure 1-5: Homogeneous reticular pattern on a homogeneous clear pigmentation.
Figure 1:
Figure 2:
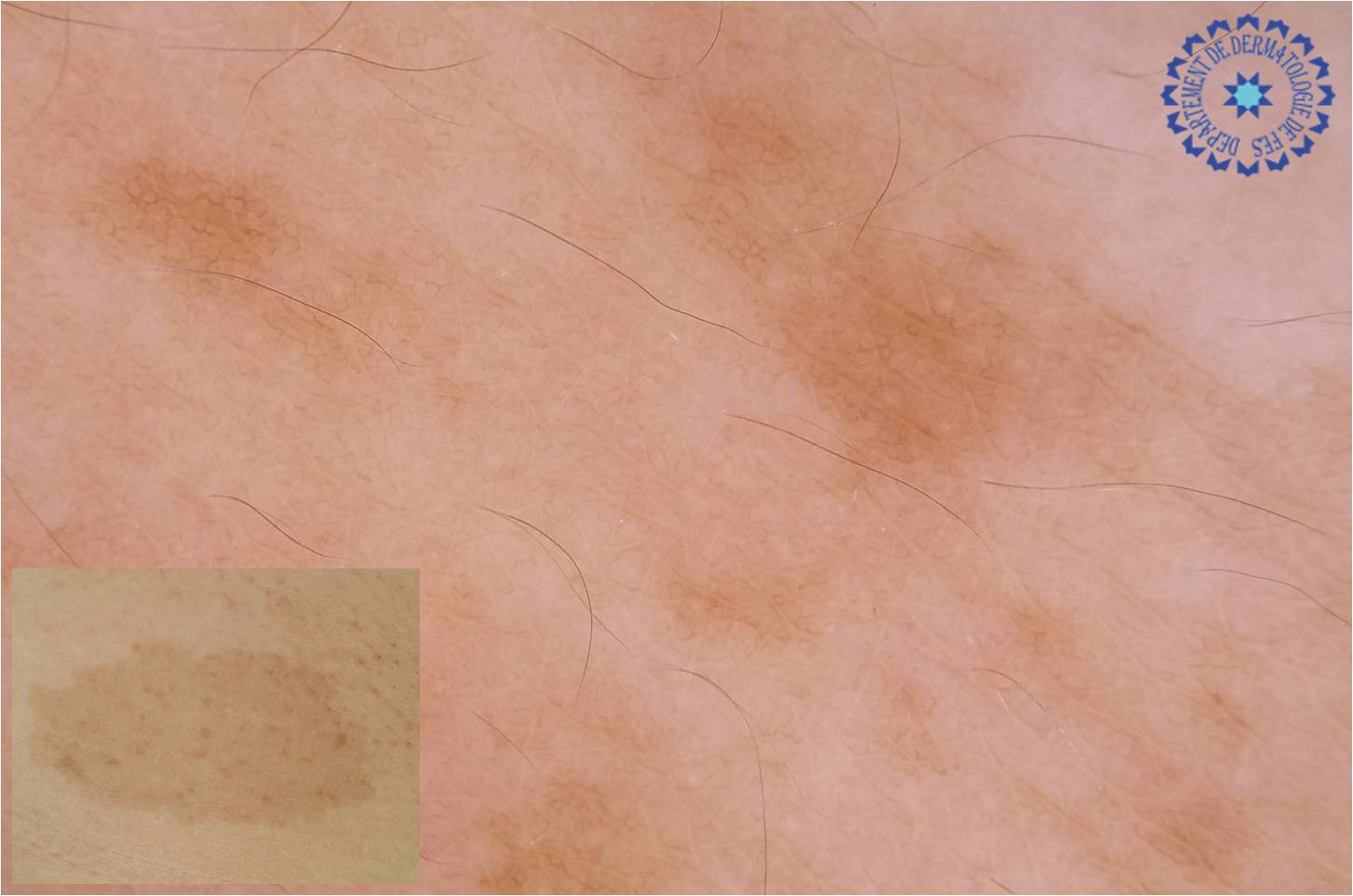
Figure 3:

Figure 4:

Figure 5: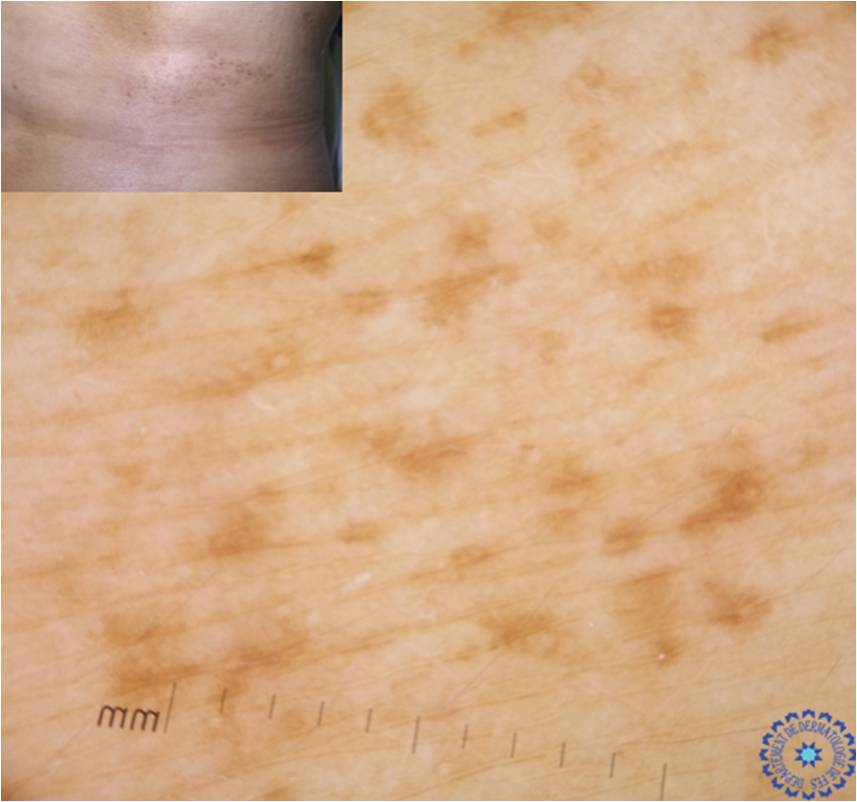
Figure 6: Reticular pattern mixed with a dots pattern.
Discussion
NS is a rare dermatologic entity, found in 2.8% of the pigmented lesions examined [3]. NS usually appears during infancy but may also appear later in life, typically in the intensive growth stages. Anatomically, it is most frequently located on the trunk, the lower and upper extremities, and the head, as in our patients [4]. NS is defined as a cafe-au-lait macula with superimposed pigmented maculopapular lesions [2]. NS dermoscopy reveals darker brown areas with a reticuloglobular pattern. The background is usually light brown and reticular. In typical cases of NS, dermoscopy illustrates a reticular pattern with absence of atypia. In suspected cases of NS, it reveals an atypical aspect of hyperpigmented area with an irregular pattern [4]. Thus, dermoscopy is recommended as a diagnostic tool in the monitoring and surveillance of any suspicious lesion of progression to melanoma. The risk of melanoma appearing in NS is low, but self-examination, clinical observation, serial photographic imaging, and dermoscopic archives remain the mainstay of NS management.
Conclusion
Because of the risk of transformation into melanoma, NS requires regular clinical and dermoscopic monitoring, and skin biopsy whenever there is a change in the clinical or dermoscopic appearance. Hence the importance of recognizing its typical dermoscopic aspects.
Consent for publication
Written informed consent was obtained from the patients for publication of this study and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Fernandez-Flores A. 2012. Eponyms, morphology, and pathogenesis of some less mentioned types of melanocytic nevi. Am J Dermatopathol. 34: 607-618. [Ref.]
- Haenssle HA, Kaune KM, Buhl T, et al. 2009. Melanoma arising in segmental nevus spilus: detection by sequential digital dermatoscopy. J Am Acad Dermatol. 61: 337-341. [Ref.]
- Menon K, Dusza SW, Marghoob AA, et al. 2006. Classification and prevalence of pigmented lesions in patients with total-body photographs at high risk of developing melanoma. J Cutan Med Surg. 10: 85-91. [Ref.]
- Manganoni AM, Pavoni L, Farisoglio C, et al. 2012. Report of 27 cases of naevus spilus in 2134 patients with melanoma: is naevus spilus a risk marker of cutaneous melanoma? J Eur Acad Dermatol Venereol. 26: 129-130. [Ref.]




















