Indexing & Abstracting
Full Text
Case ReportDOI Number : 10.36811/jcri.2019.110001Article Views : 2161Article Downloads : 24
Pediatric Zygomaticomaxillary complex fracture with retroorbital hematoma. A case report
Mohamed Ashraf Elkahwagi1 and Ahmed Ali El-degwi2*
1Assistant lecturer, MD of ORL, HNS Mansoura University, Egypt
2Professor of ORL, HNS Mansoura University, Egypt
*Corresponding author: Ahmed Ali El-degwi, Professor of ORL, HNS Mansoura University Egypt, Email: adegwi57@yahoo.com
Article Information
Aritcle Type: Case Report
Citation: Elkahwagi MA, Eldegwi AA. 2019. Pediatric Zygomaticomaxillary complex fracture with retroorbital hematoma. A case report. J Case Rept Img. 1: 01-08.
Copyright:This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2019; Mohamed AE
Publication history:
Received date: 27 December, 2018Accepted date: 08 January, 2019
Published date: 09 January, 2019
Abstract:
Objective: this article describes a case of pediatric orbital fracture emphasizing on the important complications that need urgent intervention.
Methods: a case report with description of the case with zygomatic and orbital fracture with serious complications as retrorbital hematoma and inferior rectus entrapment. In addition, we described the urgent intervention done for the case.
Results:optimum timing of the management was the key for the case. Immediate lateral canthotomy and inferior cantholysis in addition to entrapped muscle release from the fracture with reduction and fixation of the fracture lines led to excellent and satisfactory results.
Conclusion: careful examination and management of pediatric orbital fractures represent the cornerstone for this entity of maxillofacial injury. Retrorbital hematoma and inferior rectus muscle entrapment are raer but serious complications of pediatric zygomatic fractures and they need immediate management.
Introduction
Zygomaticomaxillary complex fractures are one of the most common maxillofacial injuries because of zygomatic projection off the facial skeleton [1]. Pediatric facial trauma and fractures is different from those in the adults. The main difference is that pediatric fractures are much less common than adult ones accounting for less than 15% of all facial fractures, with a much decrease in the incidence below age of 6 years [2]. In addition, pediatric patients differ in anatomical, developmental and physiological point of view from adults, resulting in changes in the epidemiology, diagnosis and subsequent management [3]. However, the high ratio of cranial mass to body of children, which contributes to an increased susceptibility for maxillofacial trauma also leads to a predisposition frontocranial injury [4].
The cranium to face ratio of the pediatric patient is 8:1 compared with 2:1 in adults. This increased cranial to face ratio decreases the risk of maxillofacial injury versus skull injury [4]. Incomplete aeration of the maxillary sinus, incompletely fused suture lines, thicker periosteum and increased soft tissue padding over the malar eminence are features of the pediatric orbital region [5].
When excessive force is applied to the pediatric globe or orbital rim, a linear fracture (trapdoor) pattern develops. The fractured segment of bone can displace into the underlying maxillary sinus while still attached [5]. The increased volume of the orbital cavity is in turn the major cause for posttraumatic enophthalmos and hypoglobus. Furthermore, fractures in certain regions of the orbit, cavity is in turn the major cause for posttraumatic enophthalmos and hypoglobus [6].
Use of multiple specialty approach in the evaluation and treatment of pediatric patients with orbit fractures is of great importance. A complete physical examination may be limited by cooperation and physical examination findings may be subtler and easily missed [7]. Having the imaging results before examining the patient gives the examining surgeon some idea of what injuries the child has experienced [3]. Before addressing the definitive treatment of pediatric facial trauma, initial management should focus on the airway, breathing, circulation support. The development of shock in pediatric population is rapid so great attention for support should be done [3]. Treatment protocols that have been largely established in the adult population may not be applicable to the pediatric population [7].
Great debate is still present regarding the management of zygomatic fractures, including number of approaches and points of fixation and the decision to explore the orbital floor [8]. Although indications for operative intervention in pediatric orbital fractures remain the object of debate, some indications exist in the acute phase. Orbital floor fractures that result in extraoccular muscle entrapment or those which are significant enough to result in enophthalmos are indication for surgery. Extraoccular muscle entrapment is typically caused by trapdoor fractures, in which the floor hinges down with the injury and returns to a normal position. In these cases, surgical intervention within the first few hours [9]. Orbital floor fractures which is type of orbital blow out fractures are the most common type of fracture to require repair, whereas orbital roof fractures are the least likely to require intervention [7].
Management of zygomaticomaxillary complex (ZMC) fractures should be based on injury patterns and not on training background [8]. Significantly displaced and/or comminuted fractures are indications for internal fixation. Displaced non-comminuted fractures are adequately stabilized with microplates placed with care taken to avoid screw transfixion of the maxillary tooth buds [3].
A pediatric orbital fracture classification system was devised and includes three types of orbital fractures. Type 1 fractures include pure orbital fractures which are limited to the orbit without extension to adjacent bones. Type 2 (craniofacial fractures) are oblique fractures ex-tending from the skull into the orbital roof and face. Type 3 fractures (the common fracture patterns), the orbital fracture extends to the surrounding bones. Type 3 fractures are subdivided into 3a, impure blowout fractures; type 3b, zygomaticomaxillary fractures; type 3c, naso-orbitoethmoid fractures; and type 3d, other fracture patterns [9]. The terms “pure” and “impure” blowout fractures have been used to differentiate between fractures with and without orbital rim involvement [9].
The main goal of blowout fracture surgery is to reconstruct the contours of the bony orbit and thus to reestablish the normal orbital volume [10]. The Duke craniomaxillofacial criterion for orbital floor exploration was 1 cm or more of estimated zygomaticomaxillary complex displacement [11]. A volume increase or decrease by 20 percent or greater is a reasonable criterion for exploring the orbital floor in the setting of zygomaticomaxillary complex associated floor fractures [11].
Pediatric orbit fractures tend to be associated with more severe comorbid injury because of the great amount of force needed to overcome the elasticity of developing bone [1]. These fractures represent a more diverse spectrum of injuries than those seen in the adult population [15]. The treatment of pediatric facial fractures can be challenging, stimulating, and occasionally frustrating, especially for those practitioners who only rarely manage these injuries [12]. Non-operative management is advocated for minimally displaced or greenstick mid-face fractures, particularly in the younger child [12].
The aim of this article is to describe a case with pediatric orbital fracture with more than one indication for immediate surgical interference. The presentation emphasizes the importance of careful assessment of orbital fracture in pediatrics as the proper management can save the child’s eye.
The case
Six years old girl presented to our emergency room at Mansoura emergency hospital, a tertiary referral center for trauma cases, with a history of being kicked by a hoarse in the left side of her face 3 hours before presentation. Examination showed Left side C shaped cut wound surrounding her left eye with marked edema and proptosis of the left eye. Edema and swelling of the whole left side of the face made assessment of the bone difficult (Figure 1).
Computed tomography (CT) facial was done showing left side orbital fracture type 3. Zygomaticomaxillary complex fracture with bone chip in the lateral orbital wall in the orbit was present. Left side proptosis was noticeable in the CT with soft tissue density in the retroorbital region. This was suggestive of retroorbital hematoma. Inferior rectus entrapment in a trapdoor inferior orbital fracture was present (Figure 2).
Urgent ophthalmic consultation was done revealing: Lt dilated irreactive pupil, increasing optic disc pallor, Elevated digital intraoccular pressure and Mild impairment of the upward movement of the eye on forced duction test performed under anesthesia.
The procedure
Immediated intraoperative admission was done: Lateral canthotomy and inferior cantholysis was done to drain the retroorbital hematoma and decompress the optic nerve. Reduction of the zygomatic fracture and fixation by 2-point stabilization (zygomaticofrontal suture & inferior orbital wall) (Figure 3,4) throught the cut wound and subciliary approach. Removal of the bone chip that was violating the lateral orbital septum was done. Release of the entrapped inferior rectus from the fracture was also done.
Follow up
Postoperative Daily ophthalmic follow up revealed: decreasing temporal disc pallor, gradual improvement of the pupil reaction till regained normal condition after 2 weeks, near equal digital occular pressure, improving periobital edema and ecchymosis and normal occular motility in all directions of gaze (Figure 5).
Follow up for the cosmotic appearance was done till 6 months postoperatively with highly satisfactory results. The plates were removed 1 year postoperatively through the previous incisions not to affect the facial growth (Figure 6).
Figure 1: Preoperative picture showing the cut wound and the facial swelling.

Figure 2: Preoperative CT a. anteroposterio view of the 3D CT facial. B. lateral view. C. axial cuts showing the zygomaticosphenoid fracture and retroorbital hematoma.

Figure 3: postoperative CT a. anteroposterio view of the 3D CT facial. B. lateral view. C. axial cuts showing the repair of the zygomaticosphenoid suture.

Figure 4: Postoperative CT a. axial cut b. 3D cut showing the optimal reduction of the inferior orbital rim.
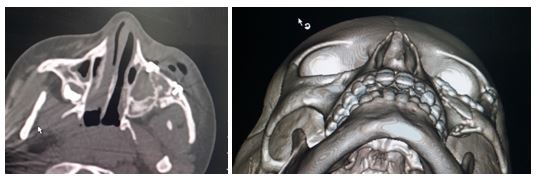
Figure 5: 2 weeks postoperative photo.

Figure 6: 6 months postoperative photoes.

Discussion
The zygoma defines the anterior and lateral projection of the face and makes up the inferior and lateral surfaces of the orbit. It relates to the facial skeleton at four points. The zygomatico-maxillary suture, the fronto-zygomatic suture, the zygomatico-temporal and the zygomatico-sphenoid suture make up the four legs of this complex. Proper alignment of this suture and the lateral orbital wall is paramount to achieve adequate reduction [13,14].
Pediatric ZMC fractures have special consideration among maxillofacial fractures with majority of the cases improve by conservative measures [13]. The literature supports non-operative management of minimally or non-displaced pediatric zygomatic fractures [15]. When facial fractures are present and require intervention, the optimal timing of repair for a child must take into account the rapidity with which most children will heal a closed injury [3]. Therefore, we introduce this case to define the absolute indications for surgical intervention in pediatric orbital fractures in addition to the importance of the intervention timing. Orbital complications have higher incidence in pediatric Zygomaticomaxillary fractures. Occular muscle entrapment, Retrorbital hematoma, traumatic or compressive Optic nerve neuropathy and Orbital emphysema can occur as a result of severe orbital trauma [16].
Lower lid malposition deformities represent a broad spectrum of complications that vary in cosmetic and functional significance. The most commonly encountered malposition deformities include ectropion, lower lid retraction Lower lid edema and visible or hypertrophic scars can also occur either from the trauma itself or as a result of intervention through lid incisions like sub-ciliary or sub-tarsal incisions [17].
In addition to enophthalmos, orbital fractures may be followed by persistent diplopia. Diplopia is caused by inhibited function of extraocular muscles due to swelling, fibrosis, entrapment, or by nerve injury. Visual function may also be permanently affected by concomitant traumatic injury to the optic nerve or eye bulb [6].
Clinical findings of a pediatric orbital fracture include enophthalmos, periorbital ecchymosis, subcutaneous crepitus, and subconjunctival hemorrhage. Signs of entrapment indicative of blow-out fracture include horizontal or vertical diplopia, restricted eye movements, nausea, vomiting, and severe pain with eye movements. Orbital floor fractures may involve the infraorbital nerve. This would manifest as decreased sensation on the ipsilateral side to the upper cheek, upper palate, and upper lip. Acute exophthalmos may result from periorbital edema, hemorrhage, or inflammation [16].
It is well described that muscle entrapment in the pediatric orbital fracture constitutes a “surgical emergency” and must be addressed at the earliest possible time to prevent extraocular muscle dysfunction [9]. Entrapment of the soft tissue (inferior rectusmuscle, fat, or connective tissue) causes ischemia. This is worsened with delayed intervention. So, this needs surgical interference and correction by release of the muscle from the fracture line and reduction of the fracture [16].
There are few papers in the literature in the last decade concerning trapdoor fractures, all of which recommend early treatment to release tissues entrapped in the fracture line [5]. Although rare, orbital floor trapdoor fractures are considered to represent a surgical emergency and need urgent exploration and release of the entrapped periorbital tissues and/or muscle [5].
Presence of retroorbital hematoma in cases of orbital fracture is an urgent condition especially if not associated with medial and inferior orbital wall fracture: this can lead to orbital compartmental syndrome and irreversible visual loss withing 1-2 hours if not urgently managed. On the other hand, Immediated reduction of the Zygomatic fracture in absence of retrorbital hematoma is controversial also for fear of postoperative compartmental syndrome and compressive optic neuropathy. In addition, Presence of severe orbital emphysema with vision affection is an indication for drainage or aspiration to save the vision [13].
Optic canal fracture and traumatic optic neuropathy is a serious complication: This can lead to irreversible visual loss and the treatment is controversial [1]. The most accepted measures are high dose corticosteroids, lateral canthotomy to decrease the intraoccular pressure and exploration of the optic canal with neurosurgical consultation [9].
The dilemma in the case presented was that she had more than one indication for urgent surgical interference. Early management prevented the irreversible visual loss complication that would have occurred if the management was delayed.
Conclusion
Pediatric orbital and zygomatic fractures should have special consideration among maxillofacial injuries. Accurate ophthalmic examination in zygomatico-maxillary fractures is mandatory to exclude orbital complications that need immediate management. Presence of retroorbital hematoma with proptosis is an urgent condition that needs immediate intervention to relieve the compression inside the orbit on the optic nerve. Occular muscle entrapment is another emergency that needs surgical release of the entrapped muscle from the fracture line.
References
- Nezafati S, Mortazavi A, Arta SA, et al. 2018. Treatment and Complications of Patients with Zygomatic Fractures. 23.[Ref.]
- Spitz JA, Bradford P, Hwang L, et al. 2018. Surgical Management of Zygoma Fractures in Patients with Pre-injury Facial Asymmetry. 10.[Ref.]
- Siy RW, Brown RH, Koshy JC, et al. 2011. General Management Considerations in Pediatric Facial Fractures. J Craniofac Surg. 22:1190-1195.[Ref.]
- Allred LJ, Crantford JC, Reynolds MF, et al. 2015. Analysis of Pediatric Maxillofacial Fractures Requiring Operative Treatment: Characteristics, Management, and Outcomes. J Craniofac Surg. 26: 2368-2374.[Ref.]
- Neinstein RM, Phillips JH, Forrest CR. 2012. Pediatric orbital floor trapdoor fractures: Outcomes and CT-based morphologic assessment of the inferior rectus muscle. J Plast Reconstr Aesthetic Surg. 65: 869-874.[Ref.]
- Nowinski D, Di Rocco F, Roujeau T, et al. 2010. Complex pediatric orbital fractures combined with traumatic brain injury: treatment and follow-up. J Craniofac Surg [Internet]. 21: 1054-1059.[Ref.]
- Hink" Durairaj. 2013. Evaluation and treatment of pediatric orbital fractures. 1International Ophthalmol Clin [Internet]. 53: 103-115.[Ref.]
- Susarla SM, Mundinger GS, O’Brien-Coon D, et al. 2016. Does Training Background Influence Decision-Making in the Management of Zygomaticomaxillary Complex Fractures? J Oral Maxillofac Surg. 74: 995-1012.[Ref.]
- Losee JE, Afifi A, Jiang S, et al. 2008. Pediatric orbital fractures: classification, management, and early follow-up. Plast Reconstr Surg. 122: 886-897.[Ref.]
- Cruz AA V, Eichenberger GCD. 2004. Epidemiology and management of orbital fractures. Curr Opin Ophthalmol [Internet]. 5: 416-421.[Ref.]
- Tahernia A, Erdmann D, Follmar K, et al. 2009. Clinical implications of orbital volume change in the management of isolated and zygomaticomaxillary complex-associated orbital floor injuries. Plast Reconstr Surg. 123: 968-975.[Ref.]
- Taub PJ, Buchman SR, Patel PK, et al. 2015. Ferraro’s fundamentals of maxillofacial surgery. Ferraro’s Fundamentals of Maxillofacial Surgery. 1-510.[Ref.]
- Hink EM, Wei LA, Durairaj VD. 2014. Clinical Features and Treatment of Pediatric Orbit Fractures. 30: 124-131.[Ref.]
- Buchanan EP, Hopper RA, Suver DW, 2012. Zygomaticomaxillary Complex Fractures and Their Association with Naso-Orbito-Ethmoid Fractures. Plast Reconstr Surg [Internet]. 130: 1296-1304.[Ref.]
- Luck JD, Lopez J, Faateh M, 2018. Pediatric Zygomaticomaxillary Complex Fracture Repair: Plastic and Reconstructive Surgery Advance.[Ref.]
- Joshi S, Kassira W, Thaller SR. 2011. Overview of Pediatric Orbital Fractures. J Craniofac Surg. 22: 1330-1332.[Ref.]
- Ridgway EB, Chen C, Colakoglu S, et al. 2009. The incidence of lower eyelid malposition after facial fracture repair: a retrospective study and meta-analysis comparing subtarsal, subciliary, and transconjunctival incisions. Plast Reconstr Surg. 124: 1578-1586.[Ref.]




















