Indexing & Abstracting
Full Text
Research ArticleDOI Number : 10.36811/irjo.2022.110014Article Views : 37Article Downloads : 32
The pattern of Visual and Refractive status of the children
Syeed Mehbub Ul Kadir1, Mahar Ali2, Subrata Kum Paul3, Sadia Yesmin Saki4, Abdullah Hel Azam5, S Faisal Ahmed6 and Saifuddin Ahmmed7
1Assistant Professor (Ophthalmology), Sheikh Fazilatunnesa Mujib Eye Hospital and Training Institute, Gopalgonj, Bangladesh
2Assistant Professor (Ophthalmology), Sheikh Fazilatunnesa Mujib Eye Hospital and Training Institute, Gopalgonj, Bangladesh
3Medical Officer, Sheikh Fazilatunnesa Mujib Eye Hospital and Training Institute, Gopalgonj, Bangladesh
4Junior Consultant (Ophthalmology), Sheikh Fazilatunnesa Mujib Eye Hospital and Training Institute, Gopalgonj, Bangladesh
5Junior Consultant (Ophthalmology), Sheikh Fazilatunnesa Mujib Eye Hospital and Training Institute, Gopalgonj, Bangladesh
6Junior Consultant (Ophthalmology), Sheikh Fazilatunnesa Mujib Eye Hospital and Training Institute, Gopalgonj, Bangladesh
7Professor and Director, Sheikh Fazilatunnesa Mujib Eye Hospital and Training Institute, Gopalgonj, Bangladesh
*Corresponding Author: Syeed Mehbub Ul Kadir, Assistant Professor and Consultant, Department of Oculoplasty and Ocular Oncology, Bangladesh Eye Hospital and Institute, 78-Satmosjid Road, Dhanmondi, Dhaka-1205, Bangladesh, Email: mehbubkadir@gmail.com
Article Information
Aritcle Type: Research Article
Citation: Syeed Mehbub Ul Kadir, Mahar Ali, Subrata Kum Paul, et al. 2022. The pattern of Visual and Refractive status of the children. Int Res J Optha. 4: 07-13.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2022; Syeed Mehbub Ul Kadir
Publication history:
Received date: 21 March, 2022Accepted date: 30 March, 2022
Published date: 01 April, 2022
Abstract
Aim: Amblyopia (lazy eye) may develop due to uncorrected refractive error, especially in schoolgoing age. We were attempting to assess the frequency of refractive error among the children.
Methodology: The prospective cross-sectional study was conducted in a tertiary eye hospital of Bangladesh from 01 February 2021 to 30 June 2021. The investigators will maintain pre-design data, and data were analyzed by SPSS software.
Results: 228 children from 6 years to 12 years of age were evaluated in this study. Boys were 142 (62.3%), and girls were 86 (37.7%). The Mean Age was 9.84 years. The Visual acuity was improved after the corrections of refractive errors in both eyes. Myopia (47.9%) was the highest occurrence among the children among the pattern of refractive errors. Myopic astigmatism (76.9%) was common in all types of astigmatism. 21% of children were associated with strabismus. Amblyopia was found in 6.6% of all. Ophthalmic trauma was noted as 16.7% of all children. Developmental cataracts, Healed keratitis, lacrimal drainage system disorders, congenital ptosis were the associated ophthalmic diseases.
Conclusion: Refractive error gradually increased with age. Simple myopia was the most common refractive error than hyperopia and astigmatism. Each child should evaluate the ocular condition and visual status for the early detection and management of refractive error and amblyopia.
Introduction
Ametropia (refractive error) is the most common cause of visual impairment and the second most common cause of blindness globally. The WHO has estimated that about 153 million people over the age of five years are visually impaired due to uncorrected Refractive Error (RE) [1,2]. Around 12.8 million children (aged 5 to 15 years) are visually impaired, with a global prevalence of 1% due to uncorrected or inadequately corrected refractive errors [2].
An impaired vision is defined as a patient having the best-corrected visual acuity less than 6/18 in the better eye. Blindness is defined by WHO as visual acuity less than 3/60 with the best possible correction in the better look on the Snellen visual acuity chart. The WHO and 20 international Non-Governmental Organizations (NGOs) launched the global initiative, "Vision 2020," in 1999 to eradicate avoidable blindness by the year 2020 [3]. The global cost of correcting vision impairment from uncorrected refractive error has been estimated at 2800 million US dollars [4]. Similarly, the potential productivity loss resulting from the global burden of uncorrected refractive error has been estimated to be 121.4 billion international dollars [5]. In low- and high-income countries, an uncorrected refractive error has significant economic implications for potential lost productivity [5]. Up to date information on the prevalence and causes of visual impairment is essential to set policies and priorities and evaluate global eye health [2]. The impact of refractive errors on the individual and the community cannot be ignored. Most of the children with an uncorrected refractive error are asymptomatic, and hence screening helps in early detection and timely interventions. The provision of spectacles to the needy is a cost-effective health intervention. Hence, the VISION 2020 initiative to eliminate avoidable blindness has prioritized refractive error correction and has placed it within the category of childhood blindness [6]. Uncorrected refractive errors attribute a significant percentage to visual impairment, which can cause significant ocular morbidity in children [7]. Early detection and timely management can help to prevent refractive error-related visual impairment. Refractive error is an avoidable cause of ocular morbidity. High Refractive error may cause permanent visual impairment. We attempt to assess the refractive error and associated ocular diseases among the children who attended the outpatient department of this hospital.
Materials and Methods
This prospective cross-sectional study was carried out in Sheikh Fazilatunnesa Mujib Eye Hospital and Training Institute (SFMEHTI) from 01 February 2021 to 30 June 2021 (Five months). Sheikh Fazilatunnesa Mujib eye hospital and training institute is a service-based tertiary eye hospital, and people are getting eye care service from 21 districts of the southern region of Bangladesh. This study was included all the children from 6 to 12 years who are attending the outpatient department of this hospital.
This study excluded all patients who were attended at the emergency department of the hospital, severely ill patients, non-cooperative patients, and the other permanent causes of visual loss, like corneal ulcer, phthisis bulbi, and intraocular tumour. Variables include age, gender, visual status, refractive status, strabismus, congenital ptosis, and amblyopia. Outcome measures included the mean age of the study subjects, the rate of refractive errors, the frequency of amblyopia, and associated ocular morbidities. Visual condition was assessed for all children using Snellen vision chart or available others vision chart. Cycloplegic refraction was for all children who presented with 6/9 or worse vision. Visual acuity was assessed initially and after seven days of the management but mentioned here only after seven days of the management of the unsound eye for all children with associated ophthalmic trauma. Before clinical evaluation, An informed written consent form was taken from the attended guardian of the patients. The researcher teams maintained pre-design data, and data were analyzed by SPSS software. The Ethical Consideration was maintained according to the declaration of Helsinki. The study received ethical clearance from Institutional review board (IRB) from the Sheikh Fazilatunnesa Mujib Eye Hospital and Training Institute (SFMEHTI), Gopalganj, Bangladesh.
Results
We evaluated 228 patients from 6 years to 12 years in this study. Boys were 142 (62.3%), and girls were 86 (37.7%). Most of them (100 children, 43.9%) were 11 to 12 years of age. 70 (30.7%) children were 6-8 years of age, and 58 (25.8%) were 9 to 10 years of age. The Mean Age ± SD of a total of 228 children were 9.84 ± 1.92 years. The minimum age was 6 years, and the maximum age was 12 years. The median was ten years, and the 95% of the confidence interval was from 9.59 t0 10.09. The visual acuity was improved after the corrections of refractive errors in both eyes. The uncorrected visual acuity was 6/12 or less in 50.4% and 49.5% of the right eye and left eye, respectively that was reduced to 10.5% (right eye) and 7.9% (left eye) after correcting the refractive errors (Table-1). 38 (16.7%) children presented with emmetropia, and the rest of the children (190, 83.3%) were associated with ametropia.
|
Table-1: Distribution of UCVA and BCVA of Right and Left Eye. |
||||
|
Visual Acuity |
Right Eye |
Left Eye |
||
|
UCVA |
BCVA |
UCVA |
BCVA |
|
|
6/9 to 6/6 |
113 |
204 |
115 |
210 |
|
6/18 to 6/12 |
92 |
18 |
92 |
16 |
|
6/36 to 6/24 |
15 |
04 |
15 |
02 |
|
5/60 to 6/60 |
06 |
02 |
04 |
00 |
|
≤4/60 |
02 |
00 |
02 |
00 |
|
Total |
228 |
228 |
228 |
228 |
Among the 190 study subjects with refractive errors, boys were 113, and girls were 77. Among the refractive error, Myopia (Table 2) was the highest occurrence (91 children, 47.9%), followed by astigmatism (78 children, 41%) and hyperopia (21 children, 11%). Myopia, astigmatism and hyperopia were 46.7% to 48.7%, 40.7% to 41.5% and 10.6% to 11.7%, respectively, in boys and girls.
|
Table-2: Distribution of refractive errors among the boys and girls. |
|||
|
Variables |
Boys |
Girls |
Total |
|
Myopia |
55 (48.7%) |
36 (46.7%) |
91 (47.9%) |
|
Astigmatism |
46 (40.7%) |
32 (41.5%) |
78 (41.0%) |
|
Hyperopia |
12 (10.6%) |
09 (11.7%) |
21 (11.0%) |
|
Total |
113 (59.7%) |
77 (60.3%) |
190 |
Among the 78 children presented with astigmatism, myopic astigmatism was 60 cases (76.9%), representing 26.3% of the total. Mixed astigmatism was evaluated in 12 (15.4%) children, and Hyperopic astigmatism was found in 6 (7.7%) study subjects. Strabismus (misalignment of eyes) were found in 50 (21.9%) study subjects. Among the children presented with strabismus, 45 (90%) children showed esotropia and 5 (10%) children were associated with exotropia. We found 15 patients presented with unilateral (33.3%) or bilateral (66.7%) amblyopia. Among them, Boys were 46.7%, and girls were 53.3%. 38 (16.67%) children were presented with a different pattern of ocular trauma. Sub-Conjunctival Hemorrhage was found in 15 (6.6%) children, Eyelid trauma was found in 4 (1.7%) children, Corneal abrasion was noted in 8 (3.5%) study subjects, Ocular surface foreign body was extracted from 6 (2.6%) children, globe injury was diagnosed in 3 (1.04%) subjects. Canalicular trauma was evaluated in 2 (0.69%) children.
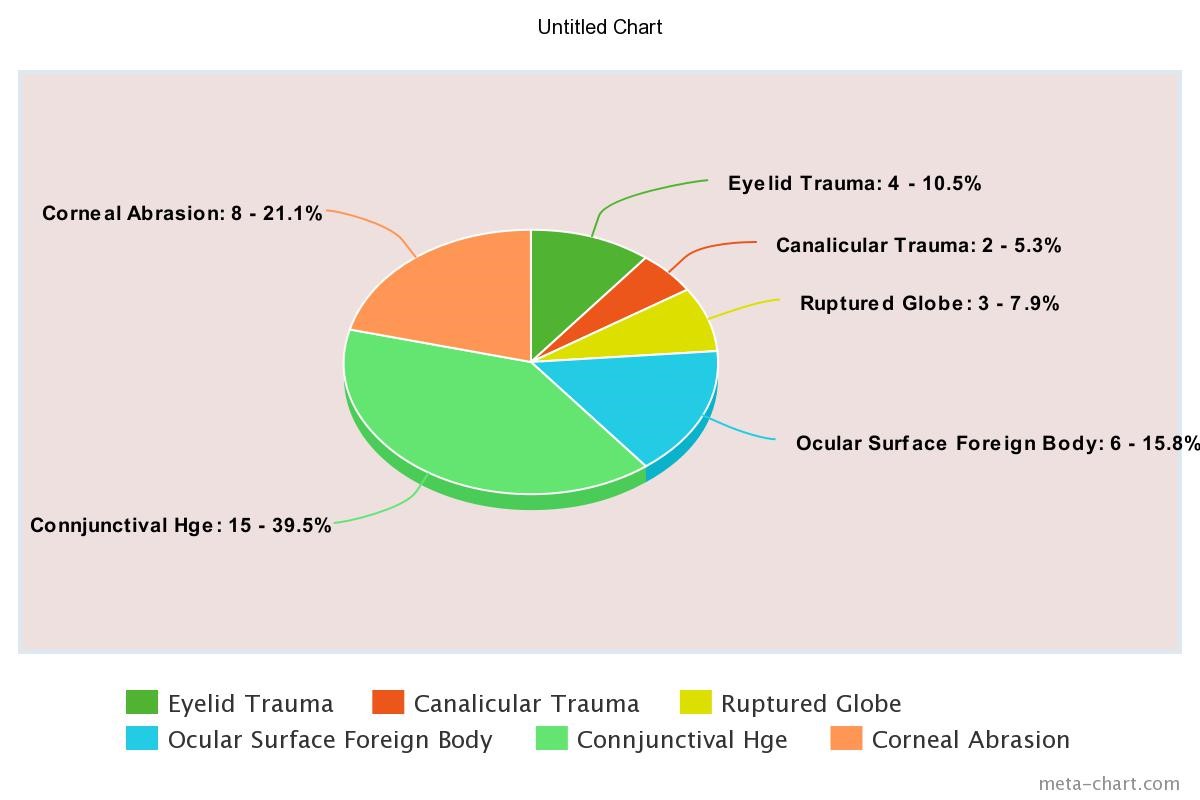
The associated ocular diseases (Graph 1) were evaluated in our study—68 (29.8%) children presented with associated ocular disease. Among the 68 children, Ocular surface diseases were noted in 32 (47.1%) cases, eyelid disorders were found in 24 (35.3%) children, lacrimal drainage system disorders were noted in 8 (11.8%) cases, and cataract was diagnosed in 4 (5.9%) cases.
Discussion
Refractive error is a commonly encountered visual problem in children and may be associated with another ocular morbidity [8,9]. Refractive error may be associated with strabismus (squinting eye) and amblyopia (lazy eye). Uncorrected refractive errors contribute a significant percentage to a visual impairment, which can cause significant ocular morbidity in children. Awareness building among the teachers, students, community leaders, and guardians can help evaluate the visual status and prevent the children's visual impairment. We assessed 228 children in the study time. According to their refractive status, the children were divided into four groups: emmetropia, myopia, hyperopia, and astigmatism. The Mean Age ± SD of the children is 9.84 ± 1.92 years. The age range is six years to 12 years, and the median age is10 years. Boys are 62.3%, and girls are 37.7%. A study reported the boys (52.5%) and girls (47.5%), with a ratio of 1.1:1. The mean age was 10.41 years ± 2.73 years [10]. The mean age of children was reported as 9.2 ± 2.8 years with an age range of 4 to 17 years [11]. The age range of children was 5 to 15 years, with 39.3% boys and 60.7% girls [10]. We assessed the refractive status, the pattern of refractive error, and associated ocular diseases among the children who will attend the outpatient department of this hospital. In this study, The visual acuity was improved after the corrections of refractive errors in both eyes, and all children were happy to explore surrounding scenarios. The uncorrected visual acuity was 6/12 or less in 50.4% and 49.5% of the right eye and left eye, respectively that was reduced to 10.5% (right eye) and 7.9% (left eye) after correcting the refractive errors. The uncorrected visual acuity was 6/9 to 6/6 in 49.5% of right eyes, and BCVA was improved to 89.4%. The scenarios were almost identical in left eyes (UCVA-50.4%, BCVA-92.1%). The VA was 6/12 or worst in 50.4% and 49.5% of the right eye and left eye, respectively, reduced to 10.5% (right eye) and 7.9% (left eye) in BCVA. The study cases reported a very high proportion of ametropia. The higher rate of ametropia is found in our study that is similar to other studies [12,13]. In this study, emmetropia is evaluated in 16.7% of study children and ametropia is noted in 83.3%. A significant number of children was presented in the hospital with ametropia. This study studied a overview of the refractive status, and associated ophthalmic diseases like strabismus, ptosis, and cataract.
The common refractive errors were myopic (53%), astigmatism (23%), hypermetropic (9.3%), and the rest of the children was emmetropia (14.8%). Binocular amblyopia was found in 25.2% of children, and monocular amblyopia was found in only 7.6% of children. The cover test showed 3.8% manifest strabismus [14]. By the age of six, most children would be, on average, 0.75D hyperopia with a shift toward higher hyperopia. The late onset of myopia (more than six years) is associated with a linear development followed by a rapid rise in myopia, the relative stability [15]. The distribution of refractive status changes gradually positively skewed to negatively skewed distributions as age increases, with 9-year- old being the critical age for changes [11]. The refractive status of children is overwhelmingly hyperopic, with a normal distribution of spherical equivalent refractive error [14]. Significant refractive errors were revealed among children aged 5-15 years [10]. Myopia is the most significant refractive error in our study in the children, about 40% of all study subjects. Astigmatism and hypermetropia are noted in 34.2% and 9.2% of all children. In the children with myopia, boys were 48.7%, and girls were 46.7%. There is no statistically significant dissimilarity in the distribution of boys and girls [10,13,15,16]. The prevalence of myopia in school-going children of Taiwan is much higher than that in other countries [11].
Astigmatism is the second refractive error (41%) in our study. Myopic, mixed and hyperopic astigmatism have been observed in 76.9%, 15.4% and 7.7% among the boys (40.7%) and girls (41.5%) with astigmatism refractive errors. In our study, hyperopia (11%) is the least amount of refractive error. If the refractive error is untreated, it may lead to amblyopia (Lazy eye) that can affect the personal as well as academic development of a child. High Refractive error may cause permanent visual impairment [17,18]. In our study, Total amblyopia is found in 15 (6.7%) children. Bilateral amblyopia was 66.7%, and girls (53.3%) were slightly preponderant than boys (46.7%). Strabismus (misalignment of eyes) is found in 50 (21.9%). The most common strabismus is alternate esotropia (90%). 16.7% of children were presented with different patterns of ocular trauma. Sub-Conjunctival Hemorrhage was the most common presentation. Early detection and timely management can tremendously improve the child's potential. Increasing the occurrences of myopia and astigmatism, but it is not clear whether the occurrence increases were caused by prolonged near-work activities or reduced outdoor activities because of a load of study, a trend with children spending a significant amount of time engaged in using smartphones (mobile), tab, computer or laptop for game fascination and also reducing the outdoor games and movements[19-21]. The outdoor activities are helpful to protect against the development of myopia, rather than near-work activities that cause myopia. Reducing near-work activity and preserving outdoor time reduce the prevalence of myopia in children [20].
Conclusion
Ametropia (Refractive Error) is common in school-going children. Myopia is the most common refractive error than astigmatism and hyperopia. Ophthalmic assessment is mandatory for six months to manage refractive errors and associated ocular diseases. There are several limitations noted in this study. Cycloplegic refraction was done with cyclopentolate 0.5% eye drop. This study was carried out on a hospital-based and could not involve a large population.
References
1. Khurana AK. 2006. Textbook of ophthalmology. 3rd ed. New Delhi: New Age International Publisher. 52-59.
2. Pascolini D, Mariotti SP. 2012. Global estimates of visual impairment: 2010. Br J Ophthalmol. 96: 614-618. Ref.: https://pubmed.ncbi.nlm.nih.gov/22133988/ DOI: https://doi.org/10.1136/bjophthalmol-2011-300539
3. Pizzarello L, Abiose A, Ffytche T. 2004. VISION 2020: The right to sight: A global initiative to eliminate avoidable blindness. Arch Ophthalmol. 122: 615-620. Ref.: https://pubmed.ncbi.nlm.nih.gov/15078680/ DOI: https://doi.org/10.1001/archopht.122.4.615
4. Negrel AD, Maul E, Pokharel GP. 2000. Refractive error study in children: Sampling and measurement methods for a multi-country survey. Am J Ophthalmol. 129: 421-426. Ref.: https://pubmed.ncbi.nlm.nih.gov/10764848/ DOI: https://doi.org/10.1016/s0002-9394(99)00455-9
5. Fricke TR, Holden BA, Wilson DA. 2012. Global cost of correcting vision impairment from uncorrected refractive error. Bull World Health Organ. 90: 728 738. Ref.: https://pubmed.ncbi.nlm.nih.gov/23109740/ DOI: https://doi.org/10.2471/blt.12.104034
6. Smith TS, Frick KD, Holden BA. 2009. Potential lost productivity resulting from the global burden of uncorrected refractive error. Bull World Health Organ. 87: 431 437. Ref.: https://pubmed.ncbi.nlm.nih.gov/19565121/ DOI: https://doi.org/10.2471/blt.08.055673
7. Resnikoff S, Pascolini D, Mariotti SP. 2008. Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bull World Health Organ. 86: 63-70. Ref.: https://pubmed.ncbi.nlm.nih.gov/18235892/ DOI: https://doi.org/10.2471/blt.07.041210 v
8. Dandona R, Dandona L. 2001. Refractive error blindness. Bull World Health Organ. 79: 237-243. Ref.: https://pubmed.ncbi.nlm.nih.gov/11285669/
9. Fricke TR, Holden BA, Wilson DA. 2012. Global cost of correcting vision impairment from uncorrected refractive error. Bull World Health Organ. 90: 728-738. Ref.: https://pubmed.ncbi.nlm.nih.gov/23109740/ DOI: https://doi.org/10.2471/blt.12.104034
10. Shrestha GS, Sujakhu D, Joshi P. 2011. Refractive error among school children in Jhapa, Nepal. J Optom. 4: 49-55.
11. Lin LL, Shih YF, Hsiao CK. 2004. Prevalence of myopia in Taiwanese schoolchildren: 1983 to 2000. Ann Acad Med Singapore. 33: 27-33. Ref.: https://pubmed.ncbi.nlm.nih.gov/15008558/
12. Ali ABM, Talha AKB, Elmadina AEM. Refractive Errors status among children examined at optical centre in Khartoum state.
13. Ekkdawi NS. 2018. Refractive Development. American Academy of Ophthalmology.
14. Yamamah GA, Talaat Abdul, Mostafa YS. 2015. Prevalence of visual impairment and refractive errors in children of South Sinai, Egypt ophthalmic epidemiology. 22: 246-252. Ref.: https://pubmed.ncbi.nlm.nih.gov/26218107/ DOI: https://doi.org/10.3109/09286586.2015.1056811
15. Pokharel A, Pokharel PK, Das H. 2010. The patterns of refractive errors among the school children of rural and urban settings in Nepal. Nepalese Journal of Ophthalmology. 2: 15-27. Ref.: https://pubmed.ncbi.nlm.nih.gov/21505527/ DOI: https://doi.org/10.3126/nepjoph.v2i2.3717
16. Pavithra MB, Maheshwaran R, Rani Sujatha MA. 2013. A study on the prevalence of refractive errors among school children of 7-15 years age group in the field practice areas of a medical college in Bangalore. Int J Med Sci Public Health. 2: 641-645.
17. Chen TC, Tsai TH, Shih YF. 2010. Long-term evaluation of refractive status and optical components in the eyes of children born prematurely. Invest Ophthalmol Vis Sci. 51: 6140-6148. Ref.: https://pubmed.ncbi.nlm.nih.gov/20688740/ DOI: https://doi.org/10.1167/iovs.10-5234
18. Padhye AS, Khandekar R, Dharmadhikari S. 2009. Prevalence of uncorrected refractive error and other eye problems among urban and rural school children. Middle East Afr J Ophthalmol. 16: 69-74. Ref.: https://pubmed.ncbi.nlm.nih.gov/20142964/ DOI: https://doi.org/10.4103/0974-9233.53864
19. Akova BB, Kivanc SA, Olcaysu OO. 2015. Association of Birth Parameters with Refractive Status in a sample of Caucasian Children Aged 4-17 years. Jr of Ophthalmol. 5. Ref.: https://pubmed.ncbi.nlm.nih.gov/25949820/ DOI: https://doi.org/10.1155/2015/635682
20. Rose KA, Morgan IG. 2008. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology. 115: 1279-1285. Ref.: https://pubmed.ncbi.nlm.nih.gov/18294691/ DOI: https://doi.org/10.1016/j.ophtha.2007.12.019
21. Asma T, Hossain M, Naznin S. 2020. Distribution of Myopia among school-going children. Jr of National Inst of Ophthalmol. 3: 22-28.




















