Indexing & Abstracting
Full Text
Research ArticleDOI Number : 10.36811/ijrmsh.2020.110008Article Views : 6Article Downloads : 16
Determination of the Duration of single Pregnancy in Dakar and the Contributing Factors
DIOUF A1,2,3*, Gueye M2,3, Ndiaye MD3, Thiam O1, WADE M3, DIAKHATE A3, DIALLO M4, DIALLO AK3, Mbodj A3, DIOUF A4 and Mbaye M2
1Regional Hospital Center of Saint-Louis, BP 401, Dakar, Senegal
2Philippe Maguilen SENGHOR health center, BP: 29026 or 8951 Aéroport Yoff, Dakar, Senegal
3Gynecological and Obstetric Clinic, EPS Aristide Le Dantec, BP 3001, Dakar, Senegal
4National Hospital Center of Pikine, BP 20630, Dakar, Senegal
*Corresponding Author: Dr Aliou DIOUF, Regional Hospital Center of Saint-Louis, BP 401, Tel: 002216412302; Email: alioudiouf69@yahoo.com
Article Information
Aritcle Type: Research Article
Citation: DIOUF A, Gueye M, Ndiaye MD, et al. 2020. Determination of the Duration of single Pregnancy in Dakar and the Contributing Factors. Int J Reprod Med Sex Health. 2: 06-17.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2020; DIOUF A
Publication history:
Received date: 06 January, 2020Accepted date: 09 January, 2020
Published date: 13 January, 2020
Abstract
Objectives: To determine the duration of single-fetal pregnancy in black Senegalese women and the factors that contribute to it.
Patients and methods: This is a retrospective and prospective cross-sectional study that evaluated parturients admitted to the Philippe Maguilen Senghor health center for the management of their delivery of a monofoetal pregnancy from January 1, 2012 to December 31, 2018. All parturients with the following characteristics were included: monofoetal pregnancy, date of last menstrual period known or reconstituted on the basis of an early ultrasound (≤13SA + 6 days), a term of pregnancy greater than or equal to 37 weeks, spontaneous induction from work and a child living at birth. The data was entered into our e-Perinatal computer database and analyzed first on Microsoft Excel 2016 and then using SPSS 24 Mac version software. The continuous quantitative variables were described by their position and dispersion parameters: mean, median, mode and standard deviation. They were compared using the ANOVA test. The relationship between the quantitative variables was assessed using a bivariate linear correlation. The level of significance used was 0.05.
Results: Over 7 years, 13,292 parturients met the inclusion criteria, representing a frequency of 35.6% of all admissions. The average age was 27.36 years with extremes of 13 and 49 years. Almost 9 in 10 parturients were under the age of 35. The average duration of gestation was 278.69 days, the median was 278 days while the mode was 279 days; which corresponded respectively to 39SA + 6 days, 39SA + 5 days and 39SA + 6 days. Parity, maternal age and type of fetal presentation did not influence the duration of pregnancy. However, male fetuses were born on average one day earlier (39SA + 5) compared to female fetuses.
Conclusion: The Senegalese black woman gives birth on average 6 to 10 days earlier than the Caucasian woman. Boys are born a day earlier than girls. It is necessary to encourage women to remember the date of their last period and to consult early enough for an early ultrasound. Finally, it is necessary to consider a larger study to clarify the duration of pregnancy in black women on an African scale in order to provide recommendations for clinical practice.
Keywords: Duration of pregnancy; Expected date of delivery; Dakar
Introduction
Calculating the expected date of delivery is an ancient practice and widespread in the world and constitutes a fundamental time of the surveillance of the pregnancy. In practice, the date which, by professional agreement, corresponds to 9 months of the calendar varies between 41 SA + 0 to 41 SA + 3, depending on whether or not February is included in the pregnancy [1]. The World Health Organization sets the timeout to 294 days after the date of the last period. Despite the uncertainties, estimating the DPA makes it possible to envisage setting up an adapted monitoring of the pregnancy in order to prevent fetal and neonatal complications [2]. Determining the average duration of pregnancy has been the subject of numerous studies across large cohorts with variable results [3] There seem to be variations depending on maternal and fetal characteristics, which makes it possible to consider the duration of pregnancy as a biological parameter, with inter- and intraobserver variability [4]. The lack of consensus in the literature and, above all, the maternal and fetal variability factors make it illusory to tell patients of an exact APD. However, such precision is of medical interest because it makes it possible to determine the monitoring interval at the end of pregnancy, which has a higher prevalence of maternal and neonatal complications. In Africa, data on the expected date of delivery are scarce and this observation leads us to take stock of DPA in our structure. The objective of this work is to determine the duration of gestation in our African context and contributing factors.
Patients and Method
It is a retrospective and prospective, transversal study, having evaluated the patients admitted to the Philippe Maguilen Senghor health center for treatment burden of delivery of a single fetal pregnancy.
This study covers a period of seven (07) years from January 1, 2012 to December 31, 2018 with two periods: a first registration period retrospective from 2012 to 2016 and a second period of prospective registration data for the years 2017 and 2018. Included in the study were all patients admitted for management of their delivery with the following characteristics:
* monofoetal pregnancy;
* date of the last period known or reconstituted on the basis of a early ultrasound (≤ 13SA + 6 days);
* regular menstrual cycle;
* term of pregnancy ≥ 37SA;
* no intercurrent maternal pathology which could interfere with induction of labor;
* spontaneous induction of labor;
* child living at birth.
The data was entered into our e-Perinatal computer database.
The data was entered into our e-Perinatal computer database.
They were then extracted and analyzed first on Microsoft Excel 2016
then Statistical Package for Social Science (SPSS 24), Mac version.
Continuous quantitative variables were described by their parameters of position and dispersion: mean, median, mode, standard deviation. They were compared using the ANOVA (ANalysis Of VAriance) test. In case of rejection of the null hypothesis (equal variances), the inter-group significance was analyzed using multiple post-hoc comparisons using the T2 test of Tamhane or T3 from Dunnett. The relationship between the quantitative variables was evaluated using a bivariate linear correlation and, if visually consistent, by a linear regression with calculation of the coefficient a of the slope and the constant b of the following equation: y = ax + b (y = dependent variable - x = independent variable). The level of significance used was 0.05.
Results
1. Descriptive results
a. Frequency
Between January 1, 2012 and December 31, 2018, the establishment recorded 13, 292 deliveries that met the inclusion criteria, i.e. 35.6% of all admissions. The distribution of women by year is reported in following graphic:
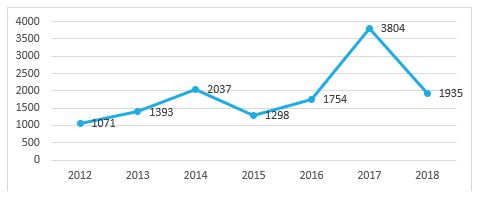
Figure 1: Evolution annuelle des accouchements entre 2012 et 2018.
b. Socio-demographic characteristics
• Age
The average age of the patients was 27.36 years with extremes of 13 and 49 years. The most represented age group was that of 20 to 29 years old who
was 54.9% of the sample as shown in the following figure.

Figure 2: Répartition des patientes selon la classe d’âge.
Almost 9 in 10 patients (85.8%) were under 35 years of age, while patients 35 years of age and over made up less than 15% of the sample (14.2%).
* Parity
Our sample consisted of 55% multiparas and 45% primiparas.
c. Pregnancy and childbirth data
* Distribution of births according to gestational age
The average gestation time was 278.69 days, the median was 278 days while the mode was 279 days, which corresponded in weeks of amenorrhea to 39SA + 3d, 39SA + 2d and 39SA + 6d respectively. Figure 3 shows the distribution of births between 259 days and 315 completed days.

Figure 3: Distribution of births according to gestational age.
About 35% of deliveries took place between 275 and 280 days, i.e. respectively 39SA + 2d and 40SA + 0 and, 20% in each of the weeks which preceded or followed this interval (Figure 8).
• Birth gender
Male infants accounted for more than half of the sample (53.8%) as shown in Figure 4. The sex ratio was 1.16.

Figure 4: Distribution of newborn according to the sex.
* Type of presentation
The presentation of the summit was found in more than 9 out of 10 patients (95.3%). The distribution of patients by type of presentation is reported in Table I.
|
Table I: Distribution of patients by type of presentation. |
||
|
Presentation |
Number |
Rate (%) |
|
Summit |
12 673 |
95,3 |
|
Seat |
531 |
4 |
|
Face |
38 |
0,3 |
|
Front |
15 |
0,1 |
|
Transverse |
35 |
0,3 |
|
Total |
13 292 |
100 |
Analytical Results
a. Gestation duration correlated to parity
On the point cloud diagram of figure 5, we notice that the duration of pregnancy does not follow a linear distribution, the term being divided from fairly similar according to parity except in large multiparas.

Figure 5: Scatter plot of newborn babies by parity.
This constant was also reflected on the parity average: 278.57 days for nulliparous women and 278.78 days for multiparous women. Although they appear slightly different, their respective variances were similar (Figure 6). The difference is not statistically significant as shown in Table II.

Figure 6: Gestation duration correlated to parity.
|
Tableau II: Gestation duration correlated to parity. |
|||||
|
|
Number of deliveries |
Duration (days) |
Standard deviation (days) |
p |
IC 95% |
|
Nulliparous |
5985 |
278,57 |
10,08 |
0,24 |
-0,13-0,55 |
|
Multipare |
7307 |
278,78 |
10,20 |
||
* a. Duration of gestation correlated with maternal age
As with parity, the duration of pregnancy did not follow a linear distribution by maternal age (Figure 7).

Figure 7: Scatter plot of newborn babies by maternal age.
Recoding the variable “Maternal Age” into two categories with a cut-off point at 35 also did not show any significant difference between the two groups. In patients under 35, gestation was 278.63 days compared to 278.96 days for parturients aged 35 and over.
Figure 8 and Table III show the distribution of duration of pregnancy by maternal age.

Figure 8: Distribution of duration of pregnancy by maternal age.
* Duration of gestation correlated with fetal presentation
Among parturients received with a presentation of the summit, the duration of gestation was 278.71 days and 278.19 days for those with an irregular presentation (Figure 9). The difference was not statistically significant as shown in Table IV.
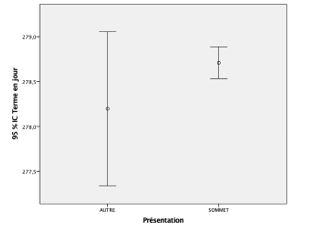
Figure 9: Duration of gestation correlated with fetal presentation.
|
Table IV: Duration of gestation correlated with fetal presentation |
|||||
|
Fetal presentation |
Number of deliveries |
Duration (days) |
Standard deviation |
p |
IC 95% |
|
Summit |
12676 |
278,71 |
10,11 |
0,22 |
-0,31-1,33 |
|
Others |
619 |
278,19 |
10,86 |
||
a. Duration of gestation correlated with the sex of the child
In women who gave birth to a newborn male, the gestation period was 278.46 days while it was 278.94 days for those with a newborn like the shows figure 10.
The difference in durations of pregnancy was statistically significant as shown in the following table:
|
Table IV: Difference in durations of pregnancy according to the sex of the child. |
|||||
|
sex |
Number of deliveries |
Duration |
Standard deviation |
P value |
IC 95% |
|
Male |
7146 |
278,46 |
10,375 |
0,007 |
-0,12-0,81 |
|
Female |
6146 |
278,940 |
9,88 |
||

Figure 10: Duration of gestation correlated with the sex of the child.
To better assess the influence of sex on the duration of gestation, we had calculated the relative risk of childbirth of a female newborn per additional week from 37 weeks of gestation as shown in Table VI. The risk appears from 39 SA.
Discussion
Limits of the study
The main limitation of our study may seem to be the sample size compared to those of population studies with national registers such as the Swedish birth register from 1976 to 1980 studied by Bergsjo et al. with 427,581 births [5]. One of the inclusion criteria, however, must be remembered, which was knowledge of the date of the last period or the existence of an early ultrasound less than 14 weeks pregnant. Knowing the Senegalese population, it is easy to understand that the date of the last rules is an event rarely remembered and that the achievement of a early ultrasound is not a common practice. According to data from the 6th Demographic and Health Survey, nearly 40% of pregnant women had made their first prenatal consultation after the 4th month of pregnancy [11]. This fact partly explains the difficulties associated with dating pregnancy and the problems associated with it. However, our study spans 7 years and includes almost 40% of patients who gave birth at the Philippe Maguilen Senghor Health Center. It is then representative of the population. Other smaller samples are also reported in the literature. In 2001, Smith et al. and Mittendorf et al. Have performed studies on samples of 1,514 women and 104 pregnant women respectively [6,7].
Maternal age and duration of pregnancy
The average age of parturients was 27.36 years with extremes of 13 and 49 years. The most represented age group in our study was that ranging from 20 at 29 (54.9%) close to that of Bergsjo et al. (62%) [5]. Nearly 9 patients on 10 were under the age of 35 (85.8%). In patients under 35 years, gestation was 278.63 days compared to 278.96 days for parturients aged 35 years or more. In the literature, the studies by Smith et al. 2001 and from Eden et al. 1992 had found no impact of age compared to the duration of pregnancy in their study of 1514 women [7-12].
Parity and duration of pregnancy
The influence of parity on the duration of pregnancy has prompted many of interrogations and at the origin of several studies, some of which admit its role in the variability of the duration of gestation. Our sample was mainly composed of multiparous (55%) against 45% of primiparous and we noticed that the duration of the pregnancy did not follow a linear distribution compared to the parity. In the literature, several authors have shown that multiparous women give birth earlier than primiparous women. Bergsjo et al. 1990, reported that multiparous mothers under 35 had given birth slightly earlier than nulliparous women [5]. Mittendorf et al. estimate that primiparas reach the term of pregnancy at 288 days from the last period and multiparas at 283 days [7]. However, this factor seems controversial and several studies do not evidence no correlation between parity and duration of pregnancy [13].
Fetal presentation and duration of pregnancy
In our study, the duration of pregnancy was slightly longer in the summit presentation, 278.71 days versus 278.19 days in presentations birregular. In the literature, few authors have been interested in the impact of the type of presentation in the duration of pregnancy. However, Beisher et al. In a prospective study of 2972 patients followed since the first trimester did not show any significant difference in the duration of pregnancy between the group of summit presentations and the group of other so-called irregular presentations such as the seat, the face, the shoulder and the forehead [9]. It is nevertheless recognized that irregular presentations favor the prolongation of the duration of pregnancy by a lack of stress on the cervix by the fetal cephalic pole [14].
Ethnicity and duration of pregnancy
Several authors are interested in the influence of race on the duration of gestation. In 2003, out of a series of 122,000 pregnancies with spontaneous induction of labor, Patel et al. reported shorter pregnancies in black and Asian women (median 39 SA) compared to Caucasians (40 SA) who were the reference group [15]. It is hypothesized to explain a shorter gestation period in black women for an early maturation of the fetal-placental unit in part related to the size of the maternal pelvis. The basins of black women are indeed narrower compared to those of Caucasian. This certainly provides stability in the standing position and works but increases the risk of cesarean section for a narrowed pelvis. Even if the development of the brain is beneficial for the fetus, adaptation makes the fetus matures much earlier to avoid conflicts between the pelvis maternal and the dimensions of the fetal head. On the other hand, it is established that gross motor skills develop much more earlier in black infants than in their racial counterparts white, evidence of early maturation [16]. The incidence of passage of meconium (sign of neuro-muscular maturity) goes from minus 5% before 34SA in Europeans to more than 25% after 40 SA whereas in black women, the incidence of meconium emission in the fluid is higher, all gestational ages combined [15]. In 2009, Caughey et al. In the United States, found a decreased risk of childbirth after 41 + 0 SA in women of African American, Latin and Asian descent compared to Caucasian women [8]. Other studies, notably that conducted by Hugues et al., Have shown a longer gestation period in Chinese patients than in Malaysian and Indian patients [17]. In Africa, our study being one of the few in the field confirms these results with an average duration of pregnancy reduced by 7 days compared to the average for pregnant Caucasians. This new information should lead to a review of the definition of pregnancy prolonged as well as that of the exceeding of term. The latter are based on a theoretical pregnancy duration of 41 weeks of amenorrhea which is not the case in this present study or in the study by Omigbodun in Nigeria where the average gestation duration was 273 days [18]. In France for example, the recommendations of the High Authority for Health (HAS) are based on a definition of prolonged pregnancy from 41 weeks on, and therefore impose strict and rigorous surveillance of all pregnant women from this date, with cervical induction or maturation if the patient does not go into labor spontaneously, in order to obtain a delivery before 42 SA [10]. She recommends first of all an ultrasound of the first quarter between 11 SA and 13 SA + 6 days allowing precise dating of the pregnancy from the cranio-caudal length of the embryo according to strict criteria previously established. Its systematic practice contributes to reduce the number of terms wrongly considered to be out of date. This brings us back to the problem of dating pregnancy discussed above. These recommendations are similar to those of the American College of Obstetricians and Gynecologists (ACOG), of the Society of Obstetricians and Gynaecologists of Canada (SOGC) and the Royal College of Obstetricians and Gynecologists (RCOG). These Anglo-Saxon learned societies recommend taking charge from 41 weeks, with a possible trigger at this term if local conditions are favorable and the patient agrees [10]. It is therefore legitimate to question the applicability of such recommendations in our country. However, a larger study is needed to confirm the results of our study. A learned society such as the Senegalese Association of Gynecology-Obstetrics (ASGO) can conduct such a study and make recommendations for clinical practice. This is the time to have a high authority for health or a national health assessment and accreditation agency like France and developed countries.
Fetal sex and duration of gestation
Studies on this subject are contradictory. According to several authors, pregnancies of male fetuses made gestation longer. Vorheer observed a male predominance in the average length of gestation [19] as well as Divon et al. About 656,423 deliveries of which 333,192 were male and 323,231 were male feminine. The mean duration of pregnancy was higher in boys (280,6+ / -8, 9 days) than girls (279.8 ± 8.6 days). [20] We found an average of 278.46 days (39 weeks + 5 days) in children of male versus 278.94 days (39SA + 6d) in female sexes The duration gestation was significantly shorter in boys than in girls. Smith et al. Find the same duration (283 days) for each sex from of a population of 1,514 parturients [6]. In 1969 France and Liggins described an absence of steroid sulfatase activity placenta during pregnancy associated with very low estrogen production [21]. This enzyme deficit linked to a genetic abnormality in the X-linked recessive mode was also associated with prolonged pregnancy. In more than 90% of cases, it resulted from a deletion of the gene on the X chromosome which codes for the production of the placental steroid sulfatase. The reported incidence is from 1 to 2,000 to 1 to 6,000 male fetuses, which they say explains a longer duration of pregnancy in male fetuses. Although confirming the results in favor of the influence of the male sex on the duration of pregnancy, our results differ with them.
Conclusion
Between January 1, 2012 and December 31, 2018, the establishment recorded 13 292 deliveries that met the inclusion criteria, i.e. 35.6% of all admissions. The average age of the patients was 27.36 years with extremes of 13 and 49 years. Almost 9 in 10 patients (85.8%) were under 35 years of age. Our sample consisted of 55% multiparas and 45% primiparas. The average gestation period was 278.69 days, the median was 278 days while the mode was 279 days, which corresponded in weeks of amenorrhea to 39SA + 6d, 39SA + 5d and 39SA + 6d respectively. Male infants accounted for more than half of the sample (53.8%). The sex ratio was 1.16. The presentation of the summit was found in more than 9 out of 10 patients (95.3%). Parity, age and type of fetal presentation did not affect the duration of pregnancy. However, male fetuses were born on average one day earlier (39SA + 5d) compared to female fetuses. In summary, the Senegalese black woman gives birth on average 5 to 7 days earlier than the Caucasian woman. Boys are born a day earlier than girls.
References
1. MARDJANE N. 2013. Date présumée de l'accouchement : incertitude sur la durée de la gestation. Vocation Sage-femme. 12: 17-21.
2. ORGANISATION MONDIALE DE LA SANTEÅL. International Statistical Classification of Disease and Related Health Problems.10ème révision Genève, 2007.
3. LE RAY C, ANSELEM O. 2012.Comment définir la date présumée de l'accouchement et le dépassement de terme? La Revue Sage-Femme. 11: 48-53. Ref.: https://bit.ly/37Ne07r
4. KISTKA Z, PALOMAR L, BOSLAUGH S, et al. 2007.Risk for postterm delivery after previous post-term delivery. Am J Gynecol Obstet. 196: 241-246. Ref.: https://bit.ly/2uzMZq5
5. BERGSJO P, DENMAN HOWARD W, HOFFMANN H, et al. 1990. Duration of human singleton pregnancy. A population-based study. Acta Obstet Gynecol Scand. 69: 197-207. Ref.: https://bit.ly/2QB1HoZ
6. SMITH G. 2001. Use of time to event analysis to estimate the normal duration of human pregnancy. Human Reproduction. 16: 1497-1500. Ref.: https://bit.ly/37J05iO
7. MITTENDORF R, WILLIAMS M, BERKEY C, et al. 1990. The length of uncomplicated human gestation. Obstet Gynecol. 75: 929-932. Ref.: https://bit.ly/2tESUtk
8. CAUGHEY A, STOTLAND N, WASHINGTON A, et al. 2009. Who is at risk for prolonged and postterm pregnancy? Am J Obstet Gynecol. 200: 683e1-683e5.
9. BEUCHER G, DREYFUS M. 2008. Prise en charge du dépassement de terme. La Revue de la Sage-Femme. 7: 118-129. Ref.: https://bit.ly/301lFMY
10. HAUTE AUTORITEÅL DE LA SANTEÅL. 2008. Déclenchement artificiel du travail à partir de 37 semaines d’aménorrhée. HAS/Service des bonnes pratiques professionnelles et Service évaluation Économique et santé publique, Avril. AGENCE NATIONALE DE LA STATISTIQUE ET DE LADEÅLMOGRAPHIE. 2015.
11. Enquête Démographique et de Santé Continue (EDS-Continue 2014). Rockville, Maryland, USA.
12. EDEN RD, SEIFERT LS, WINEGAR A, SPELLACY W. 1987. Périnatal characteristics of uncomplicated post-date pregnancies. Obstet Gynecol. 69: 296-299. Ref.: https://bit.ly/2QFwlOl
13. ALEXANDER JM, LEVENO JK. 2000. Outcomes by week of gestation. Obstet Gynecol. 96: 291-294. Ref.: https://bit.ly/2s9kSx1
14. HARRIS BA. 1983. The unfavorable cervix in prolonged pregnancy. Obstet Gynecol. 62:171-174. Ref.: https://bit.ly/35wX43G
15. PATEL RR, STEER P, DOYLE P, et al. 2004. Does gestation vary by ethnic group. A London-based study of over 122,000 pregnancies with spontaneous onset of labour. Int J Epidemiol. 33: 107-113. Ref.: https://bit.ly/305eOlN
16. ILOEJE S, OBIEWE W, KAINE W. 1991. Gross motor development of Nigerian children. Ann Trop Paediatr.11: 33-39. Ref.: https://bit.ly/2NalhGz
17. HUGUES K, TAN NR, LUN KC. 1984. Low birthweight of live singletons in Singapore. International Journal of Epidemiology. 13: 465-471. Ref.: https://bit.ly/2QXAUm4
18. OMIGBODUN A, ADEREMI ADEWUYI A. 1997. Duration of human singleton pregnancies in Ibadan, Nigeria. J Natl Med Assoc. 89: 617-621. Ref.: https://bit.ly/36ATqXO
19. VORHERR H. 1975. Placental insufficiency in relation to post-term pregnancy and fetal postmaturity. Evaluation of fetoplacental function; management of the post-term gravida. AmJ Obstet Gynaecol. 123: 67-103. Ref.: https://bit.ly/2QZ4ojd
20. ALEXANDER JM, LEVENO JK. 2000. Forty weeks and beyond: Pregnancy outcomes by week of gestation Obstet Gynecol. 96: 291-294. Ref.: https://bit.ly/2T2JX7T
21. FRANCE J, LIGGINS G. 1969. Placental sulfatase deficiency. J Clin Endocrinol Metab. 29: 138-141. Ref.: https://bit.ly/2T86kso




















