Indexing & Abstracting
Full Text
Case ReportDOI Number : 10.36811/ijho.2019.110001Article Views : 2558Article Downloads : 19
Burkitt leukemia with atypical morphology and subsequent therapy-related acute myeloid leukemia
Weijie Li1*, Linda D Cooley1 and Joy Fulbright2
1Department of Pathology and Laboratory Medicine, Missouri, USA
2Division of Hematology/Oncology, Children’s Mercy Hospital, University of Missouri-Kansas City School of Medicine, Missouri, USA
*Corresponding author: Weijie Li, Department of Pathology and Laboratory Medicine, 2401 Gillham Rd., Kansas City, Missouri, USA, 64108, Tel: 816-760-8816; Fax: 816-802-1492; Email: wli@cmh.edu
Article Information
Aritcle Type: Case Report
Citation: Weijie Li, Linda D Cooley, Joy Fulbright. 2018. Burkitt leukemia with atypical morphology and subsequent therapy-related acute myeloid leukemia. Int J Hematol Oncol. 1: 01-03.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2018; Weijie Li
Publication history:
Received date: 10 December, 2018Accepted date: 18 December, 2018
Published date: 19 December, 2018
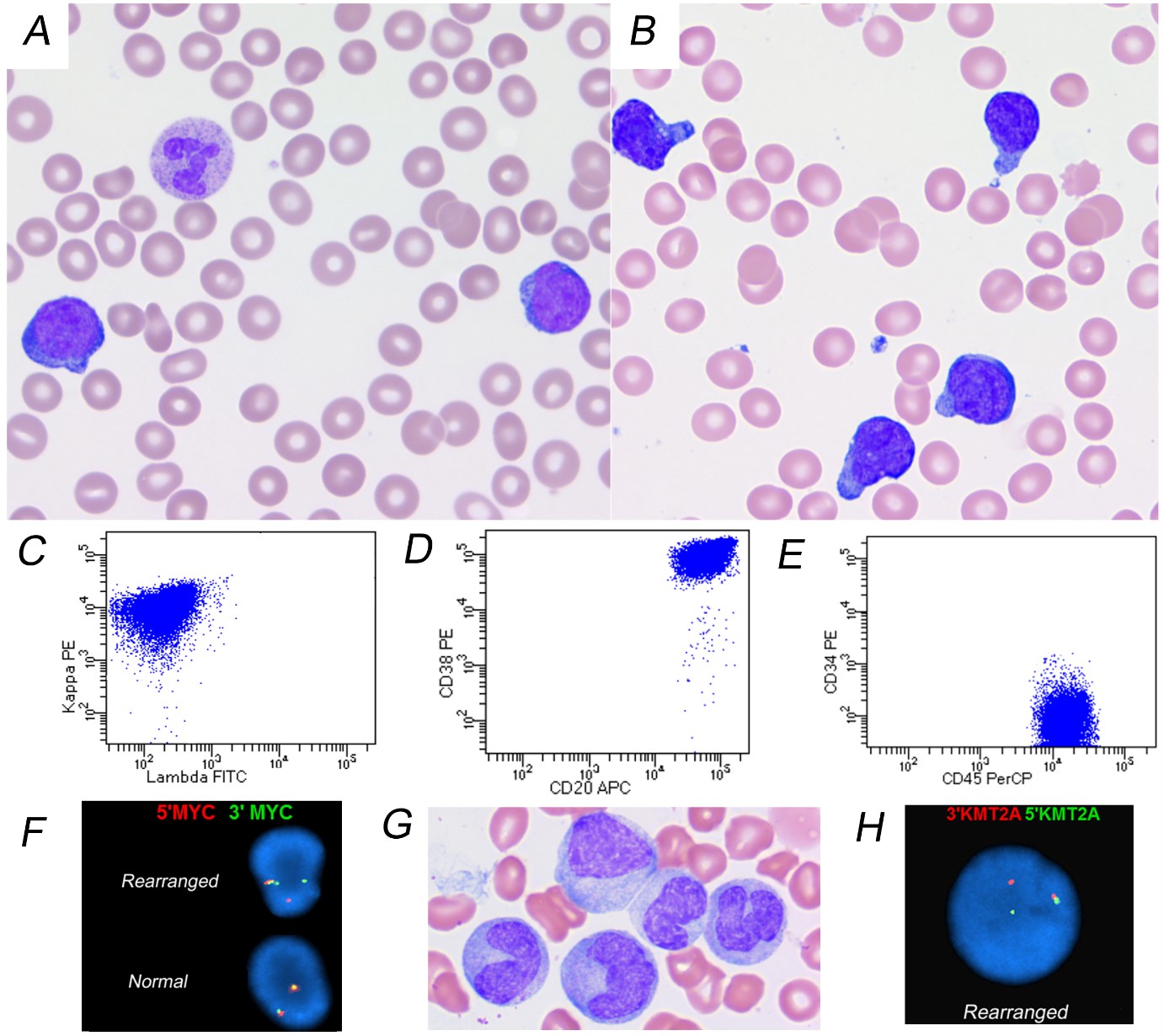
A 10-year-old previous healthy boy presented with jaw pain for several weeks. Compete blood count revealed leukocytosis (WBC 41.08 X 109/L), anemia (Hemoglobin 79 g/L) and thrombocytopenia (platelet count 50 X 109/L). Peripheral blood (PB) and bone marrow (BM) smears (Figure 1, panels A and B) showed frequent small sized blasts with high nucleus-to-cytoplasm ratio, and hand-mirror morphology. Flow cytometry analysis of BM showed 75% blasts with surface kappa-restriction, strongly positive for CD38, CD20, CD45, and negative for CD34 (Figure 1, panels C to E). The blasts were negative for CD10 and TdT. Cytogenetic study showed a complex abnormal karyotype: 46,XY,del(1)(q23),add(3)(q25),t(8;14)(q24.1;q32.3),der(13)t(1;?;13)(q23;?;q13).
FISH analysis confirmed MYC gene rearrangement (Figure 1, panel F). Burkitt leukemia (BL) was diagnosed. Patient underwent chemotherapy per COG ANHL01P1 protocol and achieved complete remission. 17 months after chemotherapy, he developed thrombocytopenia and monocytosis. BM showed many immature or atypical monocytic cells (Figure 1, panel G). Cytogenetic study showed t(11;19)(q23;p13.1). FISH confirmed KMT2A rearrangement (Figure 1, panel H).
BL is an aggressive leukemia responding well to high-intensity, short-duration chemotherapy, which differs from the treatment for precursor B-cell acute lymphoblastic leukemia (B-ALL). Therapy for BL includes high cumulative doses of topoisomerase inhibitors, etoposide and doxorubicin. BL can be separated from B-ALL by its typical FAB L-3 morphology (medium to large in size, uniform, round or oval nuclei with one or more distinct nucleoli, moderate amount of deeply basophilic cytoplasm with prominent vacuoles) [1] and typical mature germinal center B-cell phenotype. However, occasional BL cases show atypical morphology and immunophenotype [2-3]. Without cytogenetic tests, these cases could be misdiagnosed and improperly treated. Therapy-related acute myeloid leukemia (tAML) is the consequence of mutational events induced by cytotoxic therapy with no known predictable factors in most of the patients. tAML with 11q23 (KMT2A) rearrangement is known to occur at a high frequency following chemotherapy including topoisomerase II inhibitors. The tAML associated with topoisomerase therapy has a short latency period, and it commonly shows monocytic differentiation [4,5]. It is not known whether there is an association between the atypical morphology of BL and increased risk for developing tAML after chemotheropy. For any patient with a history of chemotherapy, unexpected cytopenia with monocytosis should raise the alarm for tAML.
Figure 1: A. Peripheral blood smear shows some small blast-like abnormal cells (Wright’s stain, original magnificationx1000). B. Bone marrow (BM) aspirate smear reveals frequent small blasts with hand-mirror morphology (Wright-Giemsa stain, original magnificationx1000). C-E. Flow cytometry analysis of BM shows an abnormal kappa-restricted B-cell population with strong expression of CD20, CD38, CD45 and no expression of CD34. F. FISH analysis reveals MYC gene rearrangement. G. BM smear shows many immature or atypical monocytic cells (Wright-Giemsa stain, original magnificationx1000). H. FISH analysis reveals KMT2A rearrangement.
References
- Van Eys J, Pullen J, Head D, et al. 1986. The French-American-British (FAB) classification of leukemia. The Pediatric Oncology Group experience with lymphocytic leukemia. Cancer. 57:1046-1051. [Ref.]
- Komrokji R, Lancet J, Felgar R, et al. 2003. Burkitt's leukemia with precursor B-cell immunophenotype and atypical morphology (atypical Burkitt's leukemia/lymphoma): case report and review of literature. Leuk Res. 27: 561-566. [Ref.]
- Rawlinson NJ, Baker P, Kahwash SB. 2011. Burkitt's leukemia with an atypical immunophenotype: report of a case and review of literature. Lab Hematol. 17: 27-31. [Ref.]
- Swerdlow S, Campo E, Harris NL, et al. WHO Classification of tumors of Haematopoietic and Lymphoid Tissues. Lyon France: IARC. 2017. [Ref.]
- Balgobind B V, Zwaan CM, Pieters R, et al. 2011. The heterogeneity of pediatric MLL-rearranged acute myeloid leukemia. Leukemia. 25: 1239-1248. [Ref.]




















