Indexing & Abstracting
Full Text
Case ReportDOI Number : 10.36811/ijdsc.2020.110004Article Views : 24Article Downloads : 16
Cutaneous Mastocytosis in a 61-year-old Female from a Dermatological and Histopathological Perspective
Erisa Kola1*, Jorida Memini2, Ina Kola3, John Ekladous4, Daniela Nakuci5, Denisa Cipi6 and Migena Brati Dervishi7
1Pathologist, Department of Pathology and Forensic Medicine, Albania
2Dermatologist, Department of Dermatology, Tirane, Albania
3Department of Plastic Surgery and Burns, Mother Teresa University Hospital Center, Albania
4Department of Pathology, Hackensack Meridian Health, NJ, USA
5Pathologist, Department of Pathology and Forensic Medicine, Albania
6Unit of Environmental Disease, Internal Medicine, Mother Teresa University Hospital Center, Tirane, Albania
7Urgent Care Clinical Trials Complete Health Partners, Nashville, TN, USA
*Corresponding Author: Erisa Kola, Pathologist, Department of Pathology and Forensic Medicine, Albania, Email: erisa_k87@yahoo.com
Article Information
Aritcle Type: Case Report
Citation: Erisa Kola, Jorida Memini, Ina Kola, et al. 2020. Cutaneous Mastocytosis in a 61-year-old Female from a Dermatological and Histopathological Perspective. Int J Dermatol Skin Care. 2: 01-06.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2020; Erisa Kola
Publication history:
Received date: 11 April, 2020Accepted date: 18 April, 2020
Published date: 20 April, 2020
Abstract
First described by Nettleship et al. in 1869 [1], mastocytoses are a heterogeneous group of disorders characterized by the pathologic accumulation of mast cells in various tissues [2-5]. Mastocytosis can be confined to the skin as in cutaneous mastocytosis (CM), or it can involve extracutaneous tissues such as the liver, spleen, bone marrow and lymph nodes, as in systemic mastocytosis [6]. Mastocytosis is a World Health Organization-defined clonal mast cell disorder characterized by significant clinicopathologic heterogeneity [7].
Keywords: Cutaneous mastocytosis; Systemic mastocytosis; Systemic involvement; Mast cells; Mastocytosis.
Introduction
The organ most frequently involved in mastocytosis is the skin. Cutaneous mastocytosis is classified according to clinical presentation and is further defined by onset of disease [8]. Cutaneous mastocytosis tends to appear early in life but adult onset can occur. Over 55% of cases occur in patients under the age of two years, and another 10% of cases appear in patients between the ages of 2 and 15 years [9]. Males and females are affected equally and is most common in whites. Historically, CM was described by Nettleship and Tay in 1869 as a symmetrical maculopapular eruption with urtication of the lesions after rubbing [10]. Mastocytosis is characterized by expansion of clonal mast cells in different organs, often related to KIT mutations [8,11-13]. Whether mastocytosis is a hyperplastic reaction to an unknown stimulus or a neoplastic condition remains unknown. More than 80% of all patients with mastocytosis exhibit characteristic brown-red macular skin lesions [14]. The diagnosis of CM is based on clinical features, histopathologic analysis and the absence of systemic mastocytosis. Darier’s sign, which is defined by whealing and reddening of lesions upon mechanical stroking or rubbing, is a classic diagnostic hallmark of mastocytosis [15,16]. Blistering or bullous mastocytosis represents an exaggerated Darier’s sign, more commonly seen in pediatric patients.
Case presentation
A 61-year-old female presented to the Department of Dermatology with multiple pigmented macules in the chest area, arms and shoulders. Several years ago, it started as few papular elements, distributed in a non-symmetrical order, that appeared initially on the legs. The lesions were accompanied by an itch and general discomfort feeling, especially when she was exposed to heat and during emotional stress. Physical examination revealed numerous red-brown macules measuring 2-3 mm in diameter and a positive Darier’s sign. The rest of the findings were unremarkable and no evidence of systemic mastocytosis was seen.
The following tests were performed:
Abdominal ultrasonography: no hepatosplenomegaly. Several complete blood counts: within normal limits. Liver and renal function tests and lipid profile: within normal limits. Urine analyses: within normal limits. VDRL: negative. X-ray of long bones: unremarkable.
The differential diagnosis included histocytosis, mastocytosis, Grover’s Disease and autoimmune disease. After excision of the skin lesion, the morphologic and immunophenotypic findings were suggestive of CM. Thus, the occurrence of the skin lesion with no initial visceral involvement suggested the diagnosis of primary cutaneous mastocytosis.
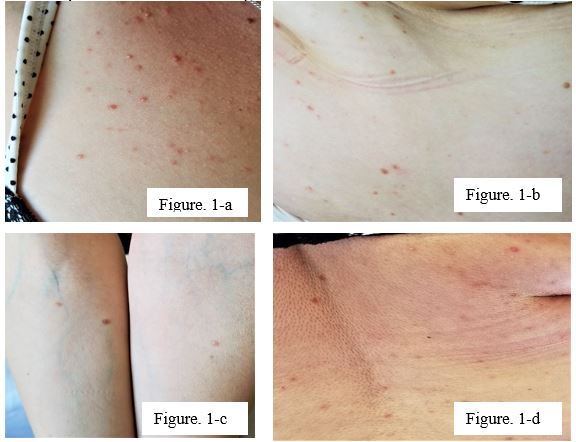
Figure 1 (a-c): Clinical presentation of maculopapular cutaneous mastocytesis with red-brown, ill-defined macules starting from the legs and expanding in random distribution involving the chest area and arms, bilaterally (c). Histopathological examination of the lesion showed a proliferation of spindled mast cells within the superficial dermis. The cells showed a granular eosinophilic to amphophilic cytoplasm and nuclei with dispersed chromatin without significant atypia.
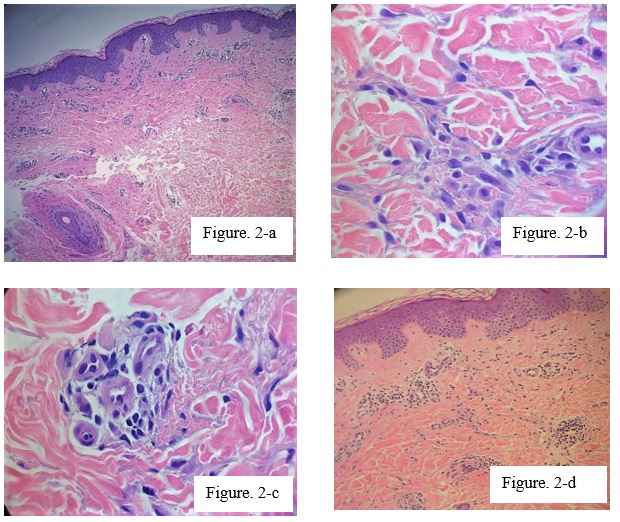
Figure 2: Hematoxylin &eosin-stained sections from skinbiopsy of the patient revealed numerous superficial dermal perivascular mast cells.
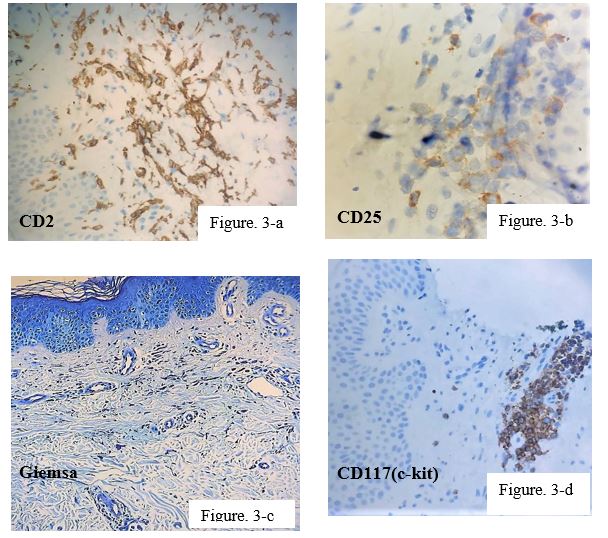
Figure 3: Immunohistochemical and special stains. Neoplastic mast cells show CD117 positivity with aberrant coexpression of CD2 and CD25. Giemsa stain highlights mast cells.
Discussion
Mastocytosis refers to a rare group of disorders characterized by excessive mast cell accumulation and is subdivided into cutaneous and systemic mastocytosis. According to the World Health Organization, cutaneous mastocytosis is classified into (1) urticaria pigmentosa, also known as maculopapular cutaneous mastocyteosis (MPCM); (2) diffuse cutaneous; (3) mastocytoma of the skin and (4) telangiectasia macular is eruptive perstans (TMEP) [17,18]. Union-US consensus group also established criteria for cutaneous involvement in patients with mastocytosis [19]. These criteria include the presence of (1) a typical skin lesion (major criterion), (2) a histologically-confirmed infiltrate of mast cells in the dermis (minor criterion) and (3) KIT mutation at codon 816 in lesional skin (minor criterion). Urticaria pigmentosa, resulting from the accumulation of excessive numbers of mast cells in the skin, is the most common form of cutaneous mastocytosis [20]. The classification of CM has been based on macroscopic features of skin lesions, their distribution and disease onset. Cutaneous mastocytosis typically has a benign course and may spontaneously regress. Commonly reported symptoms of cutaneous mastocytosis are generalized flushing and localized blistering. The laboratory tests performed should be chosen according to the symptoms displayed. The prognosis of patients with cutaneous mastocytosis depends on the existence of systemic involvement and disease onset. A bone marrow examination is recommended in all adult patients suspected of mastocytosis even if the serum tryptase is normal [21].
Conclusion
Cutaneous mastocytosis poses a diagnostic challenge clinically, as it presents with diverse dermatological manifestations and clinical symptoms. Clinicians should be aware of the various subforms and the overlapping features of the lesions with other possible etiologies such as endocrinologic, vasculopathies or immunologic. Assimilation of the clinical presentation, histologic findings and immunohistochemical and molecular studies may help to clarify the diagnosis. A multidisciplinary approach is recommended in the diagnosis and management of patients with mastocytosis. Although much progress has been made in understanding the pathogenesis of the disease and establishing diagnostic criteria and treatment recommendations, mastocytosis still remains a diagnostic challenge for physicians.
References
1. Nettleship J, Tay W. 1869. Rare forms of urticaria. Br Med J. 2: 323-324. Ref.: https://bit.ly/2XGWWOH
2. Parwaresch MR, Horny HP, Lennert K. 1985. Tissue mast cells in health and disease. Pathol Res Pract. 179: 439-461. Ref.: https://bit.ly/3ag8N9f
3. Valent P, Akin C, Sperr WR, et al. 2003. Diagnosis and treatment of systemic mastocytosis: state of the art. Br J Haematol.; 122: 695-717. Ref.: https://bit.ly/3aiO5W2
4. Metcalfe DD. 2008. Mast cells and mastocytosis. Blood. 112: 946-956. Ref.: https://bit.ly/2xFFa3V
5. Horny HP, Parwaresch MR, Lennert K. 1985. Bone marrow findings in systemic mastocytosis. Hum Pathol. 16: 808-814. Ref.: https://bit.ly/2XJMV3y
6. Mariana Castells, Dean D. 2011. Metcalfe and Luis Escribano. Guidelines for the Diagnosis and Treatment of Cutaneous Mastocytosis in Children, Am J Clin Dermatol. 12: 259-270. Ref.: https://bit.ly/2KffFsK
7. Falchi L1, Verstovsek S2. 2018. Kit Mutations: New Insights and Diagnostic Value.Immunol Allergy Clin North Am. 38: 411-428. Ref.: https://bit.ly/3esz5s4
8. Valent P, Horny H-P, Escribano L, et al. 2001. Diagnostic criteria and classification of mastocytosis: a consensus proposal. Leuk Res. 25: 603. Ref.: https://bit.ly/34JJf2W
9. Kettelhut BV, Metcalfe DD. 1991. Pediatric mastocytosis. J Invest Dermatol. 96: 15-18.
10. Nettleship E, Tay W. 1869. Rare forms of urticaria. Br Med J. 2: 323. Ref.: https://bit.ly/2z6MLZz
11. Akin C, Valent P. 2014. Diagnostic criteria and classification of mastocytosis in 2014. Immunol Allergy Clin North Am.34: 207-218. Ref.: https://bit.ly/2VFAcMF
12. Horny HP, Akin C, Metcalfe DD, et al. 2008. Mastocytosis (mast cell disease). In: Swerdlow SH, Campo PE, Harris NL, Jaffe ES, Pileri SA, Stein H, editors. World Health Organization (WHO) classification of tumours pathology and genetics of tumours of the haematopoietic and lymphoid tissues, Vol 2. Lyon (France): IARC Press. 54-63.
13. Theoharides TC, Valent P, Akin C. 2015. Mast cells, mastocytosis, and related disorders. N Engl J Med. 373: 163-72. Ref.: https://bit.ly/3exdSNy
14. Akin C, Metcalfe DD. 2004. Systemic mastocytosis. Annu Rev Med. 55: 419-432. Ref.: https://bit.ly/3bjhgcT
15. Greaves M. 1998. Mastocytoses. In: Champion RH, Burton JL, Burns AD, Breathnach SM (eds). Textbook of Dermatology, Vol. 3, 6th edn.Oxford: Blackwell Science. 2337-2346.
16. Longley BJ. 1999. What dermatologists need to know about mast cell disease: a dermatopathologist’s view. Cutis. 64: 281-282. Ref.: https://bit.ly/3ankawh
17. Horny HP, Akin C, Metcalfe DD, et al. 2008. Mastocytosis (mast cell disease). In: Swerdlow SH, Campo PE, Harris NL, Jaffe ES, Pileri SA, Stein H, editors. World Health Organization (WHO) classification of tumours pathology and genetics of tumours of the haematopoietic and lymphoid tissues, Vol 2. Lyon (France): IARC Press. 54-63.
18. Valent P, Horny HP, Li CY, et al. 2001. Mastocytosis. In: Jaffe ES, Harris NL, Stein H, Vardiman JW, editors. World Health Organization (WHO) classification of tumours pathology and genetics of tumours of the haematopoietic and lymphoid tissues, Vol 1. Lyon (France): IARC Press. 291-302. Ref.: https://bit.ly/3esB6Va
19. Valent P, Akin C, Escribano L, et al. 2007. Standards and standardization in mastocytosis: consensus statements on diagnostics, treatment recommendations and response criteria. Eur J Clin Invest. 37: 435-453. Ref.: https://bit.ly/2Vh8cQv
20. Brockow K1. 2004. Immunol Allergy Clin North Am. 24: 287-316. Ref.: https://bit.ly/2wJjl2O
21. Valent P, Akin C, Arock M, et al. 2012. Butterfield JH et al. Definitions, criteria and global classification of mast cell disorders with special reference to mast cell activation syndromes: a consensus proposal. Int Arch Allergy Immunol. 157: 215-225. Ref.: https://bit.ly/2xBO02z




















