Indexing & Abstracting
Full Text
Case ReportDOI Number : 10.36811/gju.2021.110012Article Views : 147Article Downloads : 96
Lower Urinary tract function following Radical Cystectomy and Orthotopic neobladder Urinary diversion
Abdulbast Darwish1*, Ezaldean AL shibany2, Hael Saeed1, Duyazen Alhosam1, Abdullah Ghamdhan1, Abdualmlk AL Mekhlafy1 and Ali Ahmed Al-Zaazaai2*
1Consultants of urology in Ezaldean AL Shibany Hospital, and the Algomhori Hospital Republic of Yemen, Yemen
2Clinical pharmacy from China and products manager with Al-Jabal groups company in Yemen, Yemen
*Corresponding Author: Abdulbast Darwish, Consultants of urology in Ezaldean AL Shibany Hospital, and the Algomhori Hospital Republic of Yemen, Yemen, Phone: 00967- 771030044; Email: Dr.drwish@gmail.com
Ali Ahmed Al-Zaazaai, Clinical pharmacy from China and products manager with Al-Jabal groups company in Yemen, Yemen, Tel: 00967-771207965; Email: Alzaazaiali@yahoo.com
Article Information
Aritcle Type: Case Report
Citation: Abdulbast Darwish, Ezaldean AL shibany, Hael Saeed, et al. 2021. Lower Urinary tract function following Radical Cystectomy and Orthotopic neobladder Urinary diversion. Glob J Urol. 3: 06-11.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2021; Abdulbast Darwish
Publication history:
Received date: 02 July, 2021Accepted date: 11 July, 2021
Published date: 13 July, 2021
Abstract
The aim of the study: Orthotopic neobladder reconstruction is the preferred method of urinary diversion after radical cystectomy. We evaluated lower urinary tract function outcomes in patients after orthotopic neobladder using a patient questionnaire.
Material and Methods: 40 patients who do radical cystectomy and orthotopic neobladder in EZ Aldean Al-Shi-Bany hospital at Sana'a Yemen between 2010-2018 patients with bladder cancer were included in a clinical trial, randomly assigned to Camey II pouch diversion after radical cystectomy. The patients were mailed a questionnaire 12-24 months after radical cystectomy including items on function, intermittent catheterization, and incontinence.
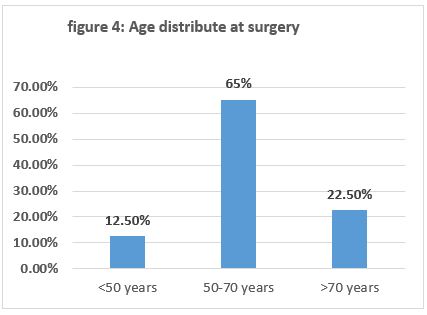
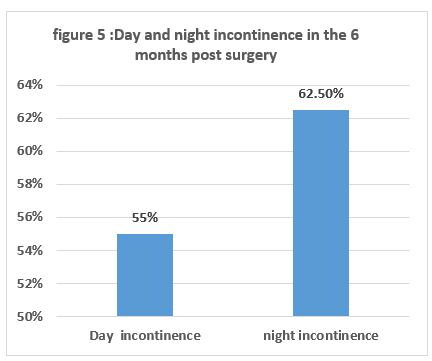
Results: During the study between 2010-2018, 40 neobladder diversion were performed, day incontinence was 55% ((22 cases)) in the first 6 months post-surgery but improved to 12.5% ((5 cases)) after 1-year post-surgery also night incontinence was 62.5% ((25 cases)) in first 6 months postsurgical but improved to 15% ((6 cases)) 1-year post-surgery. Mean age at surgery of 40 patients were sub-segments analysis <50yeas was 12.5 % (5 case), 50-70 years was 65% (26 case), >70 years 22.5% (9 case).
Conclusion: Ileal orthotopic neobladder have good lower urinary tract functional result, daytime and nighttime incomitance is coming in neobladder patients following surgery but improved with time. CIC is less common following surgery and improved with time.
Keywords: Neobladder; Orthotopic; Lower Urinary Tract Function; Incontinence
Introduction
Orthotopic neobladder reconstruction is the preferred method of urinary diversion after radical cyst-prostatectomy by patients and surgeons at our institution [1]. Although a considerable number of patients are appropriate candidates for orthotopic neobladder [2], patients and physicians need to have realistic expectations of the functional outcomes to make an informed decision about diversion type [3]. Fear of urinary incontinence and clean intermittent self-catheterization are reportedly the most common reasons for refusal of the orthotopic neobladder [1]. Daytime and nighttime UI has been reported in 12% and 15% of patients with orthotopic neobladder respectively, and emptying failure occurs in 5% [1,4-6]. However, these results were obtained from retrospective chart review or non-orthotopic neobladder-specific questionnaires [7-10]. The BCI questionnaire was developed as a tool to evaluate patients who underwent cystectomy with different types of diversion [11]. However, this questionnaire lacks detail about the size or wetness of pads, mucus leakage endoscopic view of bladder cancer (Figure 1).
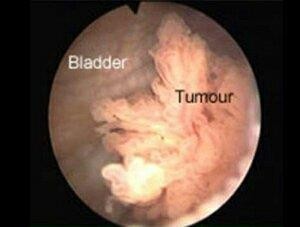
Figure 1: Show endoscopic view of bladder cancer.
Material and Methods
Between 2010-2018, 40 patients did radical cystectomy and diversion in EZ Aldean AL-Shibani hospital at Sana'a Yemen country male: female (6.4:1) received a low-pressure ileal bladder substitute at our hospital due to muscle-invasive bladder cancer following radical cystectomy ((Hysterectomy and oophorectomy in female)) The surgical technique for construction of the ileal bladder substitute is briefly, an ileal segment us to 50 cm (Figure: 2,3). long was isolated approximately 25cm proximal to ileocecal valve length of intestinal segment used for the reservoir was recorded at operation the length of this segment varied during the study period as the optimal size was sought, which was found to be an ileal segment approximately (40 to 44cm) Camey II ileal pouch retro intestinal anastomoses were performed.


Figure 2,3: An ileal segment us to 50cm long was isolated approximately 25cm Proximal to ileocecal valve length of intestinal segment used for the reservoir was recorded at operation the length of this segment varied during the study period as the optimal size was sought.
Follow up patients
All patients were followed in the prospective protocol that included clinical, metabolic, and radiological assessment from the standpoint of oncological follow-up, and lower urinary tract function to assess lower urinary tract function in detail, voiding and continence diaries ((frequency volume chart for ((2-3 days)) and a standardized questionnaire were completed at 12-24 months after surgery and sometimes annually thereafter The questionnaire. Assessed presence and degree of urinary incontinence and using bad or not day and night. The long-term follow up protocol ((more than 1 a year)) included assessment of urine status with urine culture blood pressure, laboratory study, ultrasound of the kidney post voiding residual volume continence was defined as complete dryness or loss of no more than a few drops of urine once or twice a month. All data were prospectively entered into the department database. Method, Definition, and units conform to the standards recommended by the international continence society. Statistics were performed with a commercially available software package.
Result
40 patients underwent radical cystectomy with neobladder diversion from 2010-2018 about 82.5% (33case male) and 17.5% (7 case female), age at surgery of 40 patients were subsequently analyzed less than 50 years was 5 cases ((12.5%)), between 50-70 years was 26 cases ((65%)) figure 4.
Daytime incontinence 6 months following surgery was 55% (22 cases) but decreased to about 12.5% (5 cases) after 1-year nighttime incontinence was 62.5 % (25 case) after 6 months following surgery but decreased to 15% (6 cases) Figure 5,6.

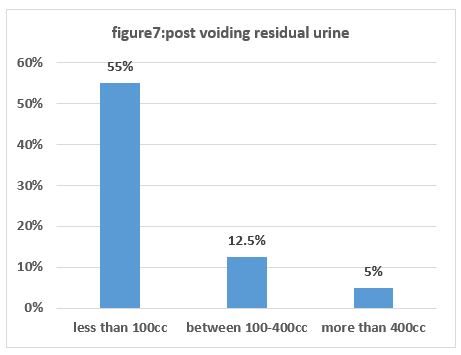
Post voiding Residual urine was after 6 months analysis less than 100cc was 55% ((22 cases)) and between 100-400cc was 12.5 ((5 cases)) more than 400cc was 5% ((2 cases)) figure 7.
No clear difference between males and females for continence. CIC was done in 12.5% (5 cases) following surgery but improved to 5% (2 cases) after one year following surgery.
Discussion
An orthotopic neobladder is an established urinary diversion option for patients who require radical cystectomy improved quality of life following orthotopic neobladder compared to alternative forms of diversion fails to be realized when voiding dysfunction arises. Therefore, detailed knowledge of the long-term functional outcome is of the important success of orthotopic bladder substitution to store urine and thus, providing urinary continence relies on sufficient functional reservoir capacity, detubulavization of an intestinal segment to reduce intravesical pressure, and preservation of external urethral sphincter tonus. Daytime and nighttime incontinence in neobladder patients is common following surgery but improved over time. In the present study, daytime continence rates average 55% at 6 months but improved to 12.5% at 1year. In our study permanent failure to empty the 2.5% bladder substitute was not a major problem as only two patients required catheterization after 1 year.
Conclusion
These clinical cases come to more reliable and confident that was orthotopic neobladder was the preferred method for lower urinary tract reconstruction. Following a radical cystectomy, voiding frequency and officious micturition remain stable for more than years. Day and night incontinence improved with time.
Authors’ Contribution
Abdulbast Darwish1, Ezaldean AL shibany 2, Hael Saeed, Duyazen ALhosam, Abdullah Ghamdhan, Abdualmlk AL mekhlafy; study concept and design, data achievement, interpretation; manuscript enrolling, study supervision, the idea of the manuscript, writing and literature review. Dr. Ali Ahmed Al-Zaazaai: revision of the manuscript for important intellectual content, and publication.
Conflict of Interests
The authors declared that there were no conflicts of interest get up in the process of this study.
Acknowledgment
We acknowledgment all responsibilities the authors would like to thank Professor Xiao Jian and Dr. Ali Ahmed Al-Zaazaai M.Sc. clinical pharmacy from Wenzhou University, Wenzhou Zhejiang province PR China who helped to arranging this paper for publication. The research team thanks all patients for their co-operation.
Funding
This research received a specific grant from Dr. Abdulbast Darwish, Ezaldean AL Shibany.
Abbreviations
CIC: Clean Intermittent Catheterization
UI: Urege incontinence
References
1. Ashley MS, Daneshmand S. 2010. Factors influencing the choice of urinary diversion in patients undergoing radical cystectomy. BJU Int. 106: 654. Ref.: https://pubmed.ncbi.nlm.nih.gov/20089108/ DOI: https://doi.org/10.1111/j.1464-410x.2009.09183.x
2. Hautmann RE. 2000. Which patients with transitional cell carcinoma of the bladder or prostatic urethra are candidates for an orthotopic neobladder? CurrUrol Rep. 1: 173.
3. Daneshmand S, Bartsch G. 2011. Improving selection of appropriate urinary diversion following radical cystectomy for bladder cancer. Expert Rev Anticancer Ther. 11: 941. Ref.: https://pubmed.ncbi.nlm.nih.gov/21707291/ DOI: https://doi.org/10.1586/era.11.19
4. Hollowell CM, Christiano AP, Steinberg GD. 2000. Technique of Hautmann ileal neobladder with chimney modification: interim results in 50patients. J Urol. 163: 47. Ref.: https://pubmed.ncbi.nlm.nih.gov/10604311/
5. Granberg CF, Boorjian SA, Crispen PL, et al. 2008. Functional and oncological outcomes after orthotopic neobladder reconstruction in women. BJU Int. 102: 1551. Ref.: https://pubmed.ncbi.nlm.nih.gov/18990170/ DOI: https://doi.org/10.1111/j.1464-410x.2008.07909.x
6. Elmajian DA, Stein JP, Esrig D, et al. 1996. The Kockileal neobladder: updated experience in 295 male patients. J Urol. 156: 920. Ref.: https://pubmed.ncbi.nlm.nih.gov/8709364/ DOI: https://doi.org/10.1016/s0022-5347(01)65663-5
7. Stein JP, Dunn MD, Quek ML, et al. 2004. The orthotopic T pouch ileal neobladder: experience with 209 patients. J Urol. 172: 584. Ref.: https://pubmed.ncbi.nlm.nih.gov/15247737/ DOI: https://doi.org/10.1097/01.ju.0000131651.77048.73
8. Hautmann RE, de Petriconi R, Gottfried HW, et al. 1999. The ileal neobladder: complications and functional results in 363 patients after 11 years of followup. J Urol. 161: 422. Ref.: https://pubmed.ncbi.nlm.nih.gov/9915417/ DOI: https://doi.org/10.1016/s0022-5347(01)61909-8
9. Studer UE, Burkhard FC, Schumacher M, et al. 2006. Twenty years' experience with an ileal orthotopic low pressure bladder substitute–lessons to belearned. J Urol. 176: 161. Ref.: https://pubmed.ncbi.nlm.nih.gov/16753394/ DOI: https://doi.org/10.1016/s0022-5347(06)00573-8
10. Gilbert SM, Wood DP, Dunn RL, et al. 2007. Measuring health-related quality of life outcomes in bladder cancer patients using the Bladder Cancer Index(BCI). Cancer. 109: 1756. Ref.: https://pubmed.ncbi.nlm.nih.gov/17366596/ DOI: https://doi.org/10.1002/cncr.22556
11. Gilbert SM, Dunn RL, Hollenbeck BK, et al. 2010. Development and validation of the Bladder Cancer Index: a comprehensive, disease specific measure of health related quality of life in patients with localized bladder cancer. J Urol. 183: 1764. Ref.: https://pubmed.ncbi.nlm.nih.gov/20299056/ DOI: https://doi.org/10.1016/j.juro.2010.01.013




















