Indexing & Abstracting
Full Text
Case BlogDOI Number : 10.36811/gju.2020.110009Article Views : 9Article Downloads : 8
Nightmare of urologist: Forgotten DJ stent (case series)
Manjeet Kumar1*, Kirti Rana2, Sanjeev Chauhan2, Girish Kumar3 and Kailash Barwal3
1Assistant Professor, Department of Urology, IGMC Shimla
2Senior Resident, Department of Urology, IGMC Shimla
3Associate Professor, Department of Urology, IGMC Shimla
*Corresponding Author: Manjeet Kumar, Assistant Professor, Department of Urology, IGMC Shimla, Email: dr.vicky.surgeon@gmail.com
Article Information
Aritcle Type: Case Blog
Citation: Manjeet Kumar, Kirti Rana, Sanjeev Chauhan, et al. 2020. Nightmare of urologist: Forgotten DJ stent (case series). Glob J Urol. 2: 11-16.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2020; Manjeet Kumar
Publication history:
Received date: 14 February, 2020Accepted date: 27 February, 2020
Published date: 28 February, 2020
Abstract
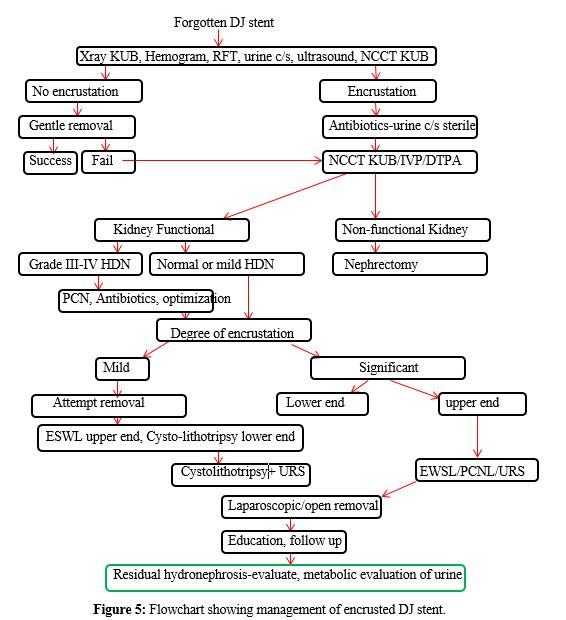
DJ stent is a routine procedure performed by a urologist. DJ stents are forgotten when instructions are not given properly, illiteracy, ignorance, increased patient load in the clinic. Forgotten DJ stent associated with complications i.e., recurrent urinary tract infections, stone formation, fragmentation, migration, obstructive uropathy, hematuria, deterioration in renal function, urosepsis. Management of these forgotten DJ stents depends upon complications. Antibiotics manage encrusted DJ stents, ESWL or PCNL for the upper end, cystolithotripsy or cystolithotripsy, ureteroscopy for lower end. We describe the management of forgotten DJ stents in 3 patients.
Introduction
The double DJ stent is the most common procedure performed by a urologist. The Ideal DJ stent is easy to insert, has excellent flow characteristics, is resistant to infection and encrustation, is chemically stable after insertion in a urinary environment, can relieve obstruction (intraluminal and extraluminal), and is associated with minimum symptoms. Thus, the ideal stent should, therefore, have high tensile strength, a low friction coefficient, memory, and a self-retainment mechanism and should be biocompatible and affordable. The frequent use of DJ stent leads to complications associated with its use. The most dreaded nightmare for a urologist would be forgotten DJ stent. The reason behind it is complications associated with forgotten DJ stent carry significant medico-legal implications [1].
The complications associated with forgotten DJ stent are
1. The encrustation of DJ stent
2. Obstruction to urine flow
3. Stent fracture
4. Impaction of DJ stent
5. Erosion of DJ stent
We describe our experience of management of forgotten DJ stents in three patients. Patients underwent routine investigations, hemgram, urea, creatinine, urine c/s, and ultrasound, x ray KUB, NCCTKUB. Patients were started on antibiotics, antispasmodics, tamsulosin 0.4 mg. On rendering patient urine c/s sterile, patients were planned for procedures. After stent removal patient were followed on 7th postoperative day with X ray KUB, ultrasound abdomen. Patient were educated regarding Dj stent and urolithiasis. After stent and stone free, urine for metabolic evaluation was done at 1 month after intervention.
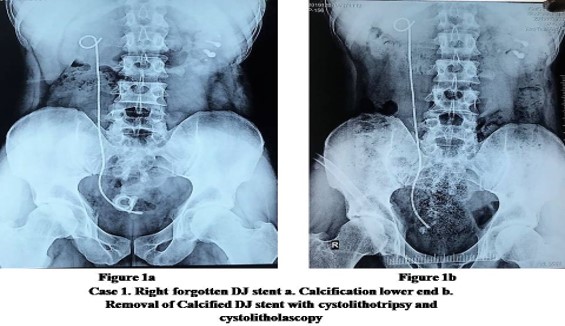
Case 1: A 55 years old male presented with dysuria, pain lower abdomen, and low-grade fever. Ultrasound suggests right DJ stent in situ, x-ray KUB showed Right calcified DJ stent with the encrusted lower end. X-ray also showed left renal stone. The patient gives a history of right PCNL with DJ stenting two years back. On blood investigations Hb 11.5, TLC 5600/mm3, Ur/cr 20/1.1, Urine c/s E coli sensitive to aminoglycosides. The patient was started on antibiotics. Patient was operated under spinal anaesthesia. Cystolithotripsy with cystolitholapexy was done with removal of lower end of DJ stent. In the second surgery, ureteroscopy with 8.5 Fr diameters with pneumatic lithotripsy of calcified DJ stent was done. DJ stent was removed during ureteroscopy. Postoperatively the patient was planned for left PCNL (Figure 1,2).

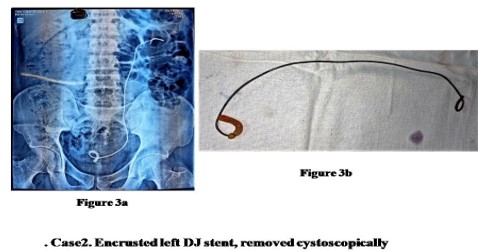
Case 2: A 35 years female presented with flank pain with low-grade fever. The patient underwent blood investigations, X-ray KUB, and ultrasound. The patient has anaemia (Hb 7.5 gm%), leucocyte count 11500/mm3, Urine c/s- E coli sensitive to ciprofloxacin. X-ray KUB suggestive of calcified left DJ stent. Ultrasound suggestive left hydronephrosis with calcified upper and lower end of forgotten stent varies. (Figure 2) Patient was taken to operating room for DJ stent removal. Under spinal anaesthesia, gentle attempt for stent removal was made. DJ stent removal was successful figure 3 (a,b).
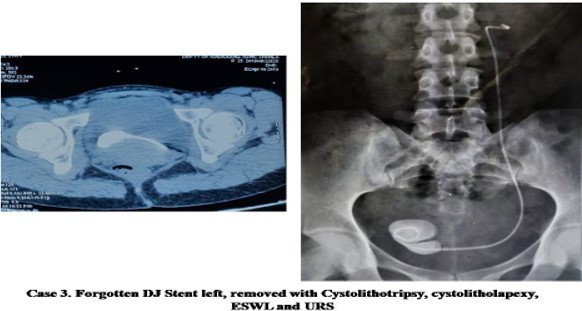
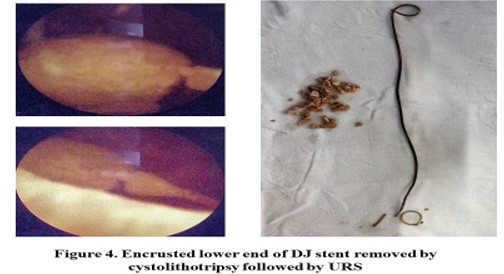
Case 3: A 39 years male presented with pain lower abdomen, with intermittent hematuria, with the frequency of urination. On investigations Hb 10.5, TLC 9900, urea 35, creatinine 1.0, urine c/s klebsiella sensitive to aminoglycosides. Patient was started on antibiotics and planned for surgery. Ultrasound and x-ray KUB suggest stone at the lower end of DJ stent with calcification of whole DJ stent. Non-contrast CT scan was done. Blood investigations showed Hb 9.9, TLC 9900/mm3, Ur/Cr 30/0.8. Patient underwent cystolithotripsy with removal of encrusted lower end with stone. Ureteroscopy with fragmentation of encrusted DJ stent had done till upper ureter figure 4.
Discussion
Management of complicated stents requires coordinated use of the latest in medical, lithotripsy, and endourologic techniques, or open surgery. Degradation of stent polymers and hardening of polyethylene and polyurethane can lead to fragmentation if a stent is left in place longer than 6 months. Encrustation of ureteral stents is often associated with alkaline urine and UTI, with struvite and calcium phosphate deposits predominating. Andriole et al reported a 10% incidence of stent obstruction secondary to encrustation in a series of 87 patients in whom the indication for stent placement was predominantly noncalculous disease. [2] Damiano et al. observed flank pain in 25.3%, encrustations in 21.6%, irritative bladder symptoms in 18.8%, hematuria in 18.1%, UTI in 12.3%, and stent migration in 9.5% of the patients.13 Stent syndrome that comprises flank pain, suprapubic discomfort, irritative voiding symptoms, and occasional hematuria is common among our study populations. [3] Lupu et al described SWL as the noninvasive procedure of choice for calcified ureteral stents. [4] SWL successfully fragmented calcifications on the renal end and ureteral segment of the stent, but electrohydraulic lithotripsy was necessary to fragment calcification on the bladder end. Smet et al successfully fragmented calcifications on both ends of a ureteral stent by applying SWL to the bladder end of the stent, with the patient in a prone position, followed by SWL to the renal end, with the patient in a supine position. [5] To prevent this situation, patients should be reminded of the presence of an internal stent that could lead to problems if left indwelling for a prolonged period of time. Moreover, a computerized registry of stent placement may be used to alert the urologist when the stent must be removed. A study by el- Faqih et al. states “the stent encrustation rate increases from 9.2% for an indwelling time of less than six weeks to 47.5% for six to 12 weeks and 76.3% for more than 12 weeks.” [6] DJ stent is double edge sword, although used frequently but not always justified. Judicious use is advised along with through counselling of patient and attendants regarding need, timely removal and complications. [7] Prevention is the best management that can be attained with patient counselling, data recording and tracking. Study has reported the decline of incidence of forgotten stent from 12.5% to 1.2% with the use of computer-based tracking software. [8] We have denileated our management of encrusted DJ stent in flowchart mentioned in figure 5.
Conclusion
DJ stent use is very common in urological practice. Proper counselling at discharge and follow up should be done. Patient are educated regarding further management, follow up and DJ stent removal. Patients with forgotten DJ stents should be managed as per protocol described.
References
1. RP Finney. 1978. Experience with new double J ureteral catheter stent. J Urol. 120: 678-681. Ref.: https://bit.ly/3cbTn7X
2. Andriole GL, Bettmann MA, Garnick MB, et al. 1984. Indwelling Double-J ureteral stents for temporary and permanent urinary drainage: experience with 87 patients. J Urol. 131: 239-241. Ref.: https://bit.ly/2Vthklo
3. Damiano R, Autorino R, Esposito C, et al. 2004. Stent positioning after ureteroscopy for urinary calculi: The question is still open. Eur Urol. 46: 381-388. Ref.: https://bit.ly/2Pu2Tdb
4. Lupu AN, Fuchs GJ, Chaussy CG. 1986. Calcification of ureteral stent treated by extracorporeal shock wave lithotripsy. J Urol. 136: 1297-1298. Ref.: https://bit.ly/2Vs1SWQ
5. Smet G, Vandeursen H, Baert L. 1991. Extracorporeal shock wave lithotripsy for calcified ureteral catheter. Urol Int. 46: 211-212. Ref.: https://bit.ly/2VpyP5Z
6. El-Faqih SR, Shamsuddin AB, Chakrabarti A, et al. 1991. Polyurethane internal ureteral stents in treatment of stone patients: morbidity related to indwelling times. The Journal of urology. 146:1487-1491. Ref.: https://bit.ly/3acFXXQ
7. Kumar M. 2019. Double J stent: double edged sword. Cli Med Cas Rep Stu: CMCRS-116. Ref.: https://bit.ly/2wdgCOo
8. Lawrentschuk N, Russell JM. 2004. Ureteric stenting 25 years on: routine or risky? ANZ J Surg.74: 243-247. Ref.: https://bit.ly/3a6yOYT




















