Indexing & Abstracting
Full Text
Case ReportDOI Number : 10.36811/cjo.2022.110005Article Views : 2Article Downloads : 0
Total section of the Humeral artery during a fall on a sharp part of a mirror: Case Report
Redha Lakehal*, Farid Aymer, Soumaya Bendjaballah, Rabah Daoud, Khaled Khacha, Baya Aziza and Abdelmalek Bouzid
Faculty of Medicine Constantine 03, Constantine, Algeria
*Corresponding Author: Redha Lakehal, Department of Heart Surgery, Ehs Dr Djaghri Mokhtar, Constantine, Algeria; Email: lakehal.redha@gmail.com
Article Information
Aritcle Type: Case Report
Citation: Redha Lakehal, Farid Aymer, Soumaya Bendjaballah, et al. 2022. Total section of the Humeral artery during a fall on a sharp part of a mirror: Case Report. Clin J Orthop. 4: 01-03.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2022; Redha Lakehal
Publication history:
Received date: 18 January, 2022Accepted date: 31 January, 2022
Published date: 02 February, 2022
Introduction
Pediatric vascular trauma is rare and comprises only approximately 0.6% to 2% of all traumatic pediatric injuries [1]. The most common mechanisms include motor vehicle accidents, firearm injuries, stab wounds, and falls. The most commonly injured vessels include those of the upper extremity, followed in decreasing frequency by abdominal trauma (Inferior vena cava, iliac and renal vessels), lower extremity, chest, and neck vessels [2,3]. Compared to adult vascular trauma, pediatric vascular injury is more likely to be asymptomatic and is associated with vasospasm. Therefore, consideration of minor signs is essential. Minor signs require other diagnostic explorations such as Doppler ultrasound and/or CT angiography. Major signs warrant rapid intervention; these include persistent shock despite adequate resuscitation, active bleeding, rapidly expanding hematoma, decreased peripheral pulses, and proximity of wound trajectory to major vessels and/or signs of nerve damage, arteriovenous fistula or distal ischemia (pallor, absence of pulse, paresthesia and pain) [4,5]. The purpose of this work is to show a domestic accident in a child such as total section of the humeral artery by the sharp part of a mirror.
Observation
We report the observation of a 08-year-old girl victim of a fall on a sharp part of a mirror without bone lesion of the forearm with abolition of the left radial pulse without sensorimotor disorders for more than 24 hours. The physical examination revealed abolition of the right radial pulse with coldness and pallor of the hand and forearm without sensorimotor deficit of the latter two as well as a deep skin wound of the right arm. The chest X-ray showed a CTI at 0.50. Electrocardiogram showed regular sinus rhythm. The patient was placed under general endotracheal anesthesia in the supine position. The intraoperative exploration found a loss of right humeral arterial substance of 03 cm with retracted and thrombosed ends without lesions of the median nerve and without associated venous lesion. The procedure consisted of restoring right humeral arterial continuity via the saphenous vein after preparation of the humeral arterial extremities with immobilization of the right upper limb with a plaster splint (Figures 1,2).
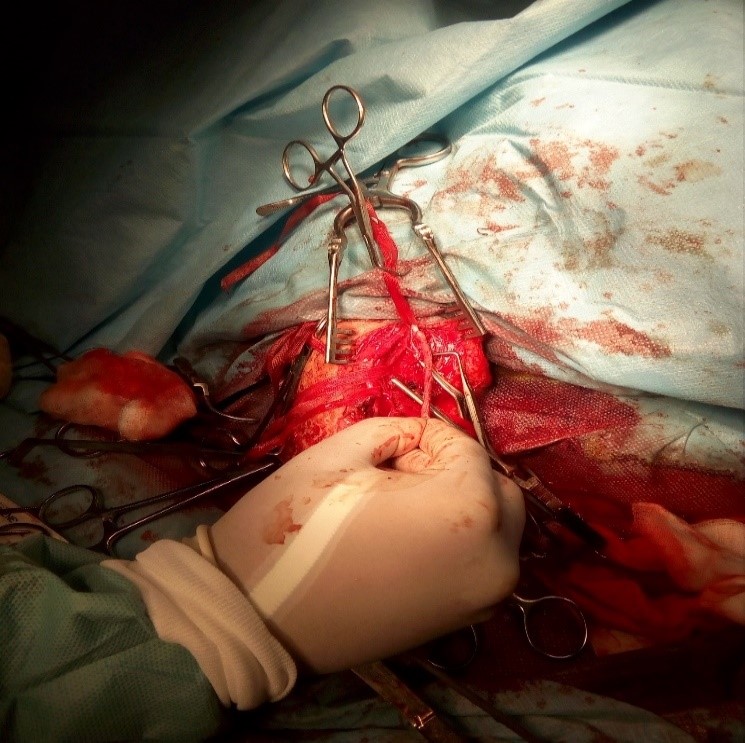
Figure 1: Intraoperative image.

Figure 2: Intraoperative image after arterial reconstitution.
Results
The postoperative follow-up was favorable in terms of revascularization of the upper limb. Stay in intensive care unit was 01 day. The immediate and medium-term postoperative follow-ups were favorable in terms of vitality and vascularization. Control CT angiography of the traumatized limb performed 6 months postoperatively showed a permeable graft without anastomotic stenosis.
Discussions
Traumatic non-iatrogenic vascular injuries in children are rare and rarely discussed in literature. Pediatric vascular injuries pose a set of challenges mainly because of continued growth and development in a child or adolescent [1-3]. Although less common than in adults, a significant proportion was due to penetrating injuries. The upper limb vessels were the most frequently injured and were associated with low mortality. Lesions of the thoracic aorta are rare [4]. Blunt vascular injuries in the lower extremities occur most commonly in the anteroposterior tibial arteries; injured arteries in the proximal upper and lower extremity require resection with interposition grafting, whereas those in the forearm or calf are usually ligated [5]. The appropriate treatment of pediatric patients with acute arterial lesions of the limbs requires early surgery and continuous postoperative follow-up during the growing years. The loss of humeral arterial substance was filled by a vascular substitute: Saphenous vein in our patient. If chronic arterial insufficiency is observed, arteriograms should be performed and arterial reconstruction should be undertaken [6]. Despite the multidisciplinary diagnostic and treatment modalities available in pediatric trauma centers, traumatic vascular injury in children and adolescents is associated with significant morbidity and mortality in contemporary surgical practice [7] but lower than in adults [4]. However, contemporary perioperative and long-term outcomes after surgical revascularization are excellent, as demonstrated by the series published by Wang SK and colleagues [8].
Conclusion
Non-iatrogenic pediatric vascular trauma is uncommon. Penetrating mechanism is more common than blunt and extremities are more frequently affected. The exploration of the humeral artery must be systematic after open dislocation of the elbow. The presence of a lesion of a vessel must be suspected and explored in front of an opening on the path of a vascular axis. The treatment is adapted to the vascular lesions and possibly to the associated lesions. It is conventional or endovascular surgery. The urgency of its implementation depends on the intensity of the hemorrhagic shock or the downstream ischemic repercussions. Overall complications come from associated injuries to tendons and nerves. Walkman's syndrome can even occur postoperatively.
References
1. Heinzerling NP, Sato TT. 2014. Pediatric Vascular Injuries. In: Dua A, Desai SS, Holcomb JB, Burgess AR, Freischlag JA, eds. Clinical Review of Vascular Trauma.
2. Branco BC, Naik MB, Montero BM. 2017. Increasing use of endovascular therapy in pediatric arterial trauma. 66: 1175-1183. Ref.: https://pubmed.ncbi.nlm.nih.gov/28756045/ DOI: https://doi.org/10.1016/j.jvs.2017.04.072
3. Morão S, Ferreira RS, Camacho N. 2018. Vascular Trauma in Children-Review from a Major Paediatric Center. Ann Vasc Surg. 49: 229-233. Ref.: https://pubmed.ncbi.nlm.nih.gov/29428539/ DOI: https://doi.org/10.1016/j.avsg.2017.10.036
4. Barmparas G, Inaba K, Talving P. 2010. Pediatric vs adult vascular trauma: a National Trauma Databank review. J Pediatr Surg. 45: 1404-1412. Ref.: https://pubmed.ncbi.nlm.nih.gov/20638516/ DOI: https://doi.org/10.1016/j.jpedsurg.2009.09.017
5. Rozycki GS, Tremblay LN, Feliciano DV. 2003. Blunt vascular trauma in the extremity: diagnosis, management, and outcome. J Trauma. 55: 814-824. Ref.: https://pubmed.ncbi.nlm.nih.gov/14608150/ DOI: https://doi.org/10.1097/01.ta.0000087807.44105.ae
6. Whitehouse WM, Coran AG, Stanley JC. 1976. Pediatric Vascular Trauma: Manifestations, Management, and Sequelae of Extremity Arterial Injury in Patients Undergoing Surgical Treatment. Arch Surg. 111: 1269-1275. Ref.: https://pubmed.ncbi.nlm.nih.gov/985076/ DOI: https://doi.org/10.1001/archsurg.1976.01360290103016
7. Klinkner DB, Arca MJ, Lewis BD. 2007. Pediatric vascular injuries: patterns of injury, morbidity, and mortality. J Pediatr Surg. 42: 178-182. Ref.: https://pubmed.ncbi.nlm.nih.gov/17208561/ DOI: https://doi.org/10.1016/j.jpedsurg.2006.09.016
8. Wang SK, Drucker NA, Raymond JL. 2019. Long-term outcomes after pediatric peripheral revascularization secondary to trauma at an urban level I center. J Vasc Surg. 69: 857-862. Ref.: https://pubmed.ncbi.nlm.nih.gov/30292605/ DOI: https://doi.org/10.1016/j.jvs.2018.07.029




















